Abstract
Backgrounds/Aims
Laparoscopic cholecystectomy can reduce postoperative pain and recovery time. However, some patients experience prolonged postoperative hospital stay. We aimed to identify factors influencing the postoperative hospital stay after laparoscopic cholecystectomy.
Methods
Patients (n=336) undergoing laparoscopic cholecystectomy for gallbladder pathology at 8 hospitals were enrolled and divided into 2 groups: 2 or less and more than 2 days postoperative stay. Perioperative factors and patient factors were retrospectively analyzed.
Results
The patient population median age was 52 years, and consisted of 32 emergency and 304 elective operations. A univariate analysis of perioperative factors revealed significant differences in operation time (p<0.001), perioperative transfusion (p=0.006), emergency operation (p<0.001), acute inflammation (p<0.001), and surgical site infection (p=0.041). A univariate analysis of patient factors revealed significant differences in age (p<0.001), gender (p=0.036), diabetes mellitus (p=0.011), preoperative albumin level (p=0.024), smoking (p=0.010), and American Society of Anesthesiologists score (p=0.003). In a multivariate analysis, operation time (p<0.001), emergency operation (p<0.001), age (p=0.014), and smoking (p=0.022) were identified as independent factors influencing length of postoperative hospital stay.
Laparoscopic cholecystectomy (LC) has been the treatment of choice for symptomatic gallstone disease since 1990.12 The main advantages of LC include less postoperative pain, shorter operation time, lower rate of postoperative complications and early ambulation leading to shorter hospital stay. In a study by Tsang et al.,3 independent predictive factors for delayed postoperative stay included age over 60 years, time for diet resumption greater than 8 hours, and oral analgesia intake of greater than two tablets. Operative findings of acute inflammation or postoperative complications did not have any influence on the length of hospital stay. Recently, Morimoto et al.4 reported that the American Society of Anesthesiologists (ASA) score and LC difficulty are the most predictive factors on length of hospital stay. Other studies have proposed advanced age and intraoperative complications as predictive risk factors.567 While an outpatient procedure is popular for LC, defining the indications and predictive factors associated with a delay in postoperative hospital stay is essential for maximizing the benefits of LC. However, there are few published articles on factors influencing the postoperative hospital stay after LC.348 This study aimed to identify influencing factors on postoperative hospital stay after LC based on retrospective analysis of data from multiple centers.
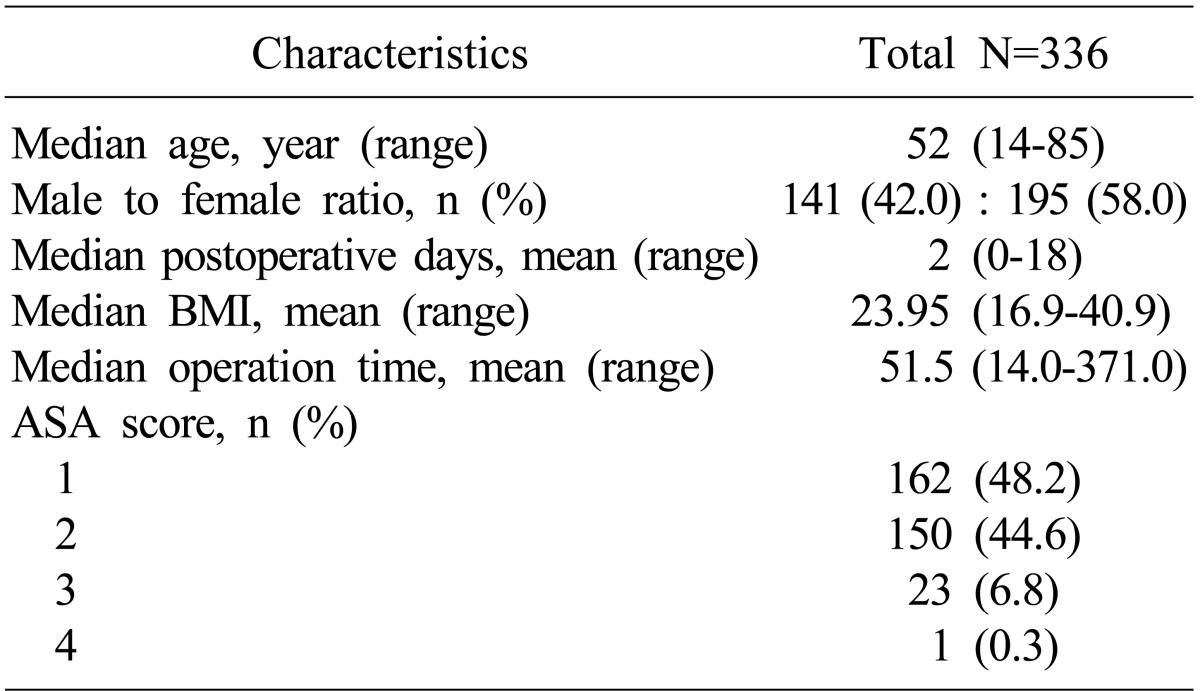
Between August 1, 2012 and August 31, 2012, 336 consecutive patients underwent LC for benign gallbladder disease at 8 different hospitals (Severance Hospital, Gangnam Severance Hospital, Wonju Severance Christian Hospital, Incheon & Daejeon St. Mary Hospital, National Health Insurance Service Ilsan Hospital, Seoul National University Bundang Hospital, and Guro Hospital). Demographic data and clinicopathologic parameters, as well as perioperative data, were gathered through a retrospective review of medical records. Patient characteristics were shown in Table 1.
