Abstract
The diagnosis of gallstone ileus is occasionally challenging due to the variability of its presentation. We herein present a very rare case of gallstone ileus inducing obstructive jaundice at the afferent loop of Roux-en-Y hepaticojejunostomy after 10 years of bile duct cancer surgery. We describe the case of a 74-year-old Korean woman with obstructive jaundice, treated conservatively. She showed severely impaired liver function test and obstructive jaundice. The computed tomography (CT) scan led to a diagnosis of very rare type of gallstones ileus at the afferent jejunal loop. Since the clinical manifestation was improved, we decided to observe her closely. On the next follow-up CT scan, the gallstone disappeared with mild distension of the afferent bowel loop, implicating spontaneous passage of the gallstone. She recovered and returned to normal life after 10 days of initiation of clinical manifestations. We presume that the gallstone may enter the afferent jejunal loop through the hepaticojejunostomy and later increase in size. The presence of narrow tract of intestine may facilitate the incidence of gallstone ileus. It appears to be the first report on this rare type of gallstone ileus inducing obstructive jaundice.
Gallstone ileus is a rare mechanical bowel obstruction caused by the transition of a gallstone in the gastrointestinal tract through a biliary-enteric fistula, or following endoscopic retrograde cholangiopancreatography (ERCP), which occurs in 1 to 3% of all cases of mechanical ileus.1 Gallstones can cause bowel obstruction by intraluminal impaction anywhere between the stomach and the rectum, thus abdomen computed tomography (CT) is very informative for diagnosis of gallstone ileus.23
Large gallstones inducing ileus are usually formed within the gallbladder, thus it is very rare to present gallstone ileus after cholecystectomy.4 In contrast, gallstones have been occasionally formed at the proximal side of hepaticojejunostomy after resection of the common bile duct and then passed through the lumen of hepaticojejunostomy. In this type of intrahepatic duct stone formation, the stones are usually muddy, not being solid stones due to the luminal environment of the hepaticojejunostomy.
We herein present an extremely rare case of gallstone ileus, in whom the gallstone stone was formed at the hepaticojejunostomy and entrapped at afferent loop of the Roux-en-Y jejunojejunostomy, by which obstructive jaundice happened and resolved after spontaneous passage.
A 74-year-old Korean woman was referred to our institution due to obstructive jaundice. She had undergone curative resection of the extrahepatic bile duct cancer (2 cm-sized moderately differentiated adenocarcinoma of T2N0M0) 10 years before. She had been followed up regularly until the end of postoperative 9 years without any evidence of disease recurrence. However, 3 days before referral, at 10 years after surgery, she complained of abdominal discomfort with no episode of biliary colic and visited a local hospital. Liver enzyme levels were very high (aspartate aminotransferase [AST] 1245 IU/L; alanine aminotransferase [ALT] 1065 IU/L) and jaundice was developed (total bilirubin 3.1 mg/dl and direct bilirubin 2.5 mg/dl).
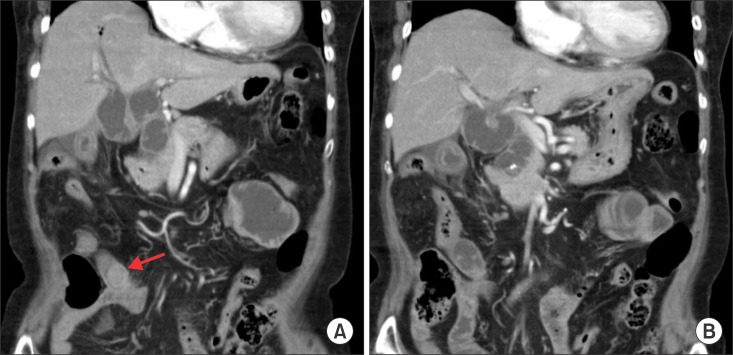
