Abstract
Backgrounds/Aims
The aim of this study was to describe clinical and biological changes in a group of patients who underwent pancreaticoduodenectomy (PD) without any complication during the postoperative period. These changes reflect the "natural history" of PD, and a deviation should be considered as a warning sign.
Methods
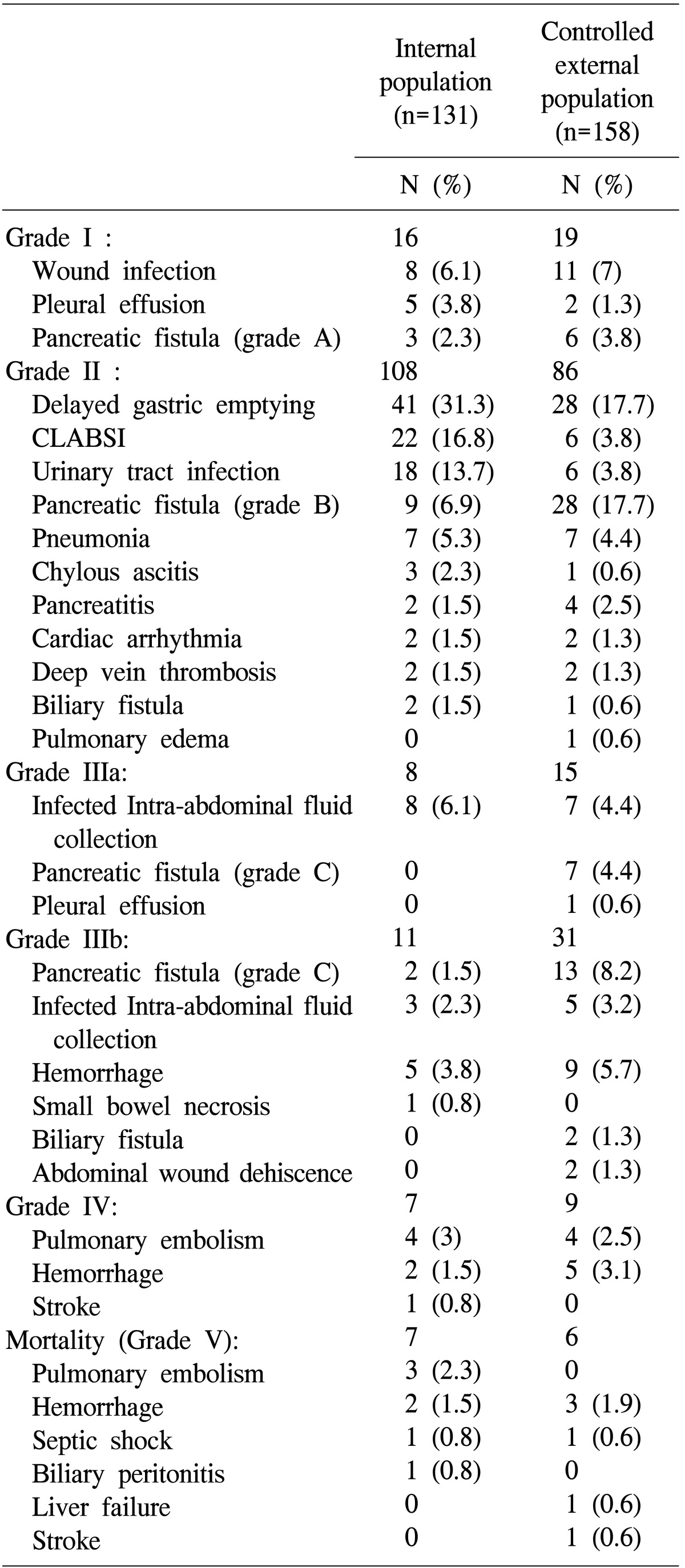
Between January 2000 and December 2009, 131 patients underwent PD. We prospectively collected and retrospectively analyzed demographic data, pathological variables, associated pathological conditions, and preoperative, intraoperative, and postoperative variables. Postoperative variables were validated using an external prospective database of 158 patients.
Results
The mean postoperative length of hospital stay was 20.3±4 days. The mean number of days until removal of nasogastric tube was 6.3±1.6 days. The maximal fall in hemoglobin level occurred on day 3 and began to increase after postoperative day (POD) 5, in patients with or without transfusions. The white blood cell count increased on POD 1 and persisted until POD 7. There was a marked rise in aminotransferase levels at POD 3. The peak was significantly higher in patients with hepatic pedicle occlusion (866±236 IU/L versus 146±48 IU/L; p<0.001). For both γ-glutamyl transpeptidase and alkaline phosphatase, there was a fall on POD1, which persisted until POD 5, followed with a stabilization. Bilirubin decreased progressively from POD 1 onwards.
In 1935, Whipple et al.1 reported 3 patients with ampullary cancer treated by a 2-stage pancreaticoduodenectomy (PD). During the 1940s, PD became a 1-stage procedure and was performed more frequently. In the 1970s, the average mortality rate was 25% and some authors suggested that it should be discontinued.23
In the 1990s, PD was performed with a very low mortality rate of <4% or with no mortality in some series.45 A better selection of patients, improvements in the surgical technique and perioperative care contributed to the improved mortality rate. Although the death rate was reduced, rate of associated complications remained at approximately 50%, and that of pancreatic fistulas at 15%. A complete assessment of clinical and biological changes after PD is required for the early detection of such complications, in order to improve their management.
The aim of this study was to describe clinical and biological changes in a group of patients who underwent PD without any complications during the postoperative period. The results were controled with an external prospective multicentric database. In this study, the changes reflected the "natural history" of PD, hence, a deviation should be considered a warning sign.
All consecutive patients who were candidates for elective PD in our department between January 2000 and December 2009 were considered eligible for the present study. Data for these patients were prospectively recorded and retrospectively analyzed. Exclusion criteria were age of 17 years or younger, and an uneventful postoperative course over the first 30 days.