The median age for all patients was 52 years (range: 14-85 years), and 141 (42%) were male and 195 (58%) female. Postoperative hospital day (POHD) was defined as the number of days from the day of operation (day 0) until hospital discharge. Patients were discharged when they were afebrile and mobile, solid food was well tolerated, and pain was adequately controlled by oral analgesia. Since POHD was not normally distributed, the median value of POHD was used to define prolonged postoperative hospital stay. Median POHD was 2 days (range: 0-18 days) and patients were divided into 2 groups. The early discharge (ED) group included patients discharged within 2 postoperative days and the late discharge (LD) group included patients discharged after more than 2 postoperative days. Possible influencing factors on POHD in the 2 groups were retrospectively analyzed.
Influencing factors on POHD were divided into perioperative and patient factors. Perioperative factors included operation time, perioperative transfusion, emergency operation, previous abdominal operation history, acute inflammation of gallbladder defined by histopathologic examination, gallbladder stones, and surgical site infections. The laparoscopic cholecystectomy was performed using a standard 3- or 4-port technique. Preoperative endoscopic retrograde cholangiopancreatography (ERCP) was performed when indicated by ultrasonograph findings. Patients were examined for surgical site infection (SSI) until hospital discharge and again at the first postoperative visit. All patients were followed up within 7 days from discharge in the outpatient department. Postoperative SSIs were defined according to the Center for Disease Control and Prevention (CDC) guidelines. Superficial or deep SSIs were defined as purulent discharge from the surgical site, with or without positive culture or signs of inflammation. Patient factors included age, gender, body mass index (BMI), diagnosis of diabetes mellitus, preoperative albumin level, smoking, and ASA score.
Analysis was performed with the Statistical Package for Social Sciences version 20 (SPSS, Chicago, IL, USA). A Shapiro-Wilk test was used to test normality for each quantitative variable. Comparisons between groups were performed using the Mann-Whitney test, chi-square test, or Fisher's exact test, as appropriate. Multiple logistic regression analysis was performed to assess influencing factors for POHD. All variables with significant results from univariate analysis were included. A p-value for statistical significance was set at 0.05.
In this study, of the 336 laparoscopic cholecystectomy cases analyzed, the ED group included 225 (67%) patients and the LD group included the remaining 111 (33%) patients. The median POHD for the ED group was 1 day (range: 0-2 days), and the median POHD for the LD group was 4 days (range: 3-18 days). The only postoperative mortality case was a 76-year-old woman.
