1. Trede M, Schwall G. The complications of pancreatectomy. Ann Surg. 1988; 207:39–47. PMID:
3276272.

2. Miedema BW, Sarr MG, van Heerden JA, Nagorney DM, McIlrath DC, Ilstrup D. Complications following pancreaticoduodenectomy. Current management. Arch Surg. 1992; 127:945–949. PMID:
1353671.
3. Yeo CJ. Management of complications following pancreaticoduodenectomy. Surg Clin North Am. 1995; 75:913–924. PMID:
7660254.
4. Aranha GV, Aaron JM, Shoup M, Pickleman J. Current management of pancreatic fistula after pancreaticoduodenectomy. Surgery. 2006; 140:561–568. PMID:
17011903.

5. Goldsmith HS, Ghosh BC, Huvos AG. Ligation versus implantation of the pancreatic duct after pancreaticoduodenectomy. Surg Gynecol Obstet. 1971; 132:87–92. PMID:
5538818.
6. Di Carlo V, Chiesa R, Pontiroli AE, Carlucci M, Staudacher C, Zerbi A, et al. Pancreatoduodenectomy with occlusion of the residual stump by Neoprene injection. World J Surg. 1989; 13:105–110. PMID:
2543144.

7. Suc B, Msika S, Fingerhut A, Fourtanier G, Hay JM, Holmières F, et al. French Associations for Surgical Research. Temporary fibrin glue occlusion of the main pancreatic duct in the prevention of intra-abdominal complications after pancreatic resection: prospective randomized trial. Ann Surg. 2003; 237:57–65. PMID:
12496531.
8. Lillemoe KD, Cameron JL, Kim MP, Campbell KA, Sauter PK, Coleman JA, et al. Does fibrin glue sealant decrease the rate of pancreatic fistula after pancreaticoduodenectomy? Results of a prospective randomized trial. J Gastrointest Surg. 2004; 8:766–772. PMID:
15531229.

9. Büchler M, Friess H, Klempa I, Hermanek P, Sulkowski U, Becker H, et al. Role of octreotide in the prevention of postoperative complications following pancreatic resection. Am J Surg. 1992; 163:125–130. PMID:
1733360.

10. Pederzoli P, Bassi C, Falconi M, Camboni MG. Efficacy of octreotide in the prevention of complications of elective pancreatic surgery. Italian Study Group. Br J Surg. 1994; 81:265–269. PMID:
8156354.
11. Strasberg SM, Drebin JA, Mokadam NA, Green DW, Jones KL, Ehlers JP, et al. Prospective trial of a blood supply-based technique of pancreaticojejunostomy: effect on anastomotic failure in the Whipple procedure. J Am Coll Surg. 2002; 194:746–758. PMID:
12081065.
12. Aranha GV, Hodul P, Golts E, Oh D, Pickleman J, Creech S. A comparison of pancreaticogastrostomy and pancreaticojejunostomy following pancreaticoduodenectomy. J Gastrointest Surg. 2003; 7:672–682. PMID:
12850681.

13. Hwang S, Ha TY, Kim JS, Cheong O, Kim KH, Lee SG. Clinical application of sution-type cigarette drain for hepatopancreatoabiliary surgery. J Korean Surg Soc. 2004; 67:428–431.
14. Bassi C, Falconi M, Molinari E, Mantovani W, Butturini G, Gumbs AA, et al. Duct-to-mucosa versus end-to-side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy: results of a prospective randomized trial. Surgery. 2003; 134:766–771. PMID:
14639354.

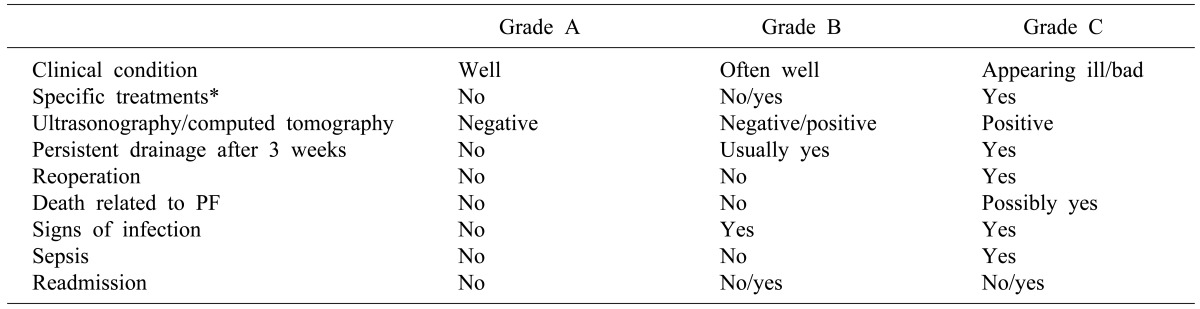
15. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13. PMID:
16003309.

16. Facy O, Chalumeau C, Poussier M, Binquet C, Rat P, Ortega-Deballon P. Diagnosis of postoperative pancreatic fistula. Br J Surg. 2012; 99:1072–1075. PMID:
22539219.

17. Jung DH, Hwang S, Lee SG. An analysis on the amount of excreted pancreatic juice after pancreatoduodenectomy. Korean J Gastroenterol. 2004; 43:309–315. PMID:
15156118.
18. Yoo D, Hwang S, Kim KH, Ahn CS, Moon DB, Ha TY, et al. Pancreatic atrophy relative to external versus internal drainage of the pancreatic duct after pylorus-preserving pancreaticoduodenectomy. J Gastrointest Surg. 2014; 18:1604–1609. PMID:
25002021.

19. El Nakeeb A, Salah T, Sultan A, El Hemaly M, Askr W, Ezzat H, et al. Pancreatic anastomotic leakage after pancreaticoduodenectomy. Risk factors, clinical predictors, and management (single center experience). World J Surg. 2013; 37:1405–1418. PMID:
23494109.

20. Strasberg SM, Drebin JA, Soper NJ. Evolution and current status of the Whipple procedure: an update for gastroenterologists. Gastroenterology. 1997; 113:983–994. PMID:
9287993.

21. Kim JH, Yoo BM, Kim JH, Kim WH. Which method should we select for pancreatic anastomosis after pancreaticoduodenectomy? World J Surg. 2009; 33:326–332. PMID:
19057947.

22. Hong S, Wang H, Yang S, Yang K. External stent versus no stent for pancreaticojejunostomy: a meta-analysis of randomized controlled trials. J Gastrointest Surg. 2013; 17:1516–1525. PMID:
23568149.

23. Motoi F, Egawa S, Rikiyama T, Katayose Y, Unno M. Randomized clinical trial of external stent drainage of the pancreatic duct to reduce postoperative pancreatic fistula after pancreaticojejunostomy. Br J Surg. 2012; 99:524–531. PMID:
22497024.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download