Abstract
Backgrounds/Aims
We report our experience with day-surgery laparoscopic cholecystectomy and assess its feasibility and safety.
Methods
Data was collected on all the patients who underwent day-surgery laparoscopic cholecystectomy between February 2009 and February 2014 at Prince Sultan Military Medical City, Riyadh, Kingdom of Saudi Arabia. All patients had symptomatic cholelithiasis that was proven on imaging studies with clearance of the common bile duct. The patient biographical data (age, gender, American Society of Anaesthesiology status, medical comorbidities) and surgical outcomes were then obtained. There was an evaluation of the success rate of day-surgery laparoscopic cholecystectomy, reasons for unexpected admission, and the re-admission rate.
Results
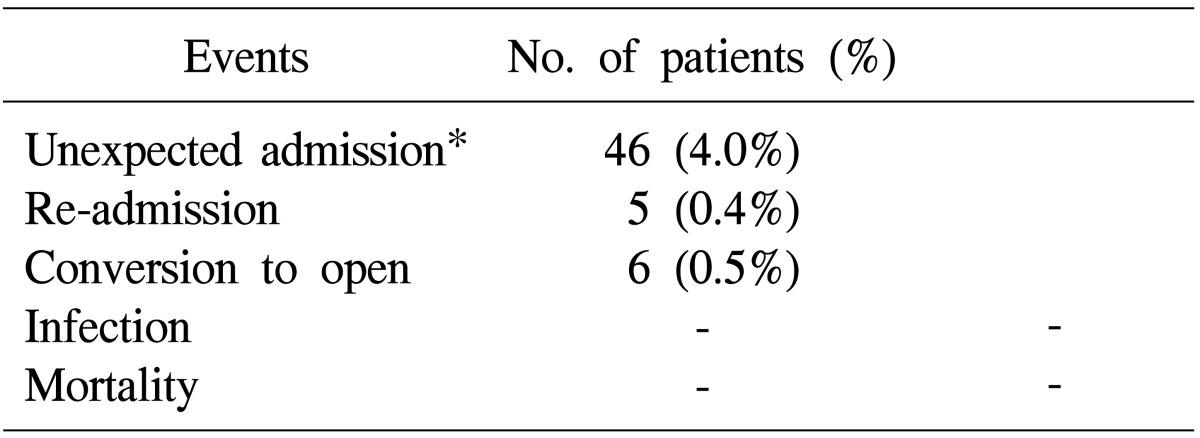
A total of 1,140 patients were included in this study. The success rate for day-surgery laparoscopic cholecystectomy was 96%. The reasons for unexpected hospital admission for 46 patients (4%) included persistent abdominal pain and postoperative emesis. The postoperative re-admission rate was 0.4% (5 patients). There were no major complications, and the conversion rate was 0.5% (6 patients).
Go to : 
Laparoscopic cholecystectomy (LC) was first performed in 1985 by Mühe in Germany and is now the treatment of choice for symptomatic gallstone diseases.1 As with other laparoscopic procedures, LC is associated with less postoperative pain, smaller scars, shorter hospitalization duration, and an earlier return to routine activities as compared with open surgical techniques.2 As expertise in laparoscopic surgery improves, there is now a trend towards performing LC as a day-surgery procedure because of its potential economic benefits. In many places, this has been both safe and acceptable.345 However, there is a lack of information on day-surgery LC carried out locally, and therefore the aim of this retrospective study is to report on our local experience with day-surgery LC, and to assess its feasibility and safety.
Go to : 
Following promising initial experience, we retrospectively studied the outcomes of 1,140 consecutive patients treated with day-surgery LC for over 5 years, from February 2009 to February 2014, at Prince Sultan Military Medical City, Riyadh, Kingdom of Saudi Arabia. All patients had symptomatic cholelithiasis that was proven on imaging studies with a normal liver function test. Patients with possible common bile obstruction had confirmation of clearance of their common bile duct either through endoscopic retrograde cholangiopancreatography (ERCP), or endoscopic ultrasonography. The patients were briefed on the administration of the procedure as a day surgery following a standard care pathway protocol: they were to report to the Day Surgery Unit in the morning of their surgery after fasting (NPO) from midnight the night before.
