1. Fukatsu S, Yano I, Igarashi T, Hashida T, Takayanagi K, Saito H, et al. Population pharmacokinetics of tacrolimus in adult recipients receiving living-donor liver transplantation. Eur J Clin Pharmacol. 2001; 57:479–484. PMID:
11699612.
2. Fukudo M, Yano I, Fukatsu S, Saito H, Uemoto S, Kiuchi T, et al. Forecasting of blood tacrolimus concentrations based on the Bayesian method in adult patients receiving living-donor liver transplantation. Clin Pharmacokinet. 2003; 42:1161–1178. PMID:
14531726.

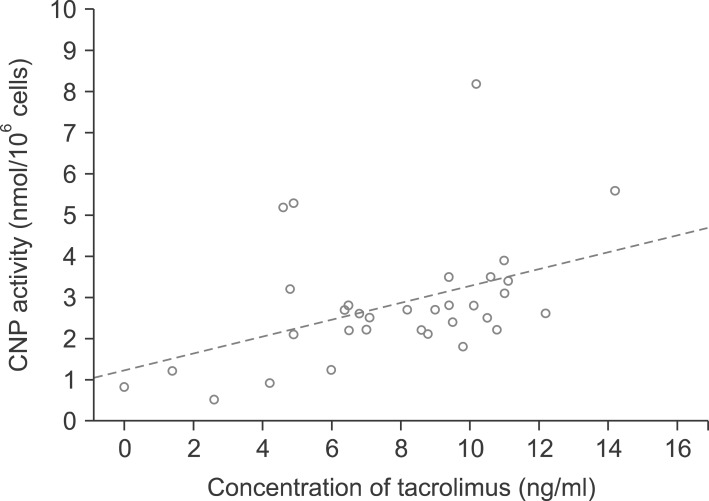
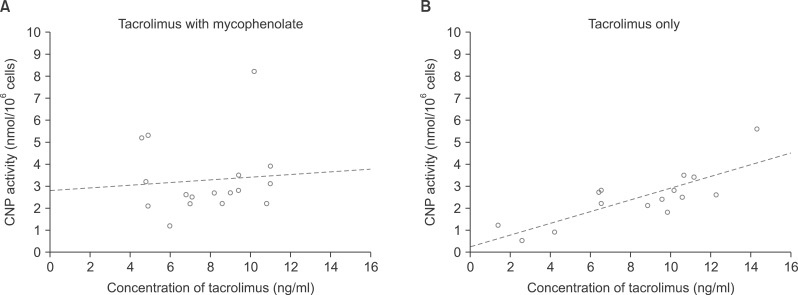
3. Fukudo M, Yano I, Masuda S, Fukatsu S, Katsura T, Ogura Y, et al. Pharmacodynamic analysis of tacrolimus and cyclosporine in living-donor liver transplant patients. Clin Pharmacol Ther. 2005; 78:168–181. PMID:
16084851.

4. Liu XQ, Hu ZQ, Pei YF, Tao R. Clinical operational tolerance in liver transplantation: state-of-the-art perspective and future prospects. Hepatobiliary Pancreat Dis Int. 2013; 12:12–33. PMID:
23392795.

5. de la Garza RG, Sarobe P, Merino J, Lasarte JJ, D'Avola D, Belsue V, et al. Trial of complete weaning from immunosuppression for liver transplant recipients: factors predictive of tolerance. Liver Transpl. 2013; 19:937–944. PMID:
23784747.

6. Londoño MC, Rimola A, O'Grady J, Sanchez-Fueyo A. Immunosuppression minimization vs. complete drug withdrawal in liver transplantation. J Hepatol. 2013; 59:872–879. PMID:
23578883.

7. Benítez C, Londoño MC, Miquel R, Manzia TM, Abraldes JG, Lozano JJ, et al. Prospective multicenter clinical trial of immunosuppressive drug withdrawal in stable adult liver transplant recipients. Hepatology. 2013; 58:1824–1835. PMID:
23532679.

8. Bohne F, Martínez-Llordella M, Lozano JJ, Miquel R, Benítez C, Londoño MC, et al. Intra-graft expression of genes involved in iron homeostasis predicts the development of operational tolerance in human liver transplantation. J Clin Invest. 2012; 122:368–382. PMID:
22156196.

9. Fukudo M, Yano I, Masuda S, Okuda M, Inui K. Distinct inhibitory effects of tacrolimus and cyclosporin a on calcineurin phosphatase activity. J Pharmacol Exp Ther. 2005; 312:816–825. PMID:
15383634.

10. Fukudo M, Yano I, Masuda S, Katsura T, Ogura Y, Oike F, et al. Cyclosporine exposure and calcineurin phosphatase activity in living-donor liver transplant patients: twice daily vs. once daily dosing. Liver Transpl. 2006; 12:292–300. PMID:
16447186.

11. Kung L, Halloran PF. Immunophilins may limit calcineurin inhibition by cyclosporine and tacrolimus at high drug concentrations. Transplantation. 2000; 70:327–335. PMID:
10933159.
12. Hwang S, Kim KH, Song GW, Yu YD, Park GC, Kim KW, et al. Peritransplant monitoring of immune cell function in adult living donor liver transplantation. Transplant Proc. 2010; 42:2567–2571. PMID:
20832545.