PD was performed without pylorus preservation. In all patients, PD was performed with an antrectomy and reconstruction with a serosa to mucosa hand-sewn end-to-side pancreaticogastrostomy, with non-absorbable monofilament sutures, on the posterior wall of the gastric body. In case of small wirsung (<3 mm) or/and soft pancreas, an external catheter with multiple side holes was inserted into the pancreatic duct. The largest sized stent that could be passed into the pancreatic duct was used. To prevent migration, the stent was secured to the pancreatic parenchyma with two 6-0 absorbable sutures. The stent was brought out through the gastric wall. The stent was externalized through a stab incision in the anterior abdominal wall and connected to a reservoir (urine bag). Gastrojejunostomy and hepaticojejunostomy were performed on the same jejunal loop, which was brought through the transverse mesocolon in a retrocolic position. Lymphadenectomy was routinely performed with skeletonization of the hepatic artery from the hepatic pedicle to the celiac axis, and removal of the retroportal pancreatic lamina on the right aspect of the superior mesenteric artery.6 No lymphadenectomy was performed in patients with proven benign disease. Two round silicone closed-suction drains were placed in the vicinity of the pancreatic and biliary anastomosis. This drain was removed progressively from postoperative day 7.
Octreotide (Sandostatine®, Novartis, Rueil-Malmaison, France; 100 microgrammes 3 times a day) was administered for 7 days only to patients with a soft pancreatic remnant as pancreatic fistula (PF) prophylaxis. Patients with a fibrotic or hard pancreas did not receive octreotide.7 Since September 2002, all patients received prophylactic erythromycin (200 mg intravenously 4 times per day).89 A thromboembolic prophylaxis with a low-molecular weight heparin was systematically performed even in patients who had PD with associated vascular resection. In accordance with the French consensus,10 all patients received antibiotic prophylaxis (Cefazolin 2 g, intravenously) following induction of anesthesia. Antibiotic therapy was repeated every 4 hours during the operative procedure. Since January 2002, a nasojejunal feeding tube (ENTRAL™ Fr 09-120 cm – Teleflex Medical – France) was placed at the end of the operation. In these patients, enteral feeding was started on postoperative day (POD) 1 after surgery with 500 ml of water. This was progressively increased to 1,000 ml or 1,500 ml of a standardized elemental diet on POD 2 to day 5. Oral diet was initiated 5 to 7 days after the operation if there was no pancreatic fistula or other intra-abdominal complication.
Patients were seen daily by an independent physician until hospital discharge. Demographic data, pathological variables, associated pathological conditions, preoperative risk factors, and operative variables were recorded. Biological parameters (i.e., prothrombin time and levels of bilirubin, liver transaminases, gamma glutamyl transpeptidase, and alkaline phosphatase) were measured on POD 1, 3, 5, 7 and 10. Patients were monitored for postoperative complications, mortality, postoperative course and length of postoperative hospital stay. Peripancreatic drainage fluids were collected and measured and amylase was dosed on POD 1, 3, 5 and 7.
Chest radiography was performed routinely on POD 3 and 7. Abdominal computed tomography with intravenous contrast were also carried out POD 7.11
Mortality and morbidity were defined as death or complications respectively, occurring either within 30 days following surgery or during hospital stay. Complications were stratified in accordance with Dindo's classification.12
Wound infection was defined as the presence of pus requiring wound opening. Infected intra-abdominal fluid collection was defined as postoperative fluid collection treated by puncture or drainage with positive cultures.
