Abstract
A hepatic lymphangioma is a rare benign neoplasm that is usually associated with systemic lymphangiomatosis. A solitary hepatic lymphangioma is extremely rare. Therefore, we present a rare case of a female patient who underwent right hepatectomy for solitary giant hepatic lymphangioma. A 42-year-old female presented to the emergency department with complaint of severe abdominal pain of the right upper quadrant. Abdominal computed tomography showed an approximately 23×30-cm sized, giant, relatively well-defined, homogenous cystic mass with few septa in the right liver (segments VII and VIII). The preoperative diagnosis was a giant hepatic cystadenoma or cystadenocarcinoma. We performed right hepatectomy. The permanent histopathological report revealed cystic lymphangioma of the liver. Although the prognosis of solitary hepatic lymphangioma after surgical resection is favorable, recurrence has been reported in literature.
A hepatic lymphangioma is a rare benign neoplasm characterized by cystic dilatation of the lymphatic vessels in the hepatic parenchyma, and usually occurs as part of systemic lymphangiomatosis.1 A solitary hepatic lymphangioma is extremely rare in adult patients.12 The prognosis for hepatic lymphangioma is good and patients have no need for further treatment after surgical resection. We present here a rare case of a female patient who underwent right hepatectomy for solitary giant hepatic lymphangioma.
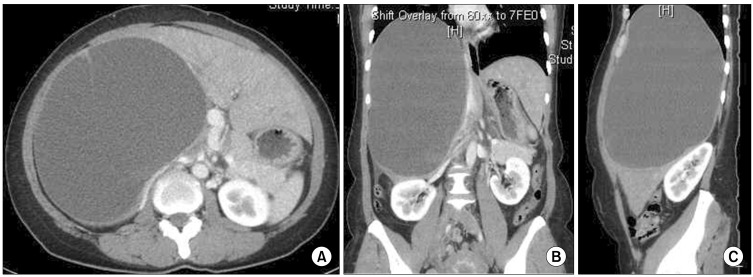
A 42-year-old female presented to the emergency department with a complaint of severe abdominal pain of the right upper quadrant for 1 day. She had no history of abdominal surgery or other medical history. A physical examination revealed a huge, palpable mass occupying the right region of the abdomen. Ultrasonography revealed a hemorrhagic complicated giant cystic mass with septation and multifocal hyperchoic solid components in the right liver (Fig. 1). Abdominal computed tomography (CT) revealed a giant and relatively well-defined homogenous cystic mass of size 23×30 cm, with few septa occupying the segment VII and VIII of the liver and extending from the diaphragm to the right iliac crest (Fig. 2A-C). Hematologic results were within normal ranges as follows: a white blood cell count of 6,660/mm3 (segmental neutrophil 81.4%), hemoglobin level of 13.3 g/dl, hematocrit of 38.9%, platelet count of 384,000/mm3, total protein level of 6.1 g/dl, albumin level of 4.2 g/dl, total bilirubin level of 0.71 mg/dl, aspirate aminotransferase level of 32 IU/L, alanine aminotransferase level of 38 IU/L, and prothrombin time (INR) of 1.09. Serologic tumor markers such as carcinoembryonic antigen (CEA: 1.22 U/ml) and carbohydrate antigen 19-9 (CA19-9: 0.6 U/ml) were normal. ICG15 was 15.6% and elevated. The preoperative diagnosis was a giant hepatic cystadenoma or cystadenocarcinoma.
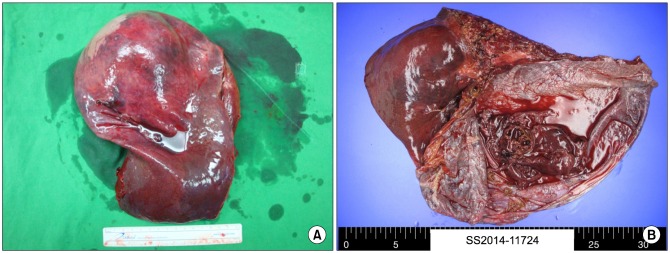
At laparotomy, a giant cystic tense mass was found at the right two segments of the liver (segments VII and VIII), accompanied with minimal spillage of old bloody fluid through the small tearing of a thinned cystic wall. We aspirated about 3,500 ml volume of cystic fluid to improve the working space and to manipulate the cyst, by which the cyst was decompressed. The patient then underwent right hepatectomy. The cystic fluid levels of CEA and CA 19-9 were 0.54 and 0.6 U/ml, respectively. Gross pathology revealed a mass of around 23×30 cm in size with a unilocular cyst and a pinkish white smooth inner surface, which was filled with a coffee-like fluid and sludge (Fig. 3A, B). On microscopic examination, the cyst wall was lined with single-layered flat endothelial cells (Fig. 4A). Immunohistochemical staining revealed that these endothelial-lined cells are positive for CD31, but negative for hepatocytes, CK19 and CK20 (Fig. 4B).
These findings confirmed the diagnosis of a solitary cystic hepatic lymphangioma. Postoperatively, the patient had an uneventful recovery. She was discharged on postoperative day 10 and has been followed up for 18 months without evidence of recurrence.
Lymphangiomas are generally considered to be congenital malformations of the lymphatic system, and they occur mostly in the neck, mediastinum and retroperitoneum; they are seldom found in the liver.123456
Most hepatic lymphangiomas usually have a non-specific clinical presentation such as vague abdominal pain or mass of the affected side.1234 The major complaints were related to the compression of surrounding structures by the large lesion. In our case, the patient suffered from sudden pain in the right abdomen, which is considered to be a localized peritoneal sign of cystic fluid leakage from the tumor.
Although the typical ultrasonography or computed tomography feature of hepatic lymphangioma is a cystic or multicystic hepatic mass with internal septations, the accurate preoperative diagnosis of hepatic lymphangioma is difficult because the these findings can be confused with other cystic tumors such as bile duct cysts, and biliary cystadenomas and cystadenocarcinomas.78 Although we could not perform magnetic resonance imaging in our hospital, it may also help with the diagnosis of lymphangioma, and usually shows a multi-lobulated heterogeneous mass with low signal intensity on T1-weighted images and high signal intensity on T2-weighted images.8
The accurate diagnosis was made by pathological examination. Histologically, lymphangiomas are classified into three subtypes according to the congenital dilated lymphatic channels: capillary (super-microcystic), cavernous (microcystic), or cystic (macrocystic).56 The histogical findings of the hepatic lymphoma are similar to those of other intra-abdominal lymphangiomas. Hepatic lymphangiomas are characterized by cystic dilatation of the lymphatic vessels in the hepatic parenchyma filled with lymph fluid, and are unilocular or multilocular in appearance.1234 The diagnosis in our case was ultimately found to be the cystic type. The histological features of cystic lymphangiomas include the following: flat endothelial lining of the cyst rather than cuboidal epithelium; lymphoid aggregates in the cyst wall; and smooth muscle in the cyst wall.5 In addition to these histological characteristics, the endothelial lining cells usually react positively with CD31 or factor VIII-related antigen, but negatively with cytokeratin on immunohistochemical staining.5 In our case, the immunochemistry with CD31 was used for the detection of endothelial cells of the hepatic lymphangioma and supported its diagnosis.
In contrast to hepatic lymphangiomas, biliary cystadenomas usually demonstrate pathological features such as a cyst with a single lining of cuboidal to columnar epithelium supported by thick fibro-connective tissue and papillary foldings into the cyst. Furthermore, biliary cystadenocarcinoma is identified by the presence of proliferating cytologically malignant epithelium.
The standard treatment for hepatic lymphangioma is complete surgical resection since incomplete excision may often lead to a recurrence.4 Liver transplantation is also considered in patients with an unresectable giant hepatic lymphangioma or poor hepatic function.9 The prognosis following complete resection is excellent.
Although the prognosis of a solitary hepatic lymphangioma is favorable after surgical resection, we recommend that the patient should undergo follow-up because of the possibility of recurrence.
References
1. Stavropoulos M, Vagianos C, Scopa CD, Dragotis C, Androulakis J. Solitary hepatic lymphangioma. A rare benign tumour: a case report. HPB Surg. 1994; 8:33–36. PMID: 7993862.
2. Huang L, Li J, Zhou F, Yan J, Liu C, Zhou AY, et al. Giant cystic lymphangioma of the liver. Hepatol Int. 2010; 4:784–787. PMID: 21286352.