The LC was carried out via a standard 4-port technique for the laparoscopic telescope, and for retrieval of the gallbladder using a plastic bag. The 4 ports were infiltrated with local anesthetic before incision and placement of the ports to minimize postoperative wound pain.
After the surgery, all patients were monitored first in the recovery ward and subsequently in the Day Surgery Observation Ward. Hourly parameters were recorded, including pulse rate, blood pressure monitoring, conscious level, and the pain score. A senior staff member reviewed all patients at the end of the day, between 6 PM and 7 PM, before they were discharged. Criteria for discharge included stable parameters, ability to retain feeds, ability to ambulate with minimal assistance and discomfort, and being accompanied home by a capable caregiver.
The possibility of re-admission after surgery was explained to all patients. This could happen if any unusual events occur, such as conversion to open surgery or unsatisfactory recovery from anesthesia. All patients were briefed on the unusual signs to look out for, and were given postoperative instructions. The symptoms on the postoperative instructions include increasing abdominal pain, excessive blood oozing from port sites through the dressings, and worsening giddiness, nausea, or vomiting. The patients were also given an emergency telephone number to call if they had any queries after their surgery and prescribed a 5-day course of paracetamol to be taken strictly. They were then reviewed in the outpatient clinic within 2 weeks of their surgery. Patient biographic data (age, gender, American Society of Anesthesiology [ASA] status, medical comorbidities) and outcomes were collected. There was an evaluation of the success rate of day-surgery LC, reasons for overnight admission, and the re-admission rate.
The patient selection criteria were as follows: age of 1370 years; body mass index <40; living in Riyadh (one hour from Prince Sultan Military Medical City); American Society of Anesthesiology (ASA) physical status (PS) I or II; living with responsible persons; accompanied to the unit with someone responsible to take him/her home postoperatively.
Go to : 
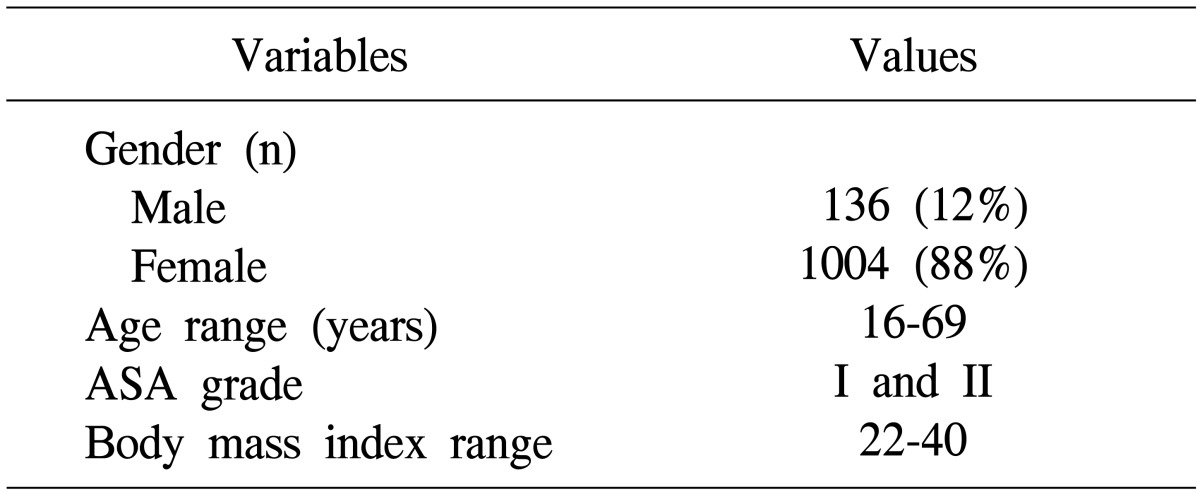
Over the 5 years, 