Abstract
Ovarian metastases represent about 3-5% of all ovarian malignancies. Most of these tumors originate in the digestive tract and cholangiocarcinoma rarely involves the ovary. A 60-year-old woman was admitted for the investigation of abdominal distension that had lasted 1 week. One and a half years prior, the patient had undergone choledochal cyst excision, Roux-en Y hepaticojejunostomy and cholecystectomy. Computed tomography scans of the abdomen revealed a papillary mass in the remnant distal common bile duct and enlargement of both ovaries with a huge amount of ascites. An explorative laparotomy disclosed no peritoneal seeding with resectable cholangiocarcinoma and bilateral ovarian mass. Pylorus-preserving pancreatoduodenectomy and bilateral salphingo-oophorectomy with hysterectomy were performed. Histologically, it was a well-differentiated adenocarcinoma and all surgical margins were free of tumor. Both ovarian masses were consistent with metastatic adenocarcinoma from the common bile duct. The patient received six cycles of postoperative adjuvant systemic chemotherapy, dying after 10 months due to pulmonary embolism.
Go to : 
Ovarian metastases represent about 3-5% of all ovarian malignancies.1 Because they occasionally mimic the clinical and morphological appearance of primary tumors, diagnosis is difficult. The majority of these neoplasias originate from the digestive tract, particularly from stomach and biliary tract, cholangiocarcinomas are very rare tumors that rarely involve the ovary. We present a very unusual case of metastatic carcinoma of the common bile duct originating from a choledochal cyst presenting as an ovarian metastasis in a 60-year-old woman.
Go to : 
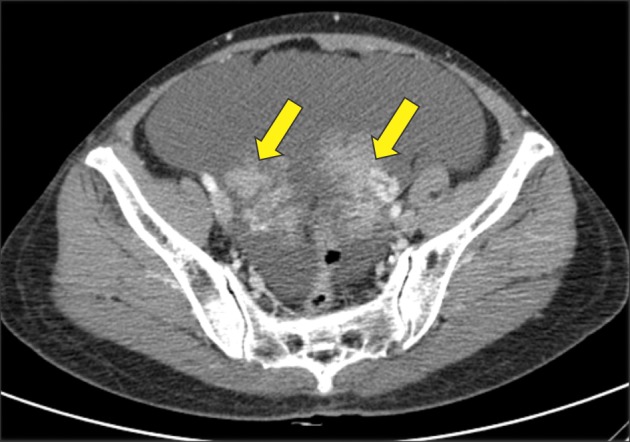
A 60-year-old woman was admitted for the investigation of abdominal distension that had lasted for 1 week. One and a half years prior, the patient had been diagnosed with a choledochal cyst and had undergone choledochal cyst excision, Roux-en Y hepaticojejunostomy and cholecystectomy at another hospital. Histopathologic findings from that time showed no evidence of malignancy of choledochal cyst. On physical examination, her abdomen was soft and distended severely without a palpable mass. Laboratory evaluation revealed elevation levels of alkaline phosphatase (415 U/L, normal range 50-200 U/L) and CA 19-9 (2,409 U/L, normal range <37 U/L). Computed tomography scan and magnetic resonance cholangiopancreatography revealed a papillary mass in the remnant distal common bile duct (CBD) (Fig. 1), bilateral enlargement of ovaries with huge amount of ascites (Fig. 2) and no other metastatic lesion. An explorative laparotomy disclosed no peritoneal seeding with resectable cholangiocarcinoma, bilateral ovarian masses measuring about 10 cm with irregular surface, multilobular cut surface and solid texture and ascites totaling about 1,000 ml. She underwent a pylorus preserving pancreaticoduodenectomy and bilateral salphingo-oophorectomy with hysterectomy. Cross sections of the excised specimen showed CBD dilated to 5 cm in the pancreatic head and papillary mass was seen inside of it. Histologically, it was a well-differentiated adenocarcinoma, which extended to the pancreas with perineural invasion and regional lymph node metastasis. All surgical margins were free of tumor. Both ovarian masses were consistent with metastatic adenocarcinoma from CBD. The post-operative course was uneventful. The patient received six cycles of postoperative palliative adjuvant systemic chemotherapy with 5-fluorouracil and cisplatin. After finishing 6 cycles of 5-fluorouracil-based chemotherapy, severe ascites redeveloped without definite metastatic lesion and with negative cytology. The patient expired at approximately 10 months postoperatively due to pulmonary embolism.
Go to : 
The present case featured two unusual findings: cancer deveolpment from remnant distal CBD after choeldochal cyst excision and bilateral ovarian metastases from cholangiocacinoma.
Theoretically, biliary malignancy should not develop after excision of the choledochal cyst because the presumed cause was abrogated by separation-operation. However, although the incidence of biliary malignancy after excision of a choledochal cyst was 0.6% in Korean multicenter study2 and 0.7% in a Japanese nationwide study,3 far lower than that in association with unresected choledochal cysts, it is still approximately 200 times higher than the incidence of biliary cancer in the general population in Japan. According to the author's literature review,4 58 cases were identified between 1970 and 2011. Among them, only 9 cases had malignancy at the intrapancreatic remnant bile duct. The mean interval between cyst excision and cancer detection was 9 years with a range of 4 to 17 years. Because the presenting case developed malignancy only one and half years after cyst excision, it could be a missed lesion but de novo malignancy. However, preoperative endoscopic retrograde cholangiopancreaticography and aspiration biopsy showed no abnormalities. Despite the poor prognosis of the presenting case, since the prognosis of the malignancy associated choledochal cyst was generally comparable with that of cholangiocarcinoma,2 regular follow-up should be done through tumor marker such as serum level of CA19-9 and imaging modalities such as computed tomography or ultrasonography for early detection of subsequent biliary malignancy after cyst excision.
Metastatic cancers in the ovary are relatively uncommon, accounitng for only about 3-5% of ovarian tumors.15 Although ovarian metastatic tumors ar typically bilateral, small (<10 cm), nodular, and solid,25 it is not easy to differentiate primary tumors from metastatic tumors. The present case showed bilateral, small and solid ovaries in preoperative imaging studies suggesting the presence of metastatic ovarian tumors. Since there was no guideline for the treatment of metastatic ovarian tumors from cholangiocarcinoma, pylorus preserving pancreaticoduodenectomy and bilateral salphingo-oophorectomy with hysterectomy were performed. The management of primary ovarian cancer includes maximum tumor volume reduction, which is advantageous for survival.6 However, very few cases documenting ovarian metastases from cholangiocarcinoma have been reported in the literature,78 so the benefit of ovarian metastatectomy remains to be elucidated. Bilateral oophorectomy for ovarian metastasis from colorectal cancer has a positive impact on disease-free and overall survival in isolated ovarian metastases patients in an Italian study.9 Also, for patients with gastric cancer, a Korean study suggested that debulking or gastrectomy plus metastasectomy may confer survival benefits on patients with distant metastases who are receiving systemic chemotherapy.10 However, since the prognosis of ovarian metastasis is dismal, and the benefit of ovarian metastatectomy is limited, further investigation is needed.
The present case is the first reported case of ovarian metastasis from cholangiocarcinoma associated with a choledochal cyst. Since biliary malignancy could develop within a relatively short period after choledochal cyst excision, regular follow-up should be done for early detection of subsequent biliary malignancy after cyst excision. Although most reported cases with ovarian metastasis from cholangiocarcinoma were treated with bilateral salphigo-oophorectomy, the benefit of ovarian metastatectomy is uncertain and should be investigated.
Go to : 
References
1. Holtz F, Hart WR. Krukenberg tumors of the ovary: a clinicopathologic analysis of 27 cases. Cancer. 1982; 50:2438–2447. PMID: 6291740.

