Abstract
Backgrounds/Aims
Standard liver volume (SLV) is an important parameter that has been used as a reference value to estimate the graft matching in living donor liver transplantation (LDLT). This study aimed to determine a reliable SLV formula for Korean adult patients as compared with the 15 SLV formulae from other studies and further estimate SLV formula by gender and body mass index (BMI).
Methods
Computed tomography liver volumetry was performed in 1,000 living donors for LDLT and regression formulae for SLV was calculated. Individual donor data were applied to the 15 previously published SLV formulae, as compared with the SLV formula derived in this study. Analysis for confounding variables of BMI and gender was also performed.
Results
Two formulae, "SLV (ml)=908.204×BSA-464.728" with DuBois body surface area (BSA) formula and "SLV (ml)=893.485×BSA-439.169" with Monsteller BSA formula, were derived by using the profiles of the 1,000 living donors included in the study. Comparison with other 15 other formulae, all except for Chouker formula showed the mean volume percentage errors of 4.8-5.4%. The gender showed no significant effect on total liver volume (TLV), but there was a significant increase in TLV as BMI increased.
Conclusions
Our study suggested that most SLV formulae showed a crudely applicable range of SLV estimation for Korean adults. Considering the volume error in estimating SLV, further SLV studies with larger population from multiple centers should be performed to enhance its predictability. Our results suggested that classifying SLV formulae by BMI and gender is unnecessary.
Go to : 
During the last 3 decades, the demand for liver transplantation (LT) has gradually increased due to expansion of its indications. Because of the relative shortage of deceased donor organs, LT cases using living donor grafts and split grafts have increased to help solve the organ shortage.
The concept of standard liver volume (SLV) emerged after the introduction of living donor LT (LDLT). It is an important parameter that is used as a reference liver volume to estimate the graft size matching, because potential LT recipients' native livers are often shrunken due to advanced liver cirrhosis. Small-for size graft syndrome, which causes graft failure, is a serious complication in LDLT.12 Accurate pretransplant estimation of the recipient SLV is crucial to reduce such graft volume-associated complications. Furthermore, it is important to determine the most suitable formula to predict SLV reliably.
In 1995, Urata et al.2 derived a simple linear equation that estimates SLV by using the body surface area (BSA) of Japanese population without liver abnormalities. Subsequent studies from various countries suggested different formulae that include different factors for SLV, such as body weight, age, height, and gender.
In the present study, based on our institutional high-volume database of LDLT, we attempted primarily to determine a reliable SLV formula for Korean adult patients and compare the equation with SLV formulae from other studies. Secondly, we also assessed the impact of the confounding variables of gender and body mass index (BMI) to determine the difference in the total liver volume (TLV) according to such variables.
Go to : 
A total of consecutive 1,000 living donors (789 males and 211 females) from our institutional database of LDLT, who underwent right or left liver donation between December 2009 and July 2013 were enrolled in the study. Donor demographics (age and sex) and anthropometric data (body weight, body height, and BMI) were recorded at the time of admission for LDLT. Non-Korean donors were excluded from the study.
BSA was calculated by using 2 formulae i.e., the DuBois and Mosteller formulae.3 BSAs obtained from these 2 formulae are very similar each other and thus interchangeable. Mosteller formula is a simplified form of DuBois formula: The equations were as follows:
DuBois formula: BSA (m2)=0.007184×height (cm)0.725×body weight (kg)0.425
Mosteller formula: BSA (m2)=[body weight (kg)×height (cm)/3600]1/2
BMI was calculated as body weight (kg) divided by [height (m)]2 (BMI=kg/m2). Using the World Health Organization (WHO) standard for Asian populations,4 donors were categorized as underweight (BMI<18.5 kg/m2), normal and overweight (18.5 kg/m2≤BMI<25.0 kg/m2), and obese (BMI≥25.0 kg/m2). TLV was measured by computed tomography (CT) volumetry using 3-mm-thick dynamic, contrast-enhanced, multidetector CT images. The CT images were stored in the Picture Archiving and Communication System (PACS; Petavision2, Asan Medical Center, Seoul, Korea), enabling image processing and various measurements, including liver volumetry. Volumes of the right liver, left liver, and caudate lobe were measured separately by using the portal-phase CT images.
After testing for normal distribution using kurtosis and skewness tests, continuous numeric variables were expressed as mean and standard deviation (SD), and median and range. Scatter plots with fitted lines were used to illustrate the correlation between TLV and BSA. Simple linear regression analysis was presented with a regression equation, correlation coefficient (r), and coefficient of determination (r2). Significance between BMI group stratifications was determined by Kruskal-Wallis test. The estimated standard TLV calculated by using each of previously published formula was compared with the calculated liver volume of each donor by 2-sided paired-sample Student's t test. The statistical significance was set at p-value<0.05 for all tests. Statistical analyses were performed with SPSS version 18.0 (SPSS Inc., Chicago).
Go to : 
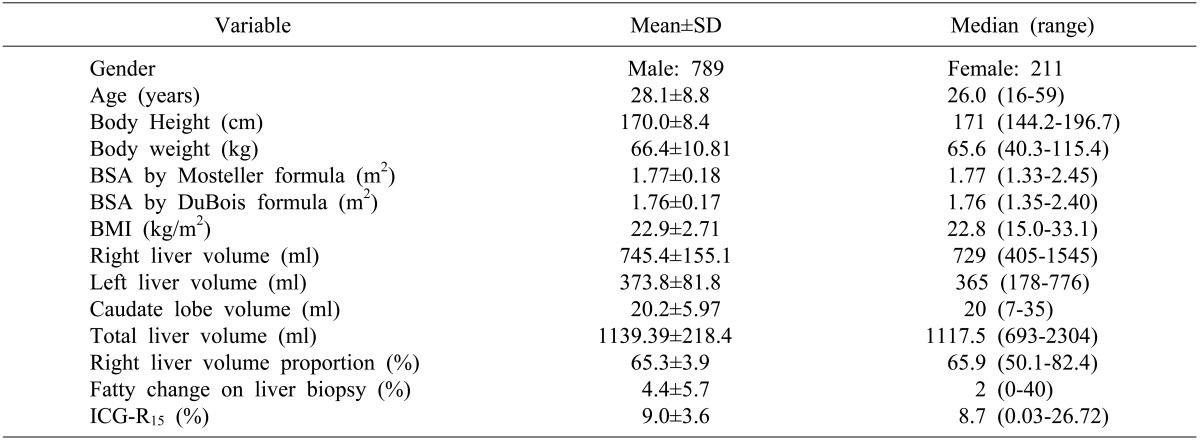
The demographic and anthropometric profiles of the 1,000 living donors were summarized in Table 1. The majority of the donors were male (79.7%) between 20 to 30 years of age (72% were within the range of 20-39 years). Of them, 77% of the donors were normal to overweight (BMI=18.5-24.9 kg/m2) and 19.7% were obese (BMI over 25 kg/m2). At the time of surgery, right liver grafts (88.1%) were used more frequently than left liver grafts (11.9%).
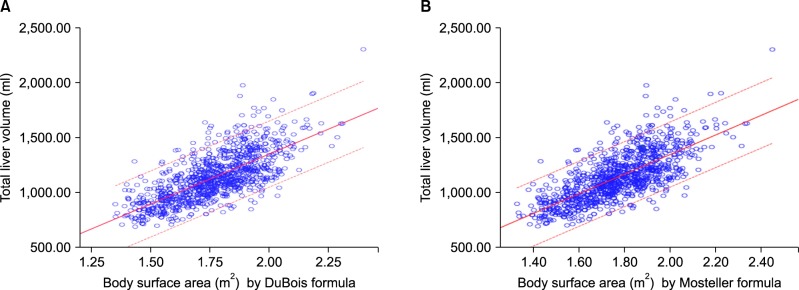
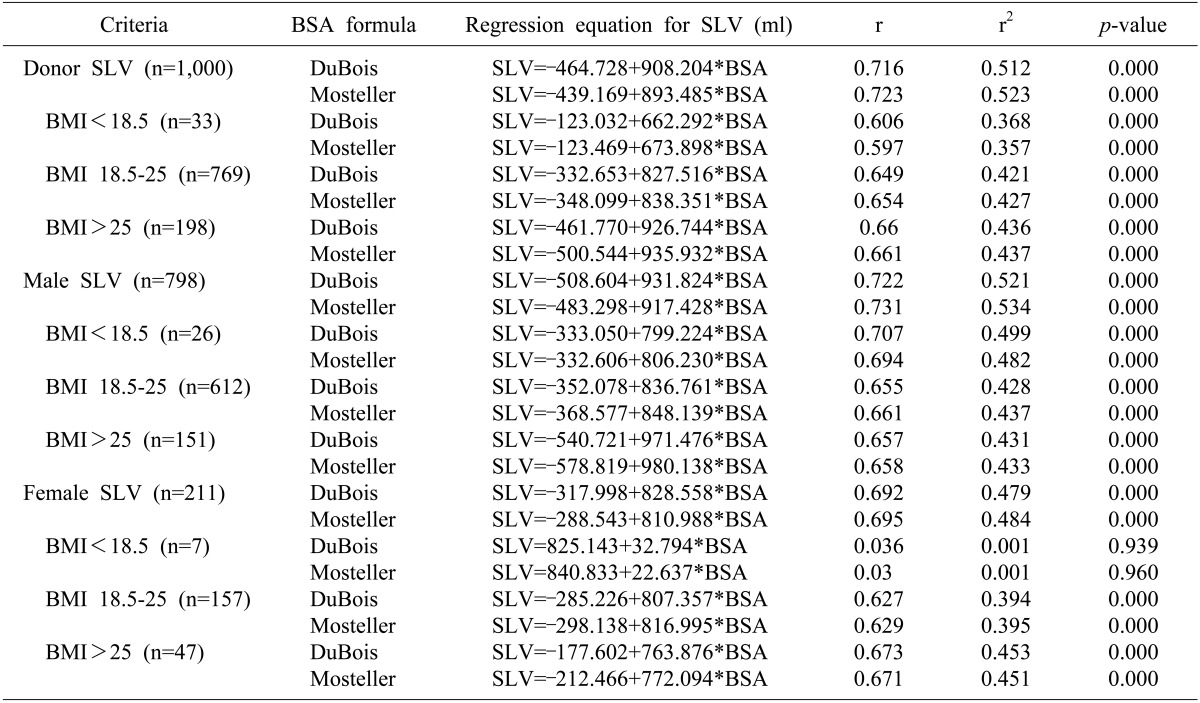
The median values of BSA according to the Mosteller and DuBois formulae were 1.77 m2 and 1.76 m2, respectively, and showed no difference between the 2 equations (p=0.338). The median values of TLV and TLV per BSA (standardized TLV) were 1117.5 ml and 632.4 ml/m2 on Mosteller formula and 631.8 ml/m2 on DuBois formula, respectively. The mean volume of the right liver was 745.4±155.1 ml and occupied 65.2% of the whole liver. The correlation between TLV and BSA according to both Mosteller and DuBois formulae (Fig. 1) with the regression equation for SLV was depicted in Table 2. The regression equation for SLV was further divided according to gender and BMI.
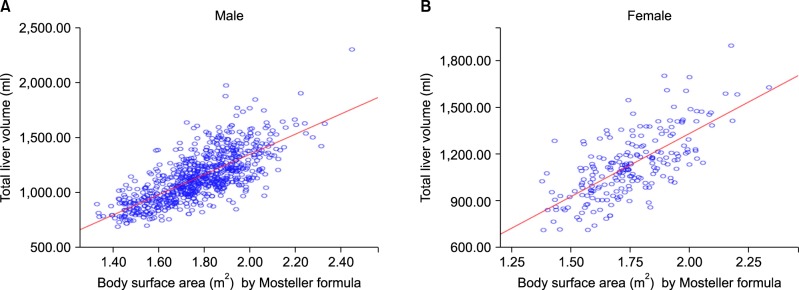
The mean standardized TLV between two genders showed no statistically significant difference (641.9±87.7 ml/m2 in male and 644.4±87.4 ml/m2 in female; p=0.716). Analyzing according to BMI, the mean standardized TLV showed statistically significant differences (590.7±64.1 ml/m2 for BMI<18.5, 636.6±86.0 ml/m2 for BMI 18.5-24.9, and 673.8±88.6 ml/m2 for BMI≥25; p=0.000), indicating that individuals with a higher BMI have a larger liver. In male donors, the correlation among standardized mean TLV and BMI showed statistically significant differences (589.3±61.4 ml/m2 for BMI<18.5, 635.2±84.8 ml/m2 for BMI 18.5-24.9, and 678.3±92.5 ml/m2 for BMI≥25; p=0.000). In contrast, female donors had no significant difference in the liver size with increases in BMI (596.2±77.9 ml/m2 for BMI<18.5, 642.0±91.0 ml/m2 for BMI 18.5-24.9, and 659.5±73.4 ml/m2 for BMI≥25; p=0.082) (Fig. 2).
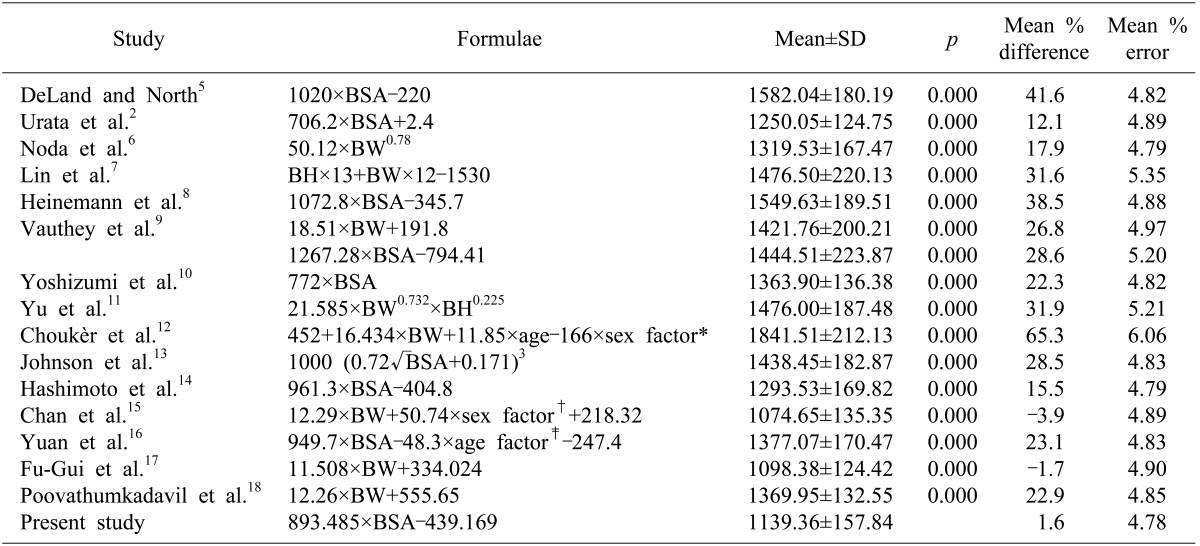
Based on the anthropometric data, the liver volumes were calculated with previously published formulae (Table 3).256789101112131415161718 Comparing with the individual TLVs of our donors' data, our formula resulted in a mean percentage of volume difference [(SLV-individual TLV)/individual TLV)×100%] of 1.6±12.9% and a mean percentage of volume error (absolute value of percentage of volume difference) of 4.8%. Appling our donor profiles to the other 16 formulae, the mean percentage of volume error was greater, ranging from 4.8% to 6.1%. The mean proportions of volume difference calculated using these formulae ranged from -3.9% to 65.3%. The Chan formula resulted in the most underestimation and the Chouker formula in the most overestimation. In comparison, Yu formula, another formula that used Korean population's data resulted in overestimation by a mean percentage volume error of 5.2%.
Go to : 
Improvement in the preoperative evaluation for LDLT resulted in better outcome in recipient side and reduced donor complications. The introduction of SLV by Urata et al.2 in 1995 contributed to the evaluation of LDLT. Currently, there are several published formulae for SLV estimation. Applying the donor data from this study to the previously published formulae indicated that Chan and Fu-Gui formulae underestimated the TLV while all the other formulae overestimated it. Except for Chouker formula, that showed 6.1% of mean percentage volume error, the mean percentage volume error using other formulae ranged from 4.8% to 5.4%. The use of our formula resulted in mean percentage volume error of 4.8%, while the other formulae also yielded crudely acceptable SLV estimation for Korean adults.
Yu formula, derived from the data of Korean population in 2004,11 overestimated the volume by 5.2% of mean percentage volume error. This difference might derive from the postmortem calculations of liver weight of children to adults, because in children, the liver volume/body weight ratio increases as age decreases. There also might be some non-negligible differences between postmortem liver weight and CT volumetry.
Subdividing individual TLV by the gender showed no difference between the 2 genders. The SLV formulae derived by each gender showed mean percentage volume error for male and female as 5.3% and 14.3%, respectively, indicating that the total donor SLV formulae have a higher accuracy in estimating SLV than dividing by the gender. Individual TLV stratified according to BMI showed that higher BMI have larger liver, and the regression formulae for underweight had mean percentage error of 5.4%, but normal and overweight was >10% (10.3% and 16.6%, respectively). Further subdividing by gender and BMI, except for male obese donors, showed mean percentage error of >10%. These results indicated that a specific formula for each criterion is inefficient and incorrect, as compared to that derived from a larger population study.
Recently, we reported another SLV formula using data of 2,155 living donors as "SLV (ml)=-456.3+969.8×BSA".19 This formula differed slightly from the formula of the present study, although the sample number was sufficiently large in our precedent and present studies.
One of the limitations of this study was the relative lack of female donor data. Standard TLV between genders showed no significant difference; however, in actuality, males tend to donate more often in the Korean culture.
In conclusion, our study suggested that nearly all formulae except Chouker formula show a crudely applicable range of SLV estimation for Korean adults. Considering the volume error in estimating SLV, further SLV studies with larger population from multiple centers should be performed to enhance its predictability. Our results also suggested that classifying SLV formulae by BMI and gender is unnecessary.
Go to : 
References
1. Pomposelli JJ, Tongyoo A, Wald C, Pomfret EA. Variability of standard liver volume estimation versus software-assisted total liver volume measurement. Liver Transpl. 2012; 18:1083–1092. PMID: 22532341.

2. Urata K, Kawasaki S, Matsunami H, Hashikura Y, Ikegami T, Ishizone S, et al. Calculation of child and adult standard liver volume for liver transplantation. Hepatology. 1995; 21:1317–1321. PMID: 7737637.

3. Mosteller RD. Simplified calculation of body-surface area. N Engl J Med. 1987; 317:1098. PMID: 3657876.

4. World Health Organization Western Pacific Region, IASO, International Obesity Task Force. Redefining obesity and its treatment. Australia: Health Communications;2000. p. 56.
5. DeLand FH, North WA. Relationship between liver size and body size. Radiology. 1968; 91:1195–1198. PMID: 5699624.

6. Noda T, Todani T, Watanabe Y, Yamamoto S. Liver volume in children measured by computed tomography. Pediatr Radiol. 1997; 27:250–252. PMID: 9126583.

7. Lin XZ, Sun YN, Liu YH, Sheu BS, Cheng BN, Chen CY, et al. Liver volume in patients with or without chronic liver diseases. Hepatogastroenterology. 1998; 45:1069–1074. PMID: 9756008.
8. Heinemann A, Wischhusen F, Püschel K, Rogiers X. Standard liver volume in the Caucasian population. Liver Transpl Surg. 1999; 5:366–368. PMID: 10477836.

9. Vauthey JN, Abdalla EK, Doherty DA, Gertsch P, Fenstermacher MJ, Loyer EM, et al. Body surface area and body weight predict total liver volume in Western adults. Liver Transpl. 2002; 8:233–240. PMID: 11910568.

10. Yoshizumi T, Gondolesi GE, Bodian CA, Jeon H, Schwartz ME, Fishbein TM, et al. A simple new formula to assess liver weight. Transplant Proc. 2003; 35:1415–1420. PMID: 12826175.

11. Yu HC, You H, Lee H, Jin ZW, Moon JI, Cho BH. Estimation of standard liver volume for liver transplantation in the Korean population. Liver Transpl. 2004; 10:779–783. PMID: 15162473.

12. Choukèr A, Martignoni A, Dugas M, Eisenmenger W, Schauer R, Kaufmann I, et al. Estimation of liver size for liver transplantation: the impact of age and gender. Liver Transpl. 2004; 10:678–685. PMID: 15108261.

13. Johnson TN, Tucker GT, Tanner MS, Rostami-Hodjegan A. Changes in liver volume from birth to adulthood: a meta-analysis. Liver Transpl. 2005; 11:1481–1493. PMID: 16315293.

14. Hashimoto T, Sugawara Y, Tamura S, Hasegawa K, Kishi Y, Kokudo N, et al. Estimation of standard liver volume in Japanese living liver donors. J Gastroenterol Hepatol. 2006; 21:1710–1713. PMID: 16984594.

15. Chan SC, Liu CL, Lo CM, Lam BK, Lee EW, Wong Y, et al. Estimating liver weight of adults by body weight and gender. World J Gastroenterol. 2006; 12:2217–2222. PMID: 16610024.

16. Yuan D, Lu T, Wei YG, Li B, Yan LN, Zeng Y, et al. Estimation of standard liver volume for liver transplantation in the Chinese population. Transplant Proc. 2008; 40:3536–3540. PMID: 19100432.

17. Fu-Gui L, Lu-Nan Y, Bo L, Yong Z, Tian-Fu W, Ming-Qing X, et al. Estimation of standard liver volume in Chinese adult living donors. Transplant Proc. 2009; 41:4052–4056. PMID: 20005340.

18. Poovathumkadavil A, Leung KF, Al Ghamdi HM, Othman Iel H, Meshikhes AW. Standard formula for liver volume in Middle Eastern Arabic adults. Transplant Proc. 2010; 42:3600–3605. PMID: 21094823.

19. Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, et al. Quantified risk assessment for major hepatectomy via the indocyanine green clearance rate and liver volumetry combined with standard liver volume. J Gastrointest Surg. 2015; 19:1305–1314. PMID: 25947549.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download