Abstract
The wall of normal proximal bile duct is occasionally thin with close approximation to the right hepatic artery. Thus, isolation of this hepatic artery can result in excessive weakening of the remnant proximal bile duct wall during hemiliver graft harvest. This type of injury can induce ischemic stricture of the donor common bile duct. This study aimed to review the clinical sequences of such ischemic type donor bile duct injuries primarily managed with endoscopic and radiological interventional treatments. A retrospective review of medical records was performed for two living donors who suffered from ischemic type donor bile duct injury. They were followed up for more than 10 years. The right and left liver grafts were harvested from these two donors. Bile duct anatomy was normal bifurcation in one and anomalous branching in the other. Bile duct stenosis was detected in them at 2 weeks and 1 week after liver donation. They underwent endoscopic balloon dilatation and temporary stent (endoscopic retrograde biliary drainage tube) insertion. After keeping the tube for 2 months, the tube was successfully removed in one donor. However, endoscopic treatment was not successful, thus additional radiological intervention was necessary in the other donor. On follow-up over 10 years, they are doing well so far with no recurrence of biliary stricture. Based on our limited experience, interventional treatment with subsequent long-term follow-up appears to be an essential and choice treatment for ischemic type biliary stricture occurring in liver living donors.
Transection of graft bile duct is a crucial step in living donor hepatectomy. Multiple small ducts can make the biliary reconstruction more difficult. In addition, they may influence the outcome in the recipient. Furthermore, they might lead to iatrogenic injury of the donor biliary system with subsequent early or late complications.1 Biliary leakage, biloma formation, and biliary stricture are well recognized donor complications that might be directly linked to bile duct division. Biliary complications constitute the majority of the clinically significant donor complications.23 The wall of normal proximal bile duct is often thin with close approximation to the right hepatic artery. Thus, isolation of this hepatic artery can result in excessive thinning of the remnant proximal bile duct wall during hemiliver graft harvest. This type of injury can induce ischemic stricture of the donor common bile duct, especially when a very short duct stump is left after bile duct transection.
This study intended to review the clinical sequences of such ischemic type donor bile duct injuries primarily managed with endoscopic and radiological interventional treatments. A retrospective review of medical records was performed for two living donors who had suffered from ischemic type donor bile duct injury. They were followed up for more than 10 years.
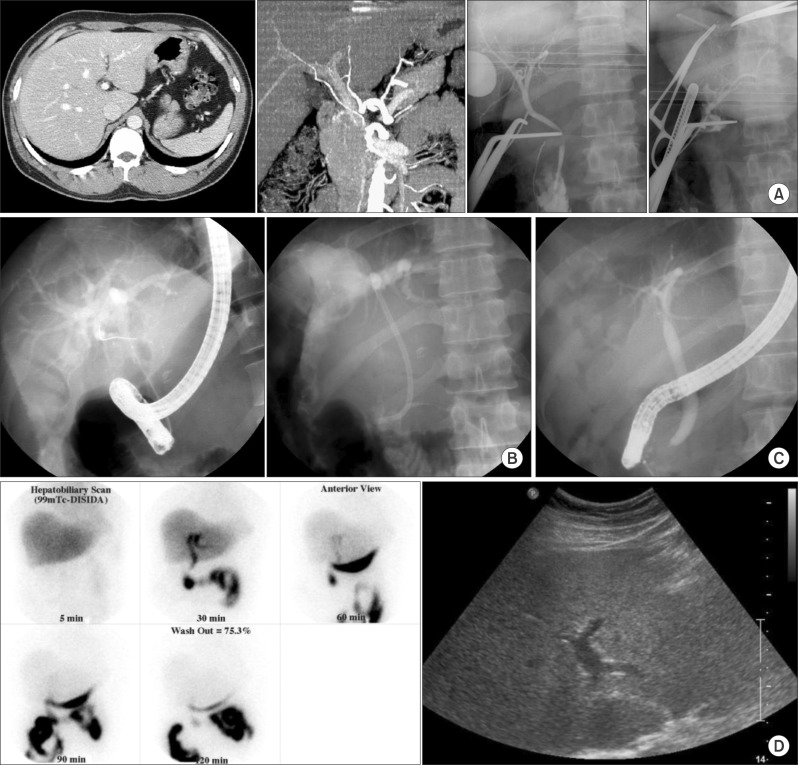
The donor was a 33-year-old son of the recipient. He donated his right liver in November 2000. The remnant left liver volume was 34% of the total liver volume. The donor had a replacing right hepatic artery from the superior mesenteric artery. This right hepatic artery was firmly attached to the bile duct. Thus, extensive dissection was necessary to isolate this hepatic artery from the bile duct. Unusual right liver graft harvest was performed. Completion intraoperative cholangiogram showed no abnormal findings (Fig. 1A). The patient was discharged uneventfully. However, at 14 days after the surgery, the patient visited an outpatient clinic with obstructive jaundice detected. After confirmation of intrahepatic duct dilatation on computed tomography (CT) follow-up, endoscopic retrograde cholangiography (ERC) showed diffuse stenosis of the common bile duct. Endoscopic balloon dilatation was carried out and a temporary stent (endoscopic retrograde biliary drainage [ERBD]) was inserted (Fig. 1B). After 2 months, the biliary stenosis disappeared completely. Thus, the ERBD tube was removed (Fig. 1C). The patient was followed up regularly for more than 10 years. The last follow-up was performed in August 2012, in which the donor showed completely normal liver function with only mild intrahepatic ductal dilatation on liver ultrasonography (Fig. 1D).
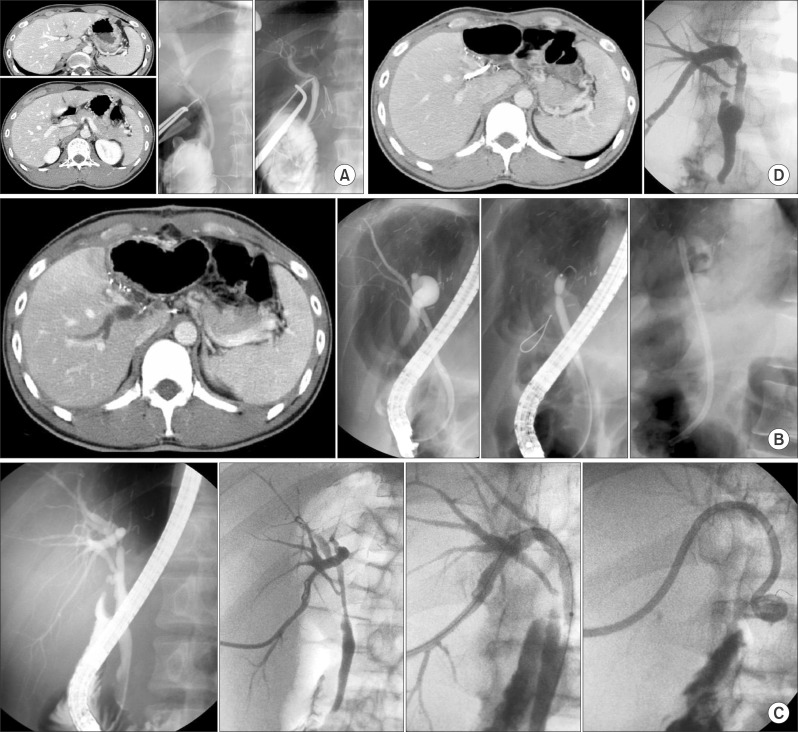