Pneumonia was defined in accordance with the American Thoracic Society as a constellation of suggestive clinical features, a demonstrable infiltrate by chest radiography or another imaging technique, with or without supporting microbiological data.13 Hospital-acquired pneumonia is an acute lower respiratory tract infection acquired after at least 48 hours of hospital admission and not incubating at the time of admission.1415 Central line-associated bloodstream infection (CLBSI) was defined as a primary bloodstream infection (BSI) in a patient who had a central line within the 48-hour period before the BSI development. Sepsis was defined as a systemic inflammatory response syndrome (SIRS) with a positive blood culture. Urinary tract infection was defined as a positive urine culture with a colony count ≥105 and ≥10,000 leukocytes per ml.
PF was defined, according to the international study group,16 as an amylase-rich fluid (amylase concentration 3 times superior than serum concentration) collected via needle aspiration of an intra-abdominal collection or from the drainage placed intraoperatively from day 3. PF were graded according to the clinical impact on the patient's hospital course (grades A, B, C). Delayed gastric emptying (DGE) was defined as the inability to resume oral feeding after the first postoperative week or prolonged use of a nasogastric aspiration tube.17 Hemorrhage was defined according to the time of onset, site of bleeding, severity, and clinical impact.18
The controlled group was established from a prospective multicentric randomized study including elective PD between January 2006 and March 2009.19 The protocol was approved by the local ethics committee (Comité Consultatif de Protection des Personnes dans la Recherche Biomédicale, No. 2004/22, Angers, France). Informed consent was obtained from each patient before they entered the study. The surgical technique, perioperative management, and data collection were the same as for the studied population.
Values were expressed as means±standard deviations (SD). Statistical analysis was performed using the assistance of the SPSS software (version 10.0 SPSS, Inc., Chicago, IL). Continuous variables were analyzed by means of a Student t-test or a Mann-Whitney test as appropriate. Multiple comparisons of continuous variables were performed with an ANOVA test. A difference was considered statistically significant when p<0.05.
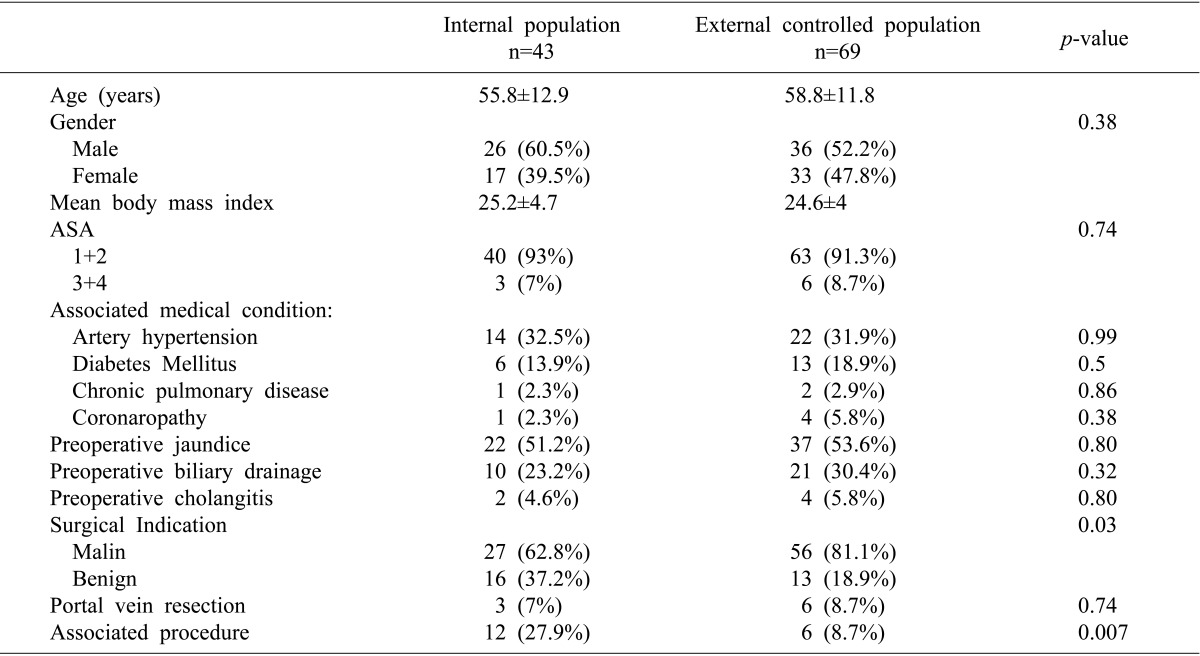
Between January 2000 and December 2009, 131 patients underwent PD. Eighty-eight patients (67.2%) had ≥ 1 postoperative complications (Table 1). Eleven patients (8.4%) required re-operation. The mortality rate was 5.3% (n=7). Causes of death were pulmonary embolism (n=3), hemorrhage (n=2), septic shock (n=1), and biliary peritonitis (n=1). We studied the 43 patients who did not have postoperative complications. The mean findings were summarized in the Table 2.
There were 26 men (60.5%) and 17 women (39.5%) with a mean age of 55.8±12.9 years [range: 33-74]. Sixteen patients (37.2%) were operated on for a benign disease: cystic dystrophy in heterotopic pancreas (n=6), chronic pancreatitis (n=5), cyst lesion (n=2), intraductal papillary and mucinous neoplasm (n=1), benign ampulloma (n=1), and arteriovenous malformation (n=1). Twenty-seven patients (62.8%) were operated on for a malignant disease: pancreatic adenocarcinoma (n=22), distal cholangiocarcinoma (n=1), neuroendocrine tumor (n=2), duodenal carcinoma (n=1), and ampullary cancer (n=1). Ten patients (23.2%) had a preoperative biliary drainage for a mean duration of 14±6.8 days.
