Abstract
Hepaticojejunostomy is an important part of many surgical procedures including pancreaticoduodenectomy. Biliary leakage from hepaticojejunostomy may be associated with intraabdominal abscess formation, biliary peritonitis, and even mortality. A 72-year-old female patient was admitted to our hospital with obstructive jaundice. After initial evaluation, she was diagnosed with distal common bile duct obstruction without accurate diagnosis. Before planned pancreaticoduodenectomy, biliary drainage with a T-tube was performed due to the presence of cholangitis. After the first operation, pancreaticoduodenectomy was performed. Postinflammatory changes around the hilar region made the hepaticojejunostomy risky. A bilio-digestive anastomosis was performed using a new technique. A nasogastric tube was placed into the common bile duct proximal to the anastomosis. The postoperative course of the patient was uneventful. The use of a nasogastric tube as a stent in risky hepaticojejunostomies is a simple technique that can be beneficial.
Pancreaticoduodenectomy (PD) is one of the most complex surgical procedures in gastrointestinal surgery. With advances in diagnostic imaging and surgical techniques, the mortality rate of PD has decreased from 20% to 2% in high volume centers.1 Leakage from pancreaticojejunostomy anastomosis is the most significant cause of postoperative morbidity and mortality. However, hepaticojejunostomy is also an important part of the surgical procedure for PD. Any bile leak from hepaticojejunostomy anastomosis may cause morbidity through the occurence of bile peritonitis and intraabdominal abscess. Many surgical techniques have been investigated in relation to securing anastomosis in hepaticojejunostomy. This report focuses on the placement of a nasogastric tube into the common bile duct, a surgical technique that allows safe hepaticojejunostomy for PD.
A 72-year-old female patient was admitted to our hospital with complaints of jaundice. She had lost 8 kg within the last month. The performance status of the patient was poor. Her physical examination was normal except for jaundice. At the time of admission, the laboratory evaluation revealed alkaline phosphatase 314 IU/L (reference: 50-150); gamma-glutamyltransferase 512 IU/L (reference: 9-36); and CEA and CA 19-9 levels were normal. Abdominal magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatography (MRCP) showed a distal bile duct obstruction with dilation of the common bile duct and intrahepatic bile ducts (Figs. 1, 2). Endoscopic retrograde cholangiopancreatography (ERCP) was performed due to an increase in bilirubin levels, and a plastic stent was placed into the common bile duct for endoscopic retrograde biliary drainange (ERBD). With a preliminary diagnosis of distal bile duct tumor, the patient was prepared for PD.
During this period, fever (38.6°C), an increased biluribin level of 11.06 mg/dl (reference: 0.2-1.2) and a C-reactive protein (CRP) level of 14.25 mg/dl was detected. Due to a legal holiday, the interventional radiology unit was not working, and thus percutaneous biliary drainage and repeat ERCP could not be performed. The patient was operated on in emergency conditions. During exploration, a dilated common bile duct was found, which was 2 cm in diameter. Choledochotomy was then performed. As there was infected bile inside the common bile duct, the bile duct was washed out with isotonic solution. A plastic stent was found inside the common bile duct and removed. A T-Tube was inserted for biliary drainage. Her postoperative course was uneventful. A cholangiogram was performed on the 10th postoperative day, from which it was found that there was total obstruction in the distal bile duct.
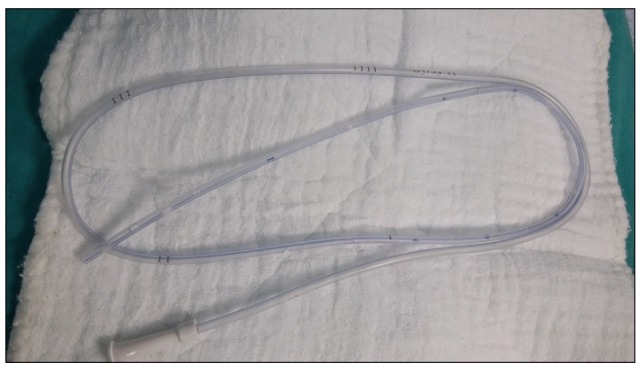
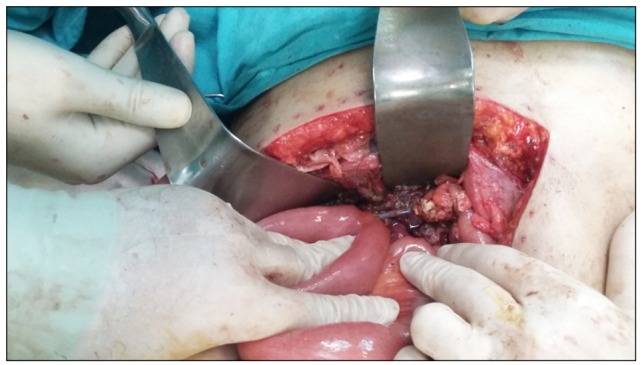
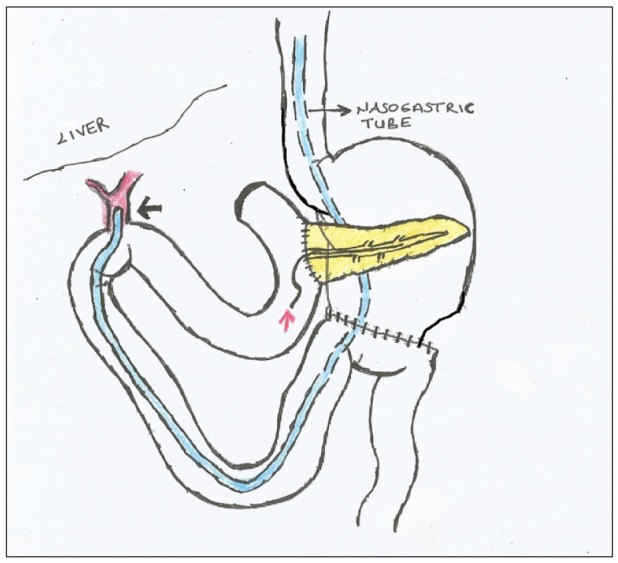