Abdomen-pelvis CT scan showed that there was a 1.7 cm-wide and 2.5 cm-long radiopaque stone at approximately 15 cm below the level of hepaticojejunostomy site with upstream afferent loop bowel dilatation and concentric bowel wall thickening of the segmental jejunal loop (Fig. 1). The intrahepatic ducts were also dilated with inhomogeneous enhancement of the liver parenchyma. Thus the primary diagnosis was gallstone ileus causing afferent loop syndrome and enteritis. Thereafter, she was transferred to our institution for further management.
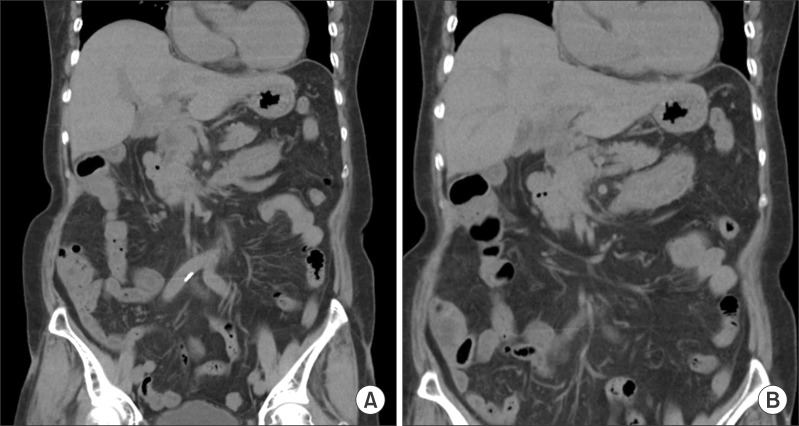
Since her symptoms of abdominal discomfort were not severe and her gross appearance was not so seriously ill with normal vital signs, we decided to observe her closely for 1 or 2 days. On follow-up of liver function tests, hepatic dysfunction improved rapidly, thus implicating spontaneous passage of gallstone impaction. After 3 days of admission, unenhanced follow-up CT scan was performed, in which intraluminal radiopaque lesion disappeared with mild distension and edematous wall thickening of the afferent bowel loop (Fig. 2). These findings implicate the gallstone was spontaneous passed through the bowel and then removed with feces. She recovered soon and returned to normal life at 10 days after initiation of clinical manifestations.
It was presumed that a gallstone was formed and grown up at the hepaticojejunostomy site within recent 1 year and then passed through the afferent jejunal loop. Since there was a gross stenosis at the jejunojejunostomy site, in which the gallstone was grown up further within the afferent jejunal loop and finally impacted. As a result, gallstone ileus of the afferent jejunal loop happened with development of obstructive jaundice. Since the gallstone was not so large, it passed the jejunojejunostomy site spontaneously and removed from the anus.
The most frequent mechanism of gallstone ileus is the migration of gallstones through a gallbladder-duodenal fistula. Gallstone ileus is the consequence of an episode of acute cholecystitis and gallbladder adhesion to the bowel. This condition is more frequent in women, given the known prevalence of gallbladder disease in this gender, and in patients over 65 years.156
The size of the gallstone represents a key factor in the development of gallstone ileus since a stone greater than 2.5 cm in diameter can cause small bowel obstruction and even smaller stones can cause gallstone ileus in cases of bowel stenosis. The gallstone usually impacts the terminal ileum or the ileocecal valve because of their anatomical narrowness. Rarely, colonic gallstones can happen if there is a gallbladder-colon fistula.57 More rarely, gallstone ileus has been reported even in absence of a bilioenteric fistula.8 This can be explained by the entrance of the gallstones through the Vater papilla and growth within the small bowel lumen.2 The alteration of the bile salts in the enterohepatic circuit following an ileum resection or in patients with Crohn's disease is a well-known phenomenon.9
Diagnosis of gallstone ileus is occasionally challenging because the clinical manifestation can be characterized by non-specific symptoms and it usually depends on the localization and the nature of the intestinal obstruction. In patients with a clinical history of gallstones, clinical signs of cholecystitis and bowel obstruction, gallstone ileus can be strongly suspected. The onset can manifest as acute, intermittent or chronic episodes.