Mean operation time was 351±55 minutes and mean intraoperative blood loss was 758±682 ml. Twenty-one patients (48.8%) required transfusion with a mean of 1.9±1.6 units of packed red blood cells. Twelve patients (27.9%) underwent other types of resection: hepatic biopsy (n=4), colectomy (n=2), hepatic resection (n=2), jejunostomy (n=2), ovariectomy (n=1), and splenectomy (n=1). Three patients (7%) underwent PD with associated portal vein resection.
Between January 2006 and March 2009, 158 patients underwent PD.19 Eighty-nine patients (56.3%) had ≥1 postoperative complications (Table 1). Six patients (3.8%) died after surgery, from hemorrhage (n=3), stroke (n=1), hepatic ischemia (n=1), and septic shock (n=1).
The controlled population included 69 patients who did not have postoperative complications and were comparable with the internal group (Table 2). Mean operative time was 381±104 minutes and mean intraoperative blood loss was 684±616 ml. Fourteen patients (20.3%) required transfusion with a mean of 2.8±1.9 units of packed red blood cells. Six patients (8.7%) underwent associated procedures: colectomy (n=2), hepatic resection with portal vein ligature (n=1), enterotomy (n=1), small bowel resection (n=1), and nephrectomy (n=1). Six patients (8.7%) underwent PD with associated portal vein resection and 41 (59.4%) benefited from an external pancreatic duct stent placement.
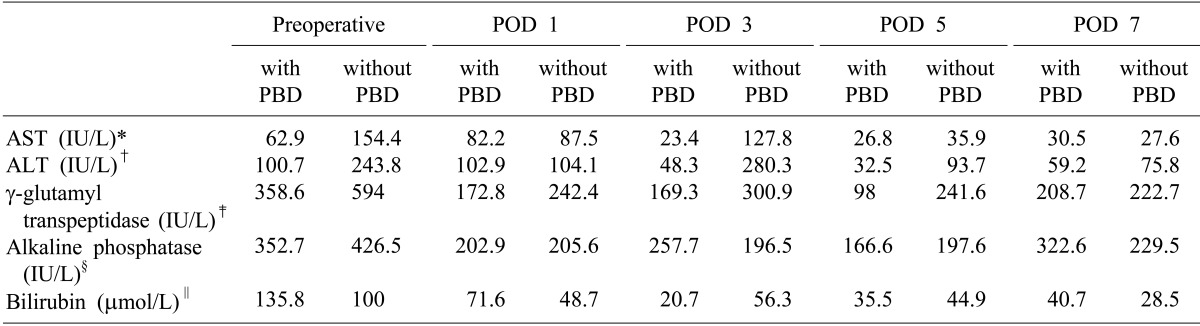
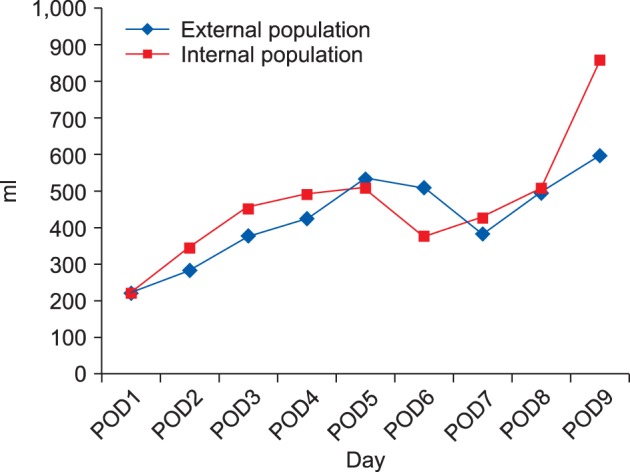
Mean postoperative length of hospital stay was 20.3±4 days. Mean number of days until nasogastric tube (NGT) removal was 6.3±1.6 days. Mean daily output was shown on Fig. 1. Mean number of days until removal of abdominal drains was 9.8±2 days. Mean daily output was shown in Fig. 2. Thirty-four patients (79.1%) received octreotide for a mean of 9.3±3.4 days. Ten patients (23.2%) received erythromycin for a mean of 10.6±4.5 days.
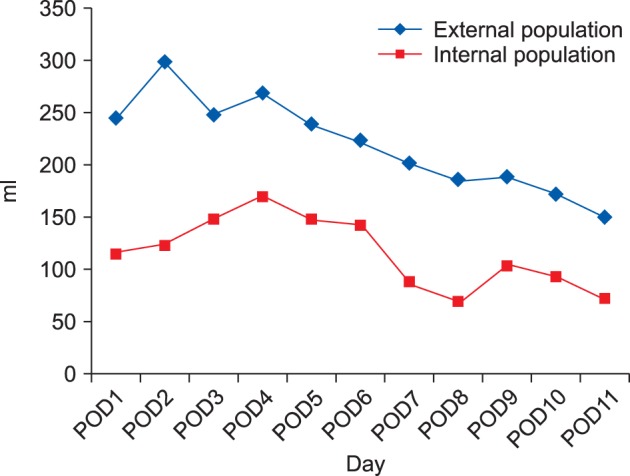
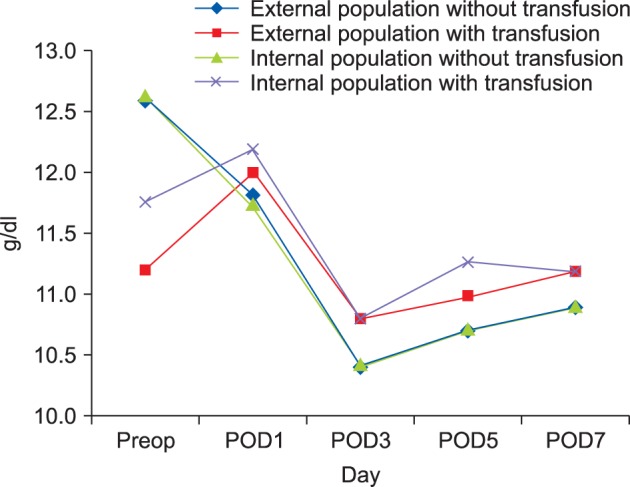
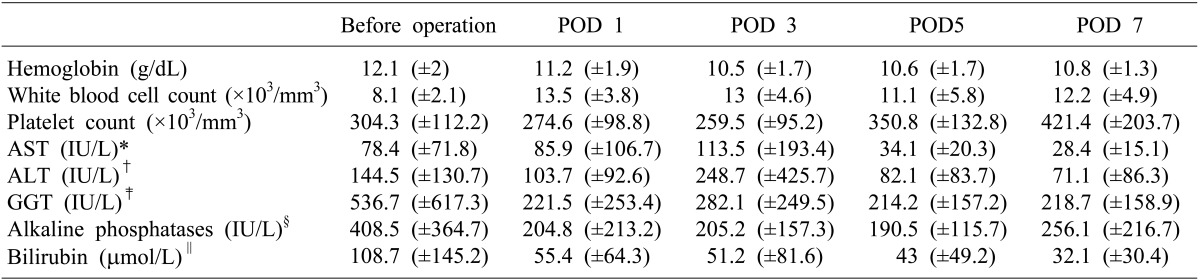
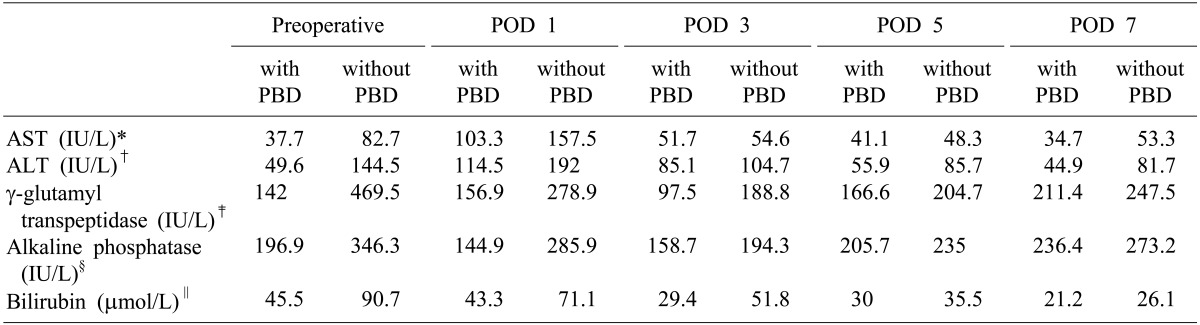
Blood changes were listed in Table 3. The maximal fall in hemoglobin level occurred on day 3 and began to increase after POD 5, in patients with or without transfusions (Fig. 3). The white blood cell count increased on POD 1 and persisted until POD 7. There was a marked rise in aminotransferase levels at POD 3. The peak was significantly higher in patients who had hepatic pedicle occlusion (866±236 IU/L versus 146±48 IU/L; p<0.001). For both γ-glutamyl transpeptidase and alkaline phosphatase, there was a drop on POD 1 (respectively –58.7% and –49.9%), which persisted until day 5 followed by stabilization. Blood hepatic changes in patients with or without preoperative biliary drainage (PBD) were listed in Table 4. Mean duration between PBD and PD was 14±5 days.
Mean postoperative length of hospital stay was 16.4±4.3 days. Mean number of days until nasogastric tube (NGT) removal was 5.6±1.9 days. Mean daily output was shown in Fig. 1. Mean number of days until removal of abdominal drains was 8.9±3.5 days. Mean daily output was shown in Fig. 2. Fourty-seven patients (68.1%) received octreotide for a mean of 8±2 days. Nineteen patients (27.5%) received erythromycin for a mean of 10.4±6.3 days.
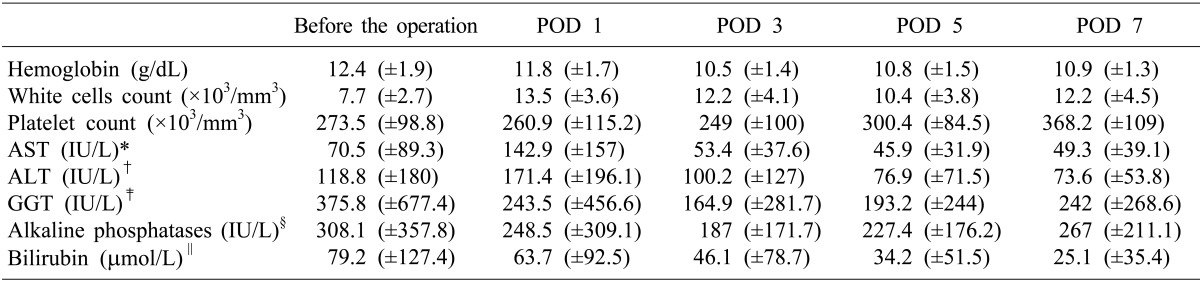
Blood changes were listed in Table 5. The controlled external population confirmed the maximal drop in hemoglobin level on POD 3 (in patients with or without transfusions), the increase in the white blood cell count on POD 1 and during 1 week, and the peak of aminotransferase levels on POD 3. The peak was significantly higher in patients who had hepatic pedicle occlusion (256±126 Units/L versus 76±48 Units/L; p<0.001). Changes of serological liver function test in patients with or without preoperative biliary drainage were listed in Table 6. Mean duration between PBD and PD was 15±6 days.