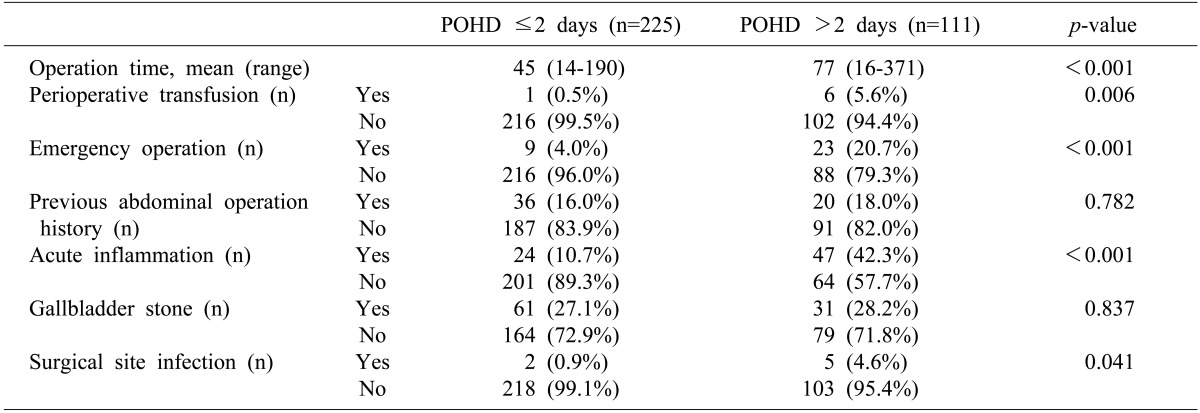
Seven factors were analyzed as possible perioperative factors influencing the POHD. The average operation times of the ED and LD groups were 45 and 77 minutes, respectively, with significant difference (p<0.001). Other perioperative factors that differed significantly included perioperative transfusion (p=0.006), emergency operation (p<0.001), acute inflammation of the gallbladder (p<0.001), and surgical site infection (p=0.041). Emergency operations accounted for 20.7% of the LD group, as compared to only 4.0% of the ED group. The ED and LD groups showed no significant differences in abdominal operation history (p=0.782) and the presence of a gallbladder stone (p=0.837). Only 7 SSIs were found in all patients. Six SSIs were superficial and one was an organ/space infection. The 2 SSIs in the ED group were superficial infections. The results of the univariate analysis of perioperative factors were depicted in Table 2.
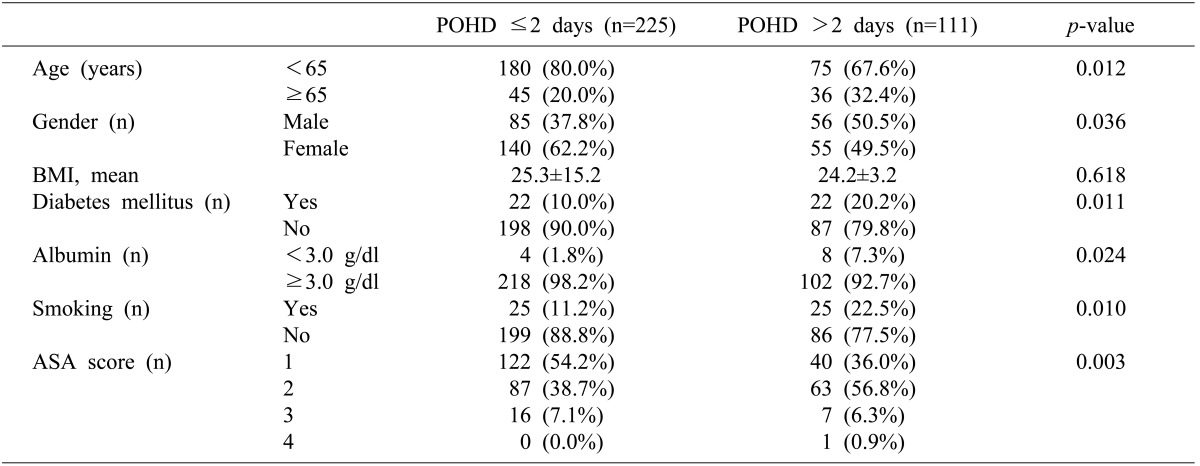
Patient variables were analyzed to determine factors that differed significantly between the ED and LD groups. Age (p=0.012), gender (p=0.036), diagnosis of diabetes mellitus (p=0.011), preoperative albumin level (p=0.024), smoking (p=0.010), and ASA score (p=0.003) were significantly different among the groups (Table 3). The median POHD in the 44 patients with diabetes mellitus was 3 days (range: 1-18 days), and in the 285 patients without diabetes mellitus, it was 2 days (range: 0-16 days). Patients with albumin levels below 3.0 g/dl at admission (12 patients) had a median POHD of 5 days (range: 1-18 days) and patients with albumin levels over 3.0 g/dl (320 patients) had a median POHD of 2 days (range: 0-16 days).