2. Lee SE, Jang JY, Lee YJ, Choi DW, Lee WJ, Cho BH, et al. Korean Pancreas Surgery Club. Choledochal cyst and associated malignant tumors in adults: a multicenter survey in South Korea. Arch Surg. 2011; 146:1178–1184. PMID: 22006877.
3. Watanabe Y, Toki A, Todani T. Bile duct cancer developed after cyst excision for choledochal cyst. J Hepatobiliary Pancreat Surg. 1999; 6:207–212. PMID: 10526053.

4. Lee SE, Jang JY. Development of biliary malignancy after cyst excision for congenital choledochal cysts: what should we do? J Gastroenterol Hepatol. 2013; 28:210–212. PMID: 23339386.

5. Lee KR, Young RH. The distinction between primary and metastatic mucinous carcinomas of the ovary: gross and histologic findings in 50 cases. Am J Surg Pathol. 2003; 27:281–292. PMID: 12604884.
6. Fader AN, Rose PG. Role of surgery in ovarian carcinoma. J Clin Oncol. 2007; 25:2873–2883. PMID: 17617518.

7. Young RH, Scully RE. Ovarian metastases from carcinoma of the gallbladder and extrahepatic bile ducts simulating primary tumors of the ovary. A report of six cases. Int J Gynecol Pathol. 1990; 9:60–72. PMID: 2294064.
8. Khunamornpong S, Lerwill MF, Siriaunkgul S, Suprasert P, Pojchamarnwiputh S, Chiangmai WN, et al. Carcinoma of extrahepatic bile ducts and gallbladder metastatic to the ovary: a report of 16 cases. Int J Gynecol Pathol. 2008; 27:366–379. PMID: 18580314.

9. Erroi F, Scarpa M, Angriman I, Cecchetto A, Pasetto L, Mollica E, et al. Ovarian metastasis from colorectal cancer: prognostic value of radical oophorectomy. J Surg Oncol. 2007; 96:113–117. PMID: 17443728.

10. Kim KH, Lee KW, Baek SK, Chang HJ, Kim YJ, Park do J, et al. Survival benefit of gastrectomy ± metastasectomy in patients with metastatic gastric cancer receiving chemotherapy. Gastric Cancer. 2011; 14:130–138. PMID: 21373855.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download