Historically, PD is associated with a high rate of mortality and morbidity. Hence, some surgeons recommend that this procedure should be discontinued.23 A better selection of patients, improvements in surgical technique and perioperative care contributed to improving the mortality rate. Current perioperative mortality in high-volume centers varies from 1 to 4%.202122 Despite progress in perioperative management, postoperative complications have remained a significant problem with a morbidity rate of 35 to 50%.23 The overall morbidity rate was at its highest (66.4%) in our series. Some studies have shown an association between increased hospital volume and better outcomes for PD.202425 Our department could be considered as a high volume center.2425 Before 2007, there was no standardized definition of PF or of DGE. The incidence of PF could range from 2 to 24%,while the incidence of DGE could range from 14 to 70%, which makes objective comparison of surgical experiences impossible.26 In this series, we chose the less restrictive definition of PF that is internationally accepted. In addition, there is no consensus within the surgical community regarding the report of surgical complications: in the present study, even patients with grade I complications in Clavien's classification12 (complications that did not require any treatment) were considered. As a result of very strict criteria of inclusion, our studied population was homogeneous. We aimed to define standard postoperative outcomes in patients after PD for early recognition of complications.27 Additionally, the complete assessment of the postoperative course can provide better information to the patient.
In the present study, the mean length of stay was about 20 days. The length of stay would reflect the required time for recovery of hemodynamic stability and bowel function and for the ability to resume adequate diet and activities of daily life. Several recent studies of patients undergoing PD have reported median length of stay of 10 to 16 days.42829 It is difficult to compare the length of hospitalization in studies from different countries with totally different insurance coverage. In our series, the longer hospital stay could be explained by the wait time for a convalescence home, and this duration was not measured. In addition, in our study, the length of stay was longer than the mean number of days until NGT removal and drains, which were 6.3 and 9.8 days, respectively. The mean number of days until NGT removal was similar to the study of Brooks et al.29 with a median NGT removal of 5.5 days. Nevertheless, the length of stay could be decreased by providing food to patients who do not have PF or DGE earlier. This shows the importance of early detection of complications to improve management of non-complicated patients. Use of standardized pathways of care based on fast-track concepts could be proposed to reduce hospital stay and stabilize costs. However, the level of evidence to support most aspects of clinical fast-track practice are low, and for many items there was no article specifically focusing on pancreatic surgery.3031 Our data in non-complicated patients indicated that the trend towards the streamlining of perioperative care is a major determiner of length of stay for PD. Selected patients who had signs of complications can enjoy some benefits of fast-track rehabilitation.