The donor was a 27-year-old son of the recipient. He donated his left liver in January 2001. The donor had a type III portal vein anomaly with definitely variant bile duct configuration. Thus, the hilar bile duct was dissected extensively to prevent iatrogenic bile duct injury during graft bile duct transection. Usual left liver graft harvest was performed. Completion intraoperative cholangiogram showed no abnormal findings (Fig. 2A). However, at routine postoperative follow-up CT at 7 days, dilatation of the right posterior hepatic duct was detected without disturbance of liver function. Diffuse stenosis of the proximal right posterior duct and common bile duct were visualized on ERC. Thus, endoscopic balloon dilatation and ERBD tube insertion were performed (Fig. 2B). Since significant bile duct stenosis were left after two sessions of ERBD tube change for 4 months, a percutaneous transhepatic biliary drainage (PTBD) tube was finally inserted at 4 months after surgery (Fig. 2C). The PTBD tube was changed three times with serial dilatation and finally removed at 10 months after surgery (Fig. 2D). Although focal stenotic configuration of the bile duct was left, the patient showed completely normal function for more than 10 years after interventional treatment without recurrence of biliary stricture.
Living donor liver transplantation has been established as a primary treatment for end-stage liver disease and an alternative to deceased donor liver transplantation. Postoperative donor complications are inevitable in general. Several high-volume studies showed that living donor complications continued to happen despite the passage of time needed for the learning curve.123 Biliary complications constitute the majority of significant complications following donor hepatectomy. They represent approximately 20% to 30% of total complications.45
Donor biliary complications can be classified as biliary leak and stricture. A recent review estimated that the average incidences of bile leak and biliary stricture were 4.2% and 0.8%, respectively.4 Sultan et al.5 report a 12.5% incidence of biliary leak without biliary stricture. Gruttadauria et al.6 reported no biliary stricture and a 9.33% rate of biliary leak. Ghobrial et al.7 reported a 0.5% rate of biliary stricture and a 9.2% rate of biliary leak. Kim et al.2 reported that 7.6% of donors experienced biliary leak, with biliary stricture in 2.6% of donors, all of which required intervention. Shin et al.1 reported a 1.2% rate of biliary leak and a 0.7% rate of biliary stricture in 827 donors. We have reported an overall major donor complication of 1.3% after learning curve in our first 1000 cases of living donor liver transplantation.8
In literature and our practice after performing more than 4,000 cases of living donor hepatectomy, most donor biliary strictures are closely associated with bile duct transection site and surgical technique. However, ischemic type biliary stricture happens sporadically as shown in this study. If any anomalous anatomy is accompanied in hilar biliary and vascular structures, special attention should be paid to avoid unusual surgical complications. The most important point is that the donor bile duct should be handled minimally in any situation. As surgical experience accumulates, we no longer need to dissect the long segment of the common bile duct as we did in our first case in this study because any short stump of the graft right hepatic artery can be reconstructed securely.
Simple ischemic type donor bile duct stricture appears to be readily manageable with endoscopic intervention as shown in our first case in this study. However, when combined with variant biliary anatomy, its treatment would be more demanding as in our second case in this study. Based on our experience, interventional treatment with subsequent long-term follow-up appears to be an essential choice treatment for ischemic type biliary stricture occurred in liver living donors.
References
1. Shin M, Song S, Kim JM, Kwon CH, Kim SJ, Lee SK, et al. Donor morbidity including biliary complications in living-donor liver transplantation: single-center analysis of 827 cases. Transplantation. 2012; 93:942–948. PMID: 22357173.
2. Kim SJ, Na GH, Choi HJ, Yoo YK, Kim DG. Surgical outcome of right liver donors in living donor liver transplantation: single-center experience with 500 cases. J Gastrointest Surg. 2012; 16:1160–1170. PMID: 22426687.