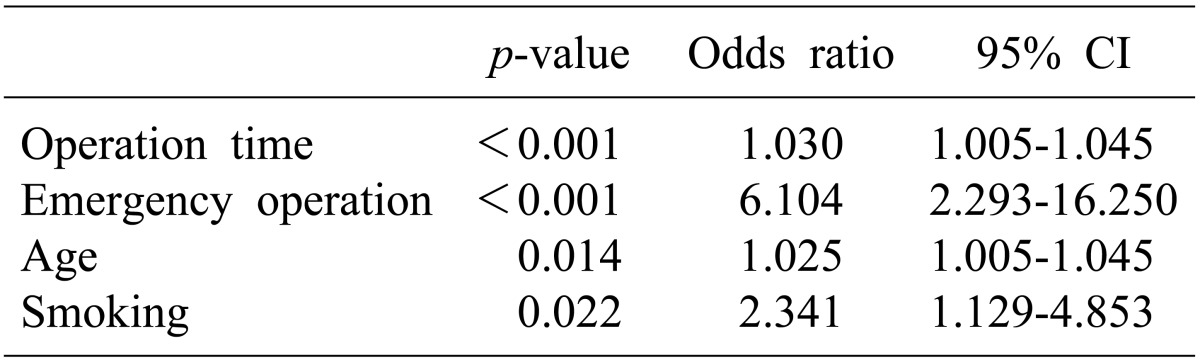
Multivariate logistic regression analysis of all significant factors in the univariate analyses yielded 4 independent influencing factors (Table 4). Emergency operation showed the highest odds ratio of 6.104 (95% confidence interval (CI): 2.293-16.250, p<0.001). Smoking was also an independent influencing factor with an odds ratio of 2.341 (95% CI: 1.129-4.853, p=0.022). Operation time (p<0.001) and age (p=0.014) were statistically significant factors that influenced POHD after LC with odds ratios of 1.030 (95% CI: 1.005-1.045) and 1.025 (95% CI: 1.005-1.045), respectively.
Perioperative transfusion, acute inflammation, SSI, gender, diabetes mellitus, albumin, and ASA scores failed to show significant differences in a multivariate analysis.
Improvements in LC and anesthetic techniques, together with increased familiarity with the procedure lead to progressively shorter hospital stays.9 In a recent study by Morimoto et al.,4 ASA scores and LC difficulty were the most influential predictive risk factors for a longer hospital stay. In addition, LC in elderly patients is associated with higher complications rates and longer hospital stays.810 Elderly patients are more likely to present with complicated cases of gallbladder disease, tend to present later than younger patients, and present with relatively benign symptoms that may conceal the severity of the case.11 Our results confirmed that age and prolonged operation time are independent factors contributing to delayed hospital stays. However, our results also suggested that while acute cholecystitis and advanced health problems are significant risk factors in the univariate analysis, they are not independent risk factors for delayed hospital stays. Our results showed that previous abdominal operation history is not associated with delayed POHD.
In evaluating patient-related risk factors, diabetes mellitus, albumin level, and smoking were also analyzed. Patients with diabetes mellitus are known to have poorer surgical outcomes and higher rates of intraoperative complications.12 While our results confirmed that more patients with diabetes mellitus belonged to the LD group, diabetes mellitus was not an independent influencing factor for POHD. Nevertheless, careful sugar control during the perioperative course should be considered for patients with diabetes mellitus. A significantly higher percentage of patients had lower preoperative albumin levels in the LD group, as compared to the ED group. Although, a lower level of albumin also failed to show significance as an independent factor, further investigation into the influence of nutritional state on POHD should be considered. Nutritional therapy or albumin replacement may be considered to reduce POHD for patients with lower preoperative albumin levels. Current smoking was found to be an independent influencing factor on delayed POHD. Since smoking is considered a risk factor for pulmonary complications and surgical site infection, patients should be advised to cease smoking prior to an elective surgery.