The patient was decided to undergo operation again on the 16th postoperative day. The abdomen was opened with a subcostal incision as performed previously. There were firm adhesions around the T-tube and hilar region. These adhesions were dissected. The head of the pancreas was firm and enlarged without an obvious mass lesion, and thus pancreatic cancer was suspected. The common bile duct was prepared for anastomosis and PD was finally performed. Due to the occurrence of inflammatory changes, hepaticojejunostomy anastomosis is estimated to be a risky anastomosis. A 12-Fr nasogastric tube with additional holes was prepared and it was passed from the stomach and jejenum and placed into the common bile duct (Figs. 3, 4, 5, 6). Hepaticojejunostomy anastomosis was performed in a one-layer fashion with 4/0 polydioxanone (PDS) sutures. Pancreaticojejunal anastomosis was performed in an end-to-side fashion with a catheter inside the pancreatic channel. The postoperative period was uneventful. There were no bile or pancreatic leaks during the postoperative period. The pathological examination of the surgical specimen revealed a pancreatic mass of 1.5×2 cm in diameter.
The first PD was performed in 1909 and popularized by an American surgeon, Allen Whipple. Although the mortality rates for PD have decreased, morbidity rates remain relatively high. PD has morbidity rates between 25% and 65%.234 Hepaticojejunostomy is an important part of many surgical procedures including PD, liver transplantation, and palliative treatment of unresectable pancreaticobiliary tumors. The risk of bile leaks after pancreatic head resection varies between 2% and 12%.56 Biliary leakage may be associated with intraabdominal abscess formation, biliary peritonitis, prolonged hospital stay, and mortality.
Due to the development of percutaneous techniques, most patients with anastomotic leakage can be managed without surgery. There are many studies that have investigated pancreaticojejunostomy anastomosis in PD. However, there are few studies relating to hepaticojejunostomy. Hepaticojejunostomy leaks are the second most common type of leak, after pancreaticojejunostomy leaks. Although hepaticojejunostomy anastomosis is not a technically difficult anastomosis to perform, it can provide a challenging problem in patients with a small diameter bile duct or postinflammatory conditions. The use of a transanastomotic biliary stent is a well-known technique for difficult hepaticojejunostomy. The placed stent can be internal or external. Herzog et al.7 investigated the role of T-tube placement into the anastomotic region in patients with difficult hepaticojejunostomy. There were 114 patients, of which 55 of them were managed with T-tube placement and 59 were not. Biliary leakage was detected in 5 patients (9%) with a T-tube and 9 patients (15%) without a T-tube. Seven percent (8/114) of patients required revisional laparotomy, 2% [1/55] of those with a T-tube and 12% [7/59] without a T-tube. There were no differences in terms of mortality. It was concluded that hepaticojejunostomy with T-tube placement cannot prevent biliary leakage but can reduce the severity of bile leaks, reducing the need for reoperation.7
Suzuki et al.8 compared hepaticojejunostomies with stenting or without stenting. They concluded that the routine use of a biliary stent in hepaticojejunostomy is not justified. Yoshida et al.9 used silicon drains for hepaticojejunostomy. In patients with hepatic hilar malignancies, they found that a 10-Fr silicon drain with channels is superior to a 5-Fr silicon drain with an internal lumen for internal biliary stenting for hepaticojejunostomy. Yoshimi et al.10 performed internal stenting for hepaticojejunostomy and pancreaticojejunostomy in 11 patients with pancreaticoduodenectomy, in which there were only 4 minor leaks during the postoperative period.
In our case, we used a 12-Fr nasogastric tube to secure hepaticojejunostomy anastomosis. Our patient was operated on due to cholangitis before PD. There were postinflammatory changes around the common bile duct in the second operation. A nasogastric tube was placed into the common bile duct. The nasogastric tube was active in the postoperative period and drained approximately 500-600 ml bile per day. There was no bile leakage at postoperative follow-up.
In conclusion, nasogastric biliary drainage can be beneficial for risky hepaticojejunostomies. The design of a prospective clinical trial with this technique should be encouraged.
References
1. Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg. 2006; 10:1199–1210. PMID: 17114007.