3. Yi NJ, Suh KS, Cho JY, Lee HW, Cho EH, Yang SH, et al. Three-quarters of right liver donors experienced postoperative complications. Liver Transpl. 2007; 13:797–806. PMID: 17539000.

4. Yuan Y, Gotoh M. Biliary complications in living liver donors. Surg Today. 2010; 40:411–417. PMID: 20425542.

5. Sultan AM, Salah T, Elshobary MM, Fathy OM, Elghawalby AN, Yassen AM, et al. Biliary complications in living donor right hepatectomy are affected by the method of bile duct division. Liver Transpl. 2014; 20:1393–1401. PMID: 25060964.

6. Gruttadauria S, Marsh JW, Vizzini GB, di Francesco F, Luca A, Volpes R, et al. Analysis of surgical and perioperative complications in seventy-five right hepatectomies for living donor liver transplantation. World J Gastroenterol. 2008; 14:3159–3164. PMID: 18506919.

7. Ghobrial RM, Freise CE, Trotter JF, Tong L, Ojo AO, Fair JH, et al. Donor morbidity after living donation for liver transplantation. Gastroenterology. 2008; 135:468–476. PMID: 18505689.

8. Hwang S, Lee SG, Lee YJ, Sung KB, Park KM, Kim KH, et al. Lessons learned from 1,000 living donor liver transplantations in a single center: how to make living donations safe. Liver Transpl. 2006; 12:920–927. PMID: 16721780.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download