Plain abdominal X-rays, abdominal ultrasound and CT scans may reveal signs of gallstone ileus and help in the preoperative diagnosis and management of gallstone ileus. Abdomen-pelvis CT scan is readily available and becomes the most reliable test in the current Korean medical setting. The Rigler's triad of radiological features consists of mechanical bowel obstruction, pneumobilia and ectopic stone within the intestinal lumen.1011 The presence of Rigler triad in a plain abdominal radiography was reported to be 17-87%. Two out of these three signs are considered to be sufficient to establish a diagnosis. Only 15% of gallstones are sufficiently calcified to be visualized as radiopaque in a plain abdomen X-ray or CT. In this case, the initial abdomen-pelvis CT scan provided critical information on the pathogenesis and status of the gallstone ileus.
There are still controversies about the management of gallstone ileus. Although spontaneous resolution of gallstone ileus is described,121314 it generally causes acute bowel obstruction, and the aim of treatment is gallstone extraction. Enterolithotomy with stone extraction is the therapy of choice.15 The one-stage procedure (enterotomy, fistula repair and cholecystectomy) is strongly associated with a greater mortality rate, largely due to a delayed diagnosis and concomitant diseases,16 but concurrent performance of biliary surgery and fistula repair reduces complications related to gallstones disease, including recurrent ileus. The two-stage procedure (enterolithotomy followed by cholecystectomy and late repair of the biliodigestive fistula) is an alternative treatment that is suggested for younger patients and in cases of recurrent biliary symptoms.17 Laparoscopic procedures can be an alternative method, although a surgeon with specialist experience in advanced laparoscopic surgery would be necessary.181920 The endoscopic treatment of gallstone ileus is a valid alternative approach and some cases have already been reported.2122 Ultrasound-guided extracorporeal shock wave lithotripsy (ESWL) has also been suggested as a non-invasive alternative to surgery to fragment the stone and solve the sub-occlusion.23
In our case, the disease entity of gallstone ileus could not be even imagined before taking abdomen CT because of the extreme rarity of this type gallstone ileus. Since the gallstone was not large comparing with the stenotic portion of jejunojejunostomy as well as her liver function began to improve, our primary management plan was short-term close observation. If the status of ileus with obstructive jaundice had persisted a few days more, we would insert percutaneous transhepatic biliary drainage (PTBD) to reverse the obstructive jaundice. It may be used for pushing the stone to pass through the stenotic portion of jejunojejunostomy. An enterolithotomy with stone extraction would be the last therapeutic for this patient.
In conclusion, our case demonstrates that the gallstone may enter the afferent jejunal loop through the hepaticojejunostomy and later increase in size. The presence of a narrow tract of intestine can facilitate the incidence of gallstone ileus. It appears to be the first report on this type of gallstone ileus.
References
1. Masannat Y, Masannat Y, Shatnawei A. Gallstone ileus: a review. Mt Sinai J Med. 2006; 73:1132–1134. PMID: 17285212.
2. Pezzoli A, Maimone A, Fusetti N, Pizzo E. Gallstone ileus treated with non-surgical conservative methods: a case report. J Med Case Rep. 2015; 9:15. PMID: 25971789.