3. Zhang YZ, Ye YS, Tian L, Li W. Rare case of a solitary huge hepatic cystic lymphangioma. World J Clin Cases. 2013; 1:152–154. PMID: 24303489.

4. Liu Q, Sui CJ, Li BS, Gao A, Lu JY, Yang JM. Solitary hepatic lymphangioma: a one-case report. Springerplus. 2014; 3:314. PMID: 25279280.

5. Chung JH, Suh YL, Park IA, Jang JJ, Chi JG, Kim YI, et al. A pathologic study of abdominal lymphangiomas. J Korean Med Sci. 1999; 14:257–262. PMID: 10402167.

6. Roisman I, Manny J, Fields S, Shiloni E. Intra-abdominal lymphangioma. Br J Surg. 1989; 76:485–489. PMID: 2660949.

7. Vargas-Serrano B, Alegre-Bernal N, Cortina-Moreno B, Rodriguez-Romero R, Sanchez-Ortega F. Abdominal cystic lymphangiomas: US and CT findings. Eur J Radiol. 1995; 19:183–187. PMID: 7601168.

8. Choi WJ, Jeong WK, Kim Y, Kim J, Pyo JY, Oh YH. MR imaging of hepatic lymphangioma. Korean J Hepatol. 2012; 18:101–104. PMID: 22511911.

9. Tepetes K, Selby R, Webb M, Madariaga JR, Iwatsuki S, Starzl TE. Orthotopic liver transplantation for benign hepatic neoplasms. Arch Surg. 1995; 130:153–156. PMID: 7848084.

Fig. 1
Abdominal ultrasonography shows a hemorrhagic complicated giant cystic mass with septation and multifocal hyperechoic solid components in the right liver.

Fig. 2
Abdominal computed tomography images show a giant and relatively well-defined homogenous cystic mass of size 23×30 cm occupying segment VII and VIII of the liver and extending from the diaphragm to the right iliac crest (A-C).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download