The increase in white blood cell count is maximal at POD 1, prolonged throughout the week, without any infectious complications. There was no data published regarding post-PD leukocytosis. However, there were data about post-hepatectomy leukocytosis.32 Moderate leukocytosis without any other signs of infection should not be regarded as a sign of complication. The hemoglobin drop observed at POD 1 could be secondary to blood loss and a hemodilution intraoperatively. After POD 1, hemoglobin remained stable and no patients in our series had red blood cell transfusion postoperatively. A drop in the hemoglobin level without externalized bleeding can be regarded as a "sentinel drop in hemoglobin". In most cases, the sentinel bleeding may allow for the early management of hemorrhage before it becomes massive with circulatory impairment. Massive bleeding may be preceded some hours or days before by a warning bleed originating from the gastrointestinal tract or abdominal drains representing the prelude to massive arterial hemorrhage.3334 Brodsky and Turnbull35 used the term "sentinel bleeding". Sentinel bleeding precedes delayed bleeding in 25 to 100% of cases.36 In patients with sentinel bleeding or patients at risk of delayed hemorrhage, helical computed tomography scan with 3-dimensional angiography allows for the early diagnosis of pseudo-aneurysms, as shown by our experience.1134
The drop in alkaline phosphatase, γ-glutamyl transferase and bilirubin at POD 1 accounts for biliary decompression. There was no difference between patients who required PBD and those who did not require PBD. Indeed, the biliary drain allows the drop in bilirubin serum levels from 207 to 135.8 µmol/L before PD, but there was no difference between bilirubin serum levels postoperatively. The mean duration between PBD and PD was 14 days, which was potentially too short. The duration of drainage should probably be at least 4 to 6 weeks. Even if the bilirubin level has decreased to normal levels, hepatic function will fully be restored only after at least 4 to 6 weeks. Hepatic mitochondrial functions,37 depressed cell-mediated immunity, impaired hepatic reticulo-endothelial function,38 and altered lymphocyte transformation39 are unlikely to improve within 4 weeks. Bile ductal proliferation and hepatic fibrosis may partially reverse at 4 to 6 weeks after removal of biliary obstruction.4041
There was an increase in transaminase levels after PD. It could be the consequence of hepatic resection associated with PD and of pedicle inflow occlusion associated with portal resection. Even if our series is too small to conclude, transaminases are not a good biochemical test to follow-up after PD.
In summary, this study facilitates a standardized biological and clinical pathway of follow-up. Patient who do not follow this recovery indicator may be suspected of not having simple postoperative outcomes. Therefore, careful clinical examination and additional examinations are indicated in these patients. Conversely, patients who have no complications can enjoy some benefits of fast-track rehabilitation.
References
1. Whipple AO, Parsons WB, Mullins CR. Treatment of carcinoma of the ampulla of vater. Ann Surg. 1935; 102:763–779. PMID: 17856666.
2. Crile G Jr. The advantages of bypass operations over radical pancreatoduodenectomy in the treatment of pancreatic carcinoma. Surg Gynecol Obstet. 1970; 130:1049–1053. PMID: 4192028.
3. Shapiro TM. Adenocarcinoma of the pancreas: a statistical analysis of biliary bypass vs Whipple resection in good risk patients. Ann Surg. 1975; 182:715–721. PMID: 1190874.
4. Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg. 2006; 244:10–15. PMID: 16794383.