2. Yeo CJ. The Whipple procedure in the 1990s. Adv Surg. 1999; 32:271–303. PMID: 9891749.
3. Grobmyer SR, Pieracci FM, Allen PJ, Brennan MF, Jaques DP. Defining morbidity after pancreaticoduodenectomy: use of a prospective complication grading system. J Am Coll Surg. 2007; 204:356–364. PMID: 17324768.

4. Balcom JH 4th, Rattner DW, Warshaw AL, Chang Y, Fernandez-del Castillo C. Ten-year experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch Surg. 2001; 136:391–398. PMID: 11296108.
5. de Castro SM, Kuhlmann KF, Busch OR, van Delden OM, Laméris JS, van Gulik TM, et al. Incidence and management of biliary leakage after hepaticojejunostomy. J Gastrointest Surg. 2005; 9:1163–1171. PMID: 16269388.
6. Antolovic D, Koch M, Galindo L, Wolff S, Music E, Kienle P, et al. Hepaticojejunostomy--analysis of risk factors for postoperative bile leaks and surgical complications. J Gastrointest Surg. 2007; 11:555–561. PMID: 17394045.

7. Herzog T, Belyaev O, Bakowski P, Chromik AM, Janot M, Suelberg D, et al. The difficult hepaticojejunostomy after pancreatic head resection: reconstruction with a T tube. Am J Surg. 2013; 206:578–585. PMID: 23906984.

8. Suzuki H, Shimura T, Mochhida Y, Wada S, Araki K, Kubo N, et al. To stent or not to stent hepaticojejunostomy--analysis of risk factors for postoperative bile leaks and surgical complication. Hepatogastroenterology. 2014; 61:920–926. PMID: 26158142.
9. Yoshida H, Mamada Y, Taniai N, Mizuguchi Y, Kakinuma D, Ishikawa Y, et al. Silicon drain with channels along the sides for internal biliary stenting of hepaticojejunostomy in hepatic hilar malignancies. J Gastroenterol Hepatol. 2009; 24:752–756. PMID: 19646017.

10. Yoshimi F, Ono H, Asato Y, Ohta T, Koizumi S, Amemiya R, et al. Internal stenting of the hepaticojejunostomy and pancreaticojejunostomy in patients undergoing pancreatoduodenectomy to promote earlier discharge from hospital. Surg Today. 1996; 26:665–667. PMID: 8855507.

Fig. 1
Magnetic resonance imaging of the coronal section of the upper abdomen showing distal bile duct obstruction.
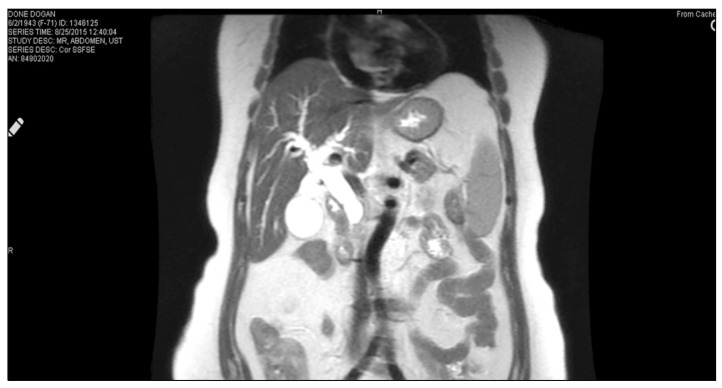
Fig. 2
Magnetic resonance cholangiopancreatography showing dlatation of the common bile duct and intrahepatic bile duct.

Fig. 3
A 12-Fr nasogastric tube used for nasobiliary drainage in hepaticojejunostomy anastomosis. Additional side holes were also added for gastric drainage.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download