3. Michele D, Luciano G, Massimiliano F, Stefano R, Roberta D, Ernesto S, et al. Usefulness of CT-scan in the diagnosis and therapeutic approach of gallstone ileus: report of two surgically treated cases. BMC Surg. 2013; 13(Suppl 2):S6. PMID: 24268073.

4. Zens T, Liebl RS. Gallstone ileus 30 years status postcholecystectomy. WMJ. 2010; 109:332–334. PMID: 21287885.
5. Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg. 1994; 60:441–446. PMID: 8198337.
6. Halabi WJ, Kang CY, Ketana N, Lafaro KJ, Nguyen VQ, Stamos MJ, et al. Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg. 2014; 259:329–335. PMID: 23295322.
7. Heaney RM. Colonic gallstone ileus: the rolling stones. BMJ Case Rep. 2014; [Epub ahead of print].

8. Armitage G, Fowweather FS, Johnstone AS. Observations on bile-acid enteroliths with an account of a recent case. Br J Surg. 1950; 38:21–25. PMID: 15434313.

Andersson H., Bosaeus I., Fasth S., Hellberg R., Hultén L. Cholelithiasis and urolithiasis in Crohn's disease. Scand J Gastroenterol. 1987. 22:253–256. PMID: 3576131.

10. Rigler LG, Borman CN, Noble JF. Gallstone obstruction: pathogenesis and roentgen manifestations. JAMA. 1941; 117:1753–1759.
12. Tandon A, Usha T, Bhargava SK, Bhatt S, Bhargava S, Prakash M, et al. Resolution of gallstone ileus with spontaneous evacuation of gallstone: a case report. Indian J Surg. 2013; 75:228–231. PMID: 24426434.

13. Roberts J, Lambrianides A. Spontaneous resolution of a gallstone ileus. J Surg Case Rep. 2012; 2012:3. PMID: 24960807.

14. Miyasaka T, Yoshida H, Makino H, Watanabe M, Uchida E, Uchida E. Response of gallstone ileus to conservative therapy. J Nippon Med Sch. 2014; 81:388–391. PMID: 25744483.

15. Mallipeddi MK, Pappas TN, Shapiro ML, Scarborough JE. Gallstone ileus: revisiting surgical outcomes using National Surgical Quality Improvement Program data. J Surg Res. 2013; 184:84–88. PMID: 23764312.

16. Warshaw AL, Bartlett MK. Choice of operation for gallstone intestinal obstruction. Ann Surg. 1966; 164:1051–1055. PMID: 5926241.
17. Zaliekas J, Munson JL. Complications of gallstones: the Mirizzi syndrome, gallstone ileus, gallstone pancreatitis, complications of "lost" gallstones. Surg Clin North Am. 2008; 88:1345–1368. PMID: 18992599.

18. Ferraina P, Gancedo MC, Elli F, Nallar M, Ferraro A, Sarotto L, et al. Video-assisted laparoscopic enterolithotomy: new technique in the surgical management of gallstone ileus. Surg Laparosc Endosc Percutan Tech. 2003; 13:83–87. PMID: 12709612.
19. Bircan HY, Koc B, Ozcelik U, Kemik O, Demirag A. Laparoscopic treatment of gallstone ileus. Clin Med Insights Case Rep. 2014; 7:75–77. PMID: 25187746.

20. Zygomalas A, Karamanakos S, Kehagias I. Totally laparoscopic management of gallstone ileus--technical report and review of the literature. J Laparoendosc Adv Surg Tech A. 2012; 22:265–268. PMID: 22303929.

21. Lübbers H, Mahlke R, Lankisch PG. Gallstone ileus: endoscopic removal of a gallstone obstructing the upper jejunum. J Intern Med. 1999; 246:593–597. PMID: 10620104.

22. Muratori R, Cennamo V, Menna M, Cecinato P, Eusebi LH, Mazzella G, et al. Colonic gallstone ileus treated with radiologically guided extracorporeal shock wave lithotripsy followed by endoscopic extraction. Endoscopy. 2012; 44(Suppl 2 UCTN):E88–E89. PMID: 22396298.

23. Meyenberger C, Michel C, Metzger U, Koelz HR. Gallstone ileus treated by extracorporeal shockwave lithotripsy. Gastrointest Endosc. 1996; 43:508–511. PMID: 8726769.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download