5. Trede M, Schwall G, Saeger HD. Survival after pancreatoduodenectomy. 118 consecutive resections without an operative mortality. Ann Surg. 1990; 211:447–458. PMID: 2322039.
6. Pessaux P, Varma D, Arnaud JP. Pancreaticoduodenectomy: superior mesenteric artery first approach. J Gastrointest Surg. 2006; 10:607–611. PMID: 16627229.

7. Sastre B, Ouassi M, Pirro N, Cosentino B, Sielezneff I. Pancreaticoduodenectomy in the era of evidence based medicine. Ann Chir. 2005; 130:295–302. PMID: 15935785.
8. Yeo CJ, Barry MK, Sauter PK, Sostre S, Lillemoe KD, Pitt HA, et al. Erythromycin accelerates gastric emptying after pancreaticoduodenectomy. A prospective, randomized, placebo-controlled trial. Ann Surg. 1993; 218:229–237. PMID: 8103982.
9. Ohwada S, Satoh Y, Kawate S, Yamada T, Kawamura O, Koyama T, et al. Low-dose erythromycin reduces delayed gastric emptying and improves gastric motility after Billroth I pylorus-preserving pancreaticoduodenectomy. Ann Surg. 2001; 234:668–674. PMID: 11685031.

10. Martin C. The use of microbial prophylaxis in visceral surgery. Update 1999. J Chir (Paris). 1999; 136:211–215. PMID: 10615589.
11. Bruno O, Brancatelli G, Sauvanet A, Vullierme MP, Barrau V, Vilgrain V. Utility of CT in the diagnosis of pancreatic fistula after pancreaticoduodenectomy in patients with soft pancreas. AJR Am J Roentgenol. 2009; 193:W175–W180. PMID: 19696255.

12. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.
13. Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America. American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007; 1. 44(Suppl 2):S27–S72. PMID: 17278083.

14. Rotstein C, Evans G, Born A, Grossman R, Light RB, Magder S, et al. Clinical practice guidelines for hospital-acquired pneumonia and ventilator-associated pneumonia in adults. Can J Infect Dis Med Microbiol. 2008; 19:19–53. PMID: 19145262.

15. Torres A. American Thoracic Society. Infectious Disease Society of North America. The new American Thoracic Society/Infectious Disease Society of North America guidelines for the management of hospital-acquired, ventilator-associated and healthcare-associated pneumonia: a current view and new complementary information. Curr Opin Crit Care. 2006; 12:444–445. PMID: 16943723.

16. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. International Study Group on Pancreatic Fistula Definition.Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13. PMID: 16003309.

17. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007; 142:761–768. PMID: 17981197.

18. Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007; 142:20–25. PMID: 17629996.
19. Pessaux P, Sauvanet A, Mariette C, Paye F, Muscari F, Cunha AS, et al. Fédération de Recherche en Chirurgie (French). External pancreatic duct stent decreases pancreatic fistula rate after pancreaticoduodenectomy: prospective multicenter randomized trial. Ann Surg. 2011; 253:879–885. PMID: 21368658.
20. Sosa JA, Bowman HM, Gordon TA, Bass EB, Yeo CJ, Lillemoe KD, et al. Importance of hospital volume in the overall management of pancreatic cancer. Ann Surg. 1998; 228:429–438. PMID: 9742926.

21. Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 2000; 232:786–795. PMID: 11088073.

22. Cameron JL, Pitt HA, Yeo CJ, Lillemoe KD, Kaufman HS, Coleman J. One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg. 1993; 217:430–435. PMID: 8098202.

23. Yeo CJ, Cameron JL, Sohn TA, Lillemoe KD, Pitt HA, Talamini MA, et al. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg. 1997; 226:248–257. PMID: 9339931.
24. Birkmeyer JD, Warshaw AL, Finlayson SR, Grove MR, Tosteson AN. Relationship between hospital volume and late survival after pancreaticoduodenectomy. Surgery. 1999; 126:178–183. PMID: 10455881.

25. Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003; 349:2117–2127. PMID: 14645640.

26. Bassi C, Butturini G, Molinari E, Mascetta G, Salvia R, Falconi M, et al. Pancreatic fistula rate after pancreatic resection. The importance of definitions. Dig Surg. 2004; 21:54–59. PMID: 14707394.
27. Lermite E, Sommacale D, Piardi T, Arnaud JP, Sauvanet A, Dejong CH, et al. Complications after pancreatic resection: diagnosis, prevention and management. Clin Res Hepatol Gastroenterol. 2013; 37:230–239. PMID: 23415988.

28. Fernández-del Castillo C, Rattner DW, Warshaw AL. Standards for pancreatic resection in the 1990s. Arch Surg. 1995; 130:295–299. PMID: 7887797.

29. Brooks AD, Marcus SG, Gradek C, Newman E, Shamamian P, Gouge TH, et al. Decreasing length of stay after pancreatoduodenectomy. Arch Surg. 2000; 135:823–830. PMID: 10896377.

30. Salvia R, Malleo G, Butturini G, Dal Molin M, Esposito A, Marchegiani G, et al. Perioperative management of patients undergoing pancreatic resection: implementation of a care plan in a tertiary-care center. J Surg Oncol. 2013; 107:51–57. PMID: 23129003.

31. di Sebastiano P, Festa L, De Bonis A, Ciuffreda A, Valvano MR, Andriulli A, et al. A modified fast-track program for pancreatic surgery: a prospective single-center experience. Langenbecks Arch Surg. 2011; 396:345–351. PMID: 20703500.

32. Suc B, Panis Y, Belghiti J, Fékété F. 'Natural history' of hepatectomy. Br J Surg. 1992; 79:39–42. PMID: 1346582.

33. Shankar S, Russell RC. Haemorrhage in pancreatic disease. Br J Surg. 1989; 76:863–866. PMID: 2765846.

34. Blanc T, Cortes A, Goere D, Sibert A, Pessaux P, Belghiti J, et al. Hemorrhage after pancreaticoduodenectomy: when is surgery still indicated? Am J Surg. 2007; 194:3–9. PMID: 17560900.

35. Brodsky JT, Turnbull AD. Arterial hemorrhage after pancreatoduodenectomy. The 'sentinel bleed'. Arch Surg. 1991; 126:1037–1040. PMID: 1863209.
36. de Castro SM, Kuhlmann KF, Busch OR, van Delden OM, Laméris JS, van Gulik TM, et al. Delayed massive hemorrhage after pancreatic and biliary surgery: embolization or surgery? Ann Surg. 2005; 241:85–91. PMID: 15621995.

37. Koyama K, Takagi Y, Ito K, Sato T. Experimental and clinical studies on the effect of biliary drainage in obstructive jaundice. Am J Surg. 1981; 142:293–299. PMID: 6789695.

38. Hunt DR, Allison ME, Prentice CR, Blumgart LH. Endotoxemia, disturbance of coagulation, and obstructive jaundice. Am J Surg. 1982; 144:325–329. PMID: 7114371.

39. Fan ST, Lo CM, Lai EC, Yu WC, Wong J. T lymphocyte function in patients with malignant biliary obstruction. J Gastroenterol Hepatol. 1994; 9:391–395. PMID: 7948822.

40. Aronson DC, Chamuleau RA, Frederiks WM, Gooszen HG, Heijmans HS, James J. Reversibility of cholestatic changes following experimental common bile duct obstruction: fact or fantasy? J Hepatol. 1993; 18:85–95. PMID: 8340613.

41. Zimmermann H, Reichen J, Zimmermann A, Sägesser H, Thenisch B, Höflin F. Reversibility of secondary biliary fibrosis by biliodigestive anastomosis in the rat. Gastroenterology. 1992; 103:579–589. PMID: 1634077.

Table 4
Biochemical changes after the operation in internal population (n=43 patients) according to a preoperative biliary drainage (PBD)




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download