The limitations of this study included the bias inherent to the retrospective nature of the design and a lack of consensus on discharge criteria among the participating hospitals. Decisions on discharge were subject to surgeon preferences. This may have confounded the results; however, our results still concurred with previous findings from other studies.
Our study was a retrospective review of LC during a 1 month period at multiple centers. The study did not have any exclusion criteria, and included all patients who underwent successful LC without open conversion. With broad inclusion criteria, a more accurate assessment of influencing factors for POHD was expected. With proper patient selection and adequate preoperative preparation, more patients could benefit from a reduced postoperative hospital stay. Patients with diabetes mellitus should be considered for strict perioperative sugar control and nutritional therapy should be considered for patients with low levels of preoperative albumin.
Although emergency operation was shown to have highest odds ratio as an influencing factor of postoperative hospital stay, causality should be carefully interpreted. Subgroup analysis revealed that older patients underwent emergency operation more frequently: Median age for emergency operation was 61 year (range: 30-85 years) and median age for elective operation was 52 years (range: 14-85 years) with p=0.003. In addition, 26 (81.2%) of 32 emergency operations were acute cholecystitis, while only 45 (14.9%) of 303 elective operations were acute cholecystitis (p<0.001). Though, acute cholecystitis was not an independent factor for prolonged hospital stay, acute cholecystitis in elderly patients may be an inevitable condition for emergency operation and prolonged hospital stay.
In terms of patient factors, patients with advanced age or diabetes should be informed of the possibility of a lengthened postoperative hospital stay, and smoking cessation prior to an elective laparoscopic cholecystectomy may be helpful in reducing postoperative hospital stay.
References
1. McMahon AJ, Fischbacher CM, Frame SH, MacLeod MC. Impact of laparoscopic cholecystectomy: a population-based study. Lancet. 2000; 356:1632–1637. PMID: 11089821.

2. Shea JA, Berlin JA, Bachwich DR, Staroscik RN, Malet PF, McGuckin M, et al. Indications for and outcomes of cholecystectomy: a comparison of the pre and postlaparoscopic eras. Ann Surg. 1998; 227:343–350. PMID: 9527056.
3. Tsang YY, Poon CM, Lee KW, Leong HT. Predictive factors of long hospital stay after laparoscopic cholecystectomy. Asian J Surg. 2007; 30:23–28. PMID: 17337367.

4. Morimoto Y, Mizuno H, Akamaru Y, Yasumasa K, Noro H, Kono E, et al. Predicting prolonged hospital stay after laparoscopic cholecystectomy. Asian J Endosc Surg. 2015; 8:289–295. PMID: 25786914.

5. Choi JB, Lim JH, Kim SH, Lee SY, Lee SJ, Kim KS. Feasible factors to reduce hospital days after laparoscopic cholecystectomy. J Minim Invasive Surg. 2014; 17:80–84.

6. Lee SR, Shin JH. Clinical study of delayed discharge after laparoscopic-cholecystectomy. J Korean Soc Endosc Laparosc Surg. 2010; 13:11–16.
7. Robinson TN, Biffl WL, Moore EE, Heimbach JK, Calkins CM, Burch JM. Predicting failure of outpatient laparoscopic cholecystectomy. Am J Surg. 2002; 184:515–518. PMID: 12488152.

8. Cheng SP, Chang YC, Liu CL, Yang TL, Jeng KS, Lee JJ, et al. Factors associated with prolonged stay after laparoscopic cholecystectomy in elderly patients. Surg Endosc. 2008; 22:1283–1289. PMID: 17968623.

9. Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006; (4):CD006231. PMID: 17054285.

10. Sauerland S, Agresta F, Bergamaschi R, Borzellino G, Budzynski A, Champault G, et al. Laparoscopy for abdominal emergencies: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc. 2006; 20:14–29. PMID: 16247571.
11. Morrow DJ, Thompson J, Wilson SE. Acute cholecystitis in the elderly: a surgical emergency. Arch Surg. 1978; 113:1149–1152. PMID: 708235.
12. Gelbard R, Karamanos E, Teixeira PG, Beale E, Talving P, Inaba K, et al. Effect of delaying same-admission cholecystectomy on outcomes in patients with diabetes. Br J Surg. 2014; 101:74–78. PMID: 24338895.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download