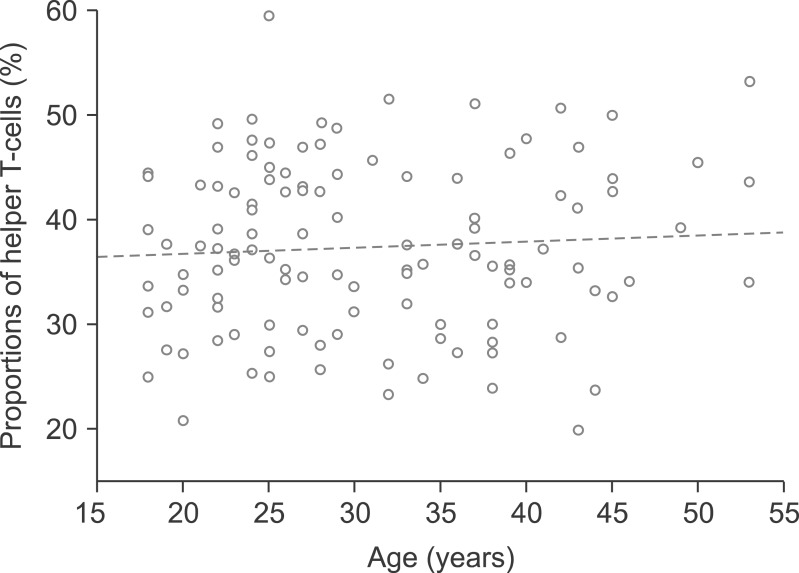
13. van Rossum HH, Romijn FP, Sellar KJ, Smit NP, van der Boog PJ, de Fijter JW, et al. Variation in leukocyte subset concentrations affects calcineurin activity measurement: implications for pharmacodynamic monitoring strategies. Clin Chem. 2008; 54:517–524. PMID:
18218723.

14. Blanchet B, Duvoux C, Costentin CE, Barrault C, Ghaleh B, Salvat A, et al. Pharmacokinetic-pharmacodynamic assessment of tacrolimus in liver-transplant recipients during the early post-transplantation period. Ther Drug Monit. 2008; 30:412–418. PMID:
18641556.

15. Yano I. Pharmacodynamic monitoring of calcineurin phosphatase activity in transplant patients treated with calcineurin inhibitors. Drug Metab Pharmacokinet. 2008; 23:150–157. PMID:
18574318.

16. Cremers S, Schoemaker R, Scholten E, den Hartigh J, König-Quartel J, van Kan E, et al. Characterizing the role of enterohepatic recycling in the interactions between mycophenolate mofetil and calcineurin inhibitors in renal transplant patients by pharmacokinetic modelling. Br J Clin Pharmacol. 2005; 60:249–256. PMID:
16120063.

17. Tredger JM, Brown NW, Adams J, Gonde CE, Dhawan A, Rela M, et al. Monitoring mycophenolate in liver transplant recipients: toward a therapeutic range. Liver Transpl. 2004; 10:492–502. PMID:
15048791.

18. Pisupati J, Jain A, Burckart G, Hamad I, Zuckerman S, Fung J, et al. Intraindividual and interindividual variations in the pharmacokinetics of mycophenolic acid in liver transplant patients. J Clin Pharmacol. 2005; 45:34–41. PMID:
15601803.

19. Brown NW, Aw MM, Mieli-Vergani G, Dhawan A, Tredger JM. Mycophenolic acid and mycophenolic acid glucuronide pharmacokinetics in pediatric liver transplant recipients: effect of cyclosporine and tacrolimus comedication. Ther Drug Monit. 2002; 24:598–606. PMID:
12352931.

20. Hesselink DA, van Hest RM, Mathot RA, Bonthuis F, Weimar W, de Bruin RW, et al. Cyclosporine interacts with mycophenolic acid by inhibiting the multidrug resistance-associated protein 2. Am J Transplant. 2005; 5:987–994. PMID:
15816878.

21. Kowalski R, Post D, Schneider MC, Britz J, Thomas J, Deierhoi M, et al. Immune cell function testing: an adjunct to therapeutic drug monitoring in transplant patient management. Clin Transplant. 2003; 17:77–88. PMID:
12709071.

22. Rodrigo E, López-Hoyos M, Corral M, Fábrega E, Fernández-Fresnedo G, San Segundo D, et al. ImmuKnow as a diagnostic tool for predicting infection and acute rejection in adult liver transplant recipients: a systematic review and meta-analysis. Liver Transpl. 2012; 18:1245–1253. PMID:
22740321.

23. Ravaioli M, Neri F, Lazzarotto T, Bertuzzo VR, Di Gioia P, Stacchini G, et al. Immunosuppression Modifications Based on an Immune Response Assay: Results of a Randomized, Controlled Trial. Transplantation. 2015; 99:1625–1632. PMID:
25757214.
24. Kang SH, Hwang S, Ha TY, Song GW, Jung DH, Kim KH, et al. Tailored long-term immunosuppressive regimen for adult liver transplant recipients with hepatocellular carcinoma. Korean J Hepatobiliary Pancreat Surg. 2014; 18:48–51. PMID:
26155248.







 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download