Abstract
Ectopic opening of the pancreatic and bile ducts (EOPBD) into the duodenal bulb is an extremely rare congenital anomaly with unknown clinical implications. We presented a case of gallbladder cancer with EOPBD into the duodenal bulb. A 57-year-old male was referred to our hospital with intermittent right upper abdominal pain. Endoscopic retrograde cholangiopancreatography and magnetic resonance cholangiopancreatography showed individual EOPBD into the duodenal bulb with no papillary structure, and a focal nodular lesion in the gallbladder. A follow-up abdominal computed tomography scan 9 months later revealed a slight increase in the size of the fundal nodule, which was suspected as gallbladder cancer. An intraoperative frozen biopsy identified the nodular lesion as adenocarcinoma involving the cystic duct, and the patient underwent radical cholecystectomy including bile duct resection with hepaticojejunostomy. EOPBD is an extremely rare condition that can be associated with gallbladder malignancy as well as benign disease. Clinicians should follow up carefully and consider surgical treatment for suspected malignant lesions.
Go to : 
The pancreatic and bile ducts form a common channel before opening into the second portion of the duodenum. However, some patients have anomalous opening of the bile and pancreatic ducts into the stomach, pylorus, or third and fourth portion of the duodenum.12345 Ectopic opening of the pancreatic and bile ducts (EOPBD) into the duodenal bulb is an extremely rare congenital anomaly6 that is related to benign biliary disease. There are no reports on the association between EOPBD and malignant disease. We presented a case of gallbladder cancer with EOPBD into the duodenal bulb.
Go to : 
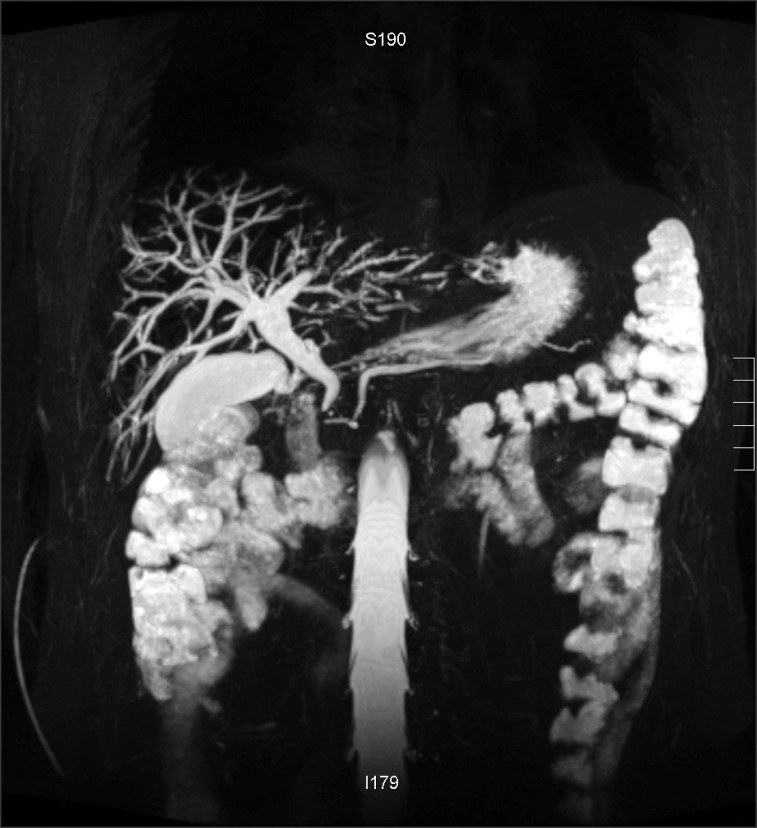
A 57-year-old man visited his local clinic, complaining of intermittent abdominal discomfort. Ultrasonography revealed pneumobilia and the patient was referred to our hospital for further evaluation. He had no relevant previous medical history and physical examination revealed no specific features. Laboratory results were within the normal ranges, including tumor markers such as carcinoembryonic antigen (CEA: 1.68 ng/ml) and carbohydrate antigen 19-9 (CA19-9: 4.73 U/ml). Endoscopic retrograde cholangiopancreatography (ERCP) showed individual EOPBD into the duodenal bulb with no papillary structure (Fig. 1). Magnetic resonance cholangiopancreatography (MRCP) showed a dilated bile duct, independent insertions of the pancreatic and bile ducts into the duodenal bulb, and a hook-shaped configuration of the distal common bile duct (CBD) (Fig. 2). There was no connection between the bile and pancreatic ducts before their individual openings. MRCP also identified a focal nodular lesion in the fundus of the gallbladder (GB).
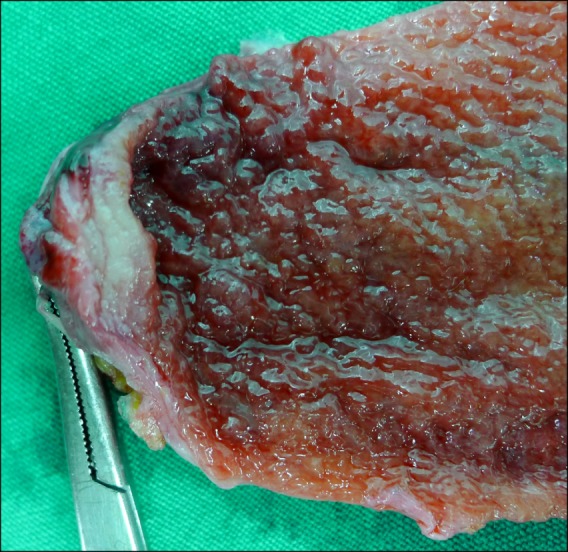
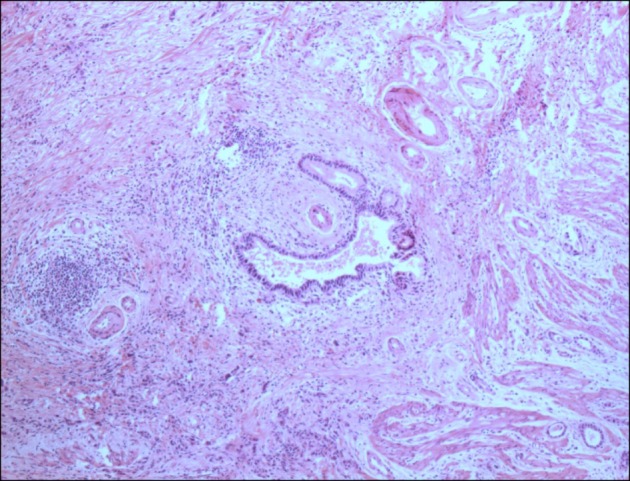
The patient discharged himself without further evaluation or treatment despite the clinician-recommended endoscopic balloon dilatation and laparoscopic cholecystectomy. As follow-up, the patient visited the outpatient department and underwent US evaluation every 3 months. Abdominal computed tomography (CT) scan 9 months after discharge showed a slight increase in the size of the GB lesion. Because the lesion was suspected as GB cancer, a laparoscopic cholecystectomy was performed. An intraoperative frozen biopsy revealed adenocarcinoma in the nodular lesion and in the cystic duct margin. After open conversion, radical cholecystectomy including regional lymphadenectomy and liver resection for S4b and S5 was performed. Because the tumor had invaded the cystic duct near the CBD junction, we resected the CBD and performed Roux-en-Y hepaticojejunostomy. On postoperative day 4, the patient started a soft blended diet after the passing of flatus. The abdominal drain was removed after checking the abdominal CT on postoperative day 9. The patient was discharged on postoperative day 15. The pathology results indicated a 1.2 cm tumor in the GB fundus (Fig. 3). Microscopically, there was invasion of moderately differentiated adenocarcinoma in the perimuscular connective tissue with no metastatic nodes observed in the 17 retrieved lymph nodes (Fig. 4). There was no tumor involvement in the CBD. There has been no recurrence of the tumor and the patient has been followed up regularly at the outpatient department since discharge.
Go to : 
The normal pancreatic and bile ducts enter the posteromedial aspect of the second portion of the duodenum. These ducts unite and form a common channel. A smooth muscular structure surrounds this channel and regulates the outflow of pancreatic and bile juice. However, some people have anomalous openings of the bile and pancreatic ducts to the intestine. The exact frequency of EOPBD is unclear, although it was recently reported in 0.10%-0.43% of patients who underwent ERCP.78 Although the etiology of this anomaly is not well known, the early subdivision of the pars hepatica during embryogenesis is a broadly accepted hypothesis. In the embryo, the pars hepatica forms the intrahepatic and common hepatic ducts; however, if the pars hepatica subdivides very early, it adopts a horizontal position above the growth zone between the stomach and duodenum, resulting in an abnormal opening of the bile duct into the stomach or duodenum.9
Patients with EOPBD present with various symptoms. In a study on 53 patients with EOPBD into the duodenal bulb, 95% and 59% visited the clinic with biliary pain, fever, respectively. In laboratory findings, 98% of patients showed elevated alkaline phosphatase and gamma-glutamyl transpeptidase levels, and 59% of patients presented with leukocytosis.7
Various imaging studies are useful in the investigation of EOPBD. Endoscopy shows the individual openings to the duodenal bulb6 and the absence of papillary structures around the openings in most cases. Abdominal CT and MRCP show characteristic features of EOPBD. In a study of 53 patients with EOPBD, the CBD was dilated to >1 cm in 94% of patients, and tapered and hook-shaped distally in 100% of patients. In some of these patients, the imaging findings included pneumobilia (21%), visualization of the pancreatic duct (22.6%), and dilated pancreatic duct (33%).7
In the present patient, abdominal ultrasonography at the local clinic revealed pneumobilia. At our hospital, endoscopy revealed separate openings into the duodenal bulb and MRCP showed parallel bile and pancreatic ducts that passed to the duodenal bulb without joining. The bile duct tapered and was hook shaped before opening into the intestine. This anomaly is related to benign biliary disease. It was reported that patients with EOPBD experience gastric and duodenal ulcers, recurrent cholangititis, CBD stones, and liver abscesses.7 However, EOPBD has not been associated with malignancy in any previous studies, except for Yamashita et al. who reported stomach cancer in a patient with pancreaticobiliary maljunction (PBM) and a double CBD opening to the stomach. They proposed that excessive exposure of the gastric mucosa to bile may lead to atrophic gastritis, which is a predisposing condition for gastric adenocarcinoma.10 In the present case, GB cancer was detected in a regular follow-up for EOPBD. The patient discharged himself without further treatment after his first admission, and a subsequent CT revealed aggravated GB wall thickening indicative of GB cancer. Radical cholecystectomy was subsequently performed. The presumptive pathogenesis of GB cancer in EOPBD is chronic inflammation, which is similar to that in PBM.
Numerous studies have revealed an association between PBM and biliary malignancy.111213 PBM was divided into C-P and P-C types, according to the type of union. A meta-analysis found that biliary malignancy was more common in patients with P-C type PBM without dilated CBD, as compared with those with other types of PBM;12 furthermore, it has been hypothesised that persistent stasis of bile and pancreatic juice may cause hyperplasia, metaplasia, and dysplasia of the ductal epithelium.121415 Tanno et al.16 found that stasis of pancreatic juice occurs exclusively in the GB in PBM without a dilated CBD, and Funabiki et al.15 reported that the incidence of GB cancer was higher in PBM without a dilated CBD, as compared with PBM with a dilated CBD (36.1% vs. 8.8%).
In the present case, there was no union between the pancreatic and bile ducts before they opened into the duodenal bulb, and no communicating duct was visualized between the ducts on ERCP or MRCP. The mechanism of carcinogenesis in this case is different from that for PBM. However, the presumptive hypothesis of GB cancer with EOPBD may be chronic inflammation of the bile duct. Reflux of intestinal contents and bacteria into the bile duct may cause recurrent cholangitis in patients with EOPBD because they lack a sphincteric barrier between the bile duct and the intestine, and chronic inflammation can be a predisposing factor for gallbladder cancer.717 Furthermore, the bile acid fraction contains carcinogenic substances such as lysolecitine and taurodeoxycholic acid.1819 Further studies are needed to reveal the pathogenesis of malignant disease in EOPBD.
As previously reported, there are surgical and endoscopic treatment modalities for EOPBD. The main treatment is generally surgery such as bile duct exploration, or choledochoenterostomy with cholecystectomy.8 Recent studies revealed that endoscopic management, such as CBD stone removal, balloon dilatation, stenting, and nasobiliary drainage showed comparable results with surgery.7 However, 13%-20% of patients who received these endoscopic procedures experienced recurrent cholangitis. Therefore, customized treatment is needed for each patient, and the long-term efficacies of endoscopic and surgical treatments should be compared.
In the current report, we described a patient who experienced malignant disease related to EOPBD suggestive that malignancy can occur in patients with EOPBD. Even though EOPBD into the duodenal bulb is extremely rare, clinicians should carefully follow up patients who have this anomaly, and consider surgical treatment in patients with a suspected malignant lesion.
Go to : 
References
1. Sezgın O, Altintaş E, Uçbılek E. Ectopic opening of the common bile duct into the stomach. Turk J Gastroenterol. 2010; 21:163–167. PMID: 20872331.

2. Kanematsu M, Imaeda T, Seki M, Goto H, Doi H, Shimokawa K. Accessory bile duct draining into the stomach: case report and review. Gastrointest Radiol. 1992; 17:27–30. PMID: 1544554.

3. Bernard P, Le Borgne J, Dupas B, Kohnen-Shari N, Raoult S, Hamel A. Double common bile duct with ectopic drainage into the stomach. Case report and review of the literature. Surg Radiol Anat. 2001; 23:269–272. PMID: 11694973.

4. Li L, Yamataka A, Wang YX, Wang DY, Wang K, Li ZX, et al. Anomalous pancreatic duct anatomy, ectopic distal location of the papilla of Vater and congenital biliary dilatation: a new developmental triad? Pediatr Surg Int. 2003; 19:180–185. PMID: 12698266.

5. Paraskevas G, Papaziogas B, Natsis K, Katsinelos P, Gigis P, Atmatzidis K. Abnormal location of papilla of Vater: a cadaveric study. Folia Morphol (Warsz). 2005; 64:51–53. PMID: 15832271.
6. Lee HJ, Ha HK, Kim MH, Jeong YK, Kim PN, Lee MG, et al. ERCP and CT findings of ectopic drainage of the common bile duct into the duodenal bulb. AJR Am J Roentgenol. 1997; 169:517–520. PMID: 9242767.

7. Disibeyaz S, Parlak E, Cicek B, Cengiz C, Kuran SO, Oguz D, et al. Anomalous opening of the common bile duct into the duodenal bulb: endoscopic treatment. BMC Gastroenterol. 2007; 7:26. PMID: 17610747.

8. Lee SS, Kim MH, Lee SK, Kim KP, Kim HJ, Bae JS, et al. Ectopic opening of the common bile duct in the duodenal bulb: clinical implications. Gastrointest Endosc. 2003; 57:679–682. PMID: 12709696.

9. Sung HY, Kim JI, Park YB, Cheung DY, Cho SH, Park SH, et al. The papilla of Vater just below the pylorus presenting as recurrent duodenal ulcer bleeding. Intern Med. 2007; 46:1853–1856. PMID: 18025767.

10. Yamashita K, Oka Y, Urakami A, Iwamoto S, Tsunoda T, Eto T. Double common bile duct: a case report and a review of the Japanese literature. Surgery. 2002; 131:676–681. PMID: 12075184.

11. Mori K, Nagakawa T, Ohta T, Nakano T, Kayahara M, Kanno M, et al. Association between gallbladder cancer and anomalous union of the pancreaticobiliary ductal system. Hepatogastroenterology. 1993; 40:56–60. PMID: 8462931.
12. Li Y, Wei J, Zhao Z, You T, Zhong M. Pancreaticobiliary maljunction is associated with common bile duct carcinoma: a meta-analysis. ScientificWorldJournal. 2013; 2013:618670. PMID: 24489507.

13. Kamisawa T, Kuruma S, Tabata T, Chiba K, Iwasaki S, Koizumi S, et al. Pancreaticobiliary maljunction and biliary cancer. J Gastroenterol. 2015; 50:273–279. PMID: 25404143.

14. Komi N, Tamura T, Miyoshi Y, Kunitomo K, Udaka H, Takehara H. Nationwide survey of cases of choledochal cyst. Analysis of coexistent anomalies, complications and surgical treatment in 645 cases. Surg Gastroenterol. 1984; 3:69–73. PMID: 6085899.
15. Funabiki T, Matsubara T, Miyakawa S, Ishihara S. Pancreaticobiliary maljunction and carcinogenesis to biliary and pancreatic malignancy. Langenbecks Arch Surg. 2009; 394:159–169. PMID: 18500533.

16. Tanno S, Obara T, Maguchi H, Fujii T, Mizukami Y, Shudo R, et al. Association between anomalous pancreaticobiliary ductal union and adenomyomatosis of the gall-bladder. J Gastroenterol Hepatol. 1998; 13:175–180. PMID: 10221820.

17. Gregg JA, De Girolami P, Carr-Locke DL. Effects of sphincteroplasty and endoscopic sphincterotomy on the bacteriologic characteristics of the common bile duct. Am J Surg. 1985; 149:668–671. PMID: 3993851.

18. Reveille RM, Van Stiegmann G, Everson GT. Increased secondary bile acids in a choledochal cyst. Possible role in biliary metaplasia and carcinoma. Gastroenterology. 1990; 99:525–527. PMID: 2163938.
19. Mizuno M, Kato T, Koyama K. An analysis of mutagens in the contents of the biliary tract in pancreaticobiliary maljunction. Surg Today. 1996; 26:597–602. PMID: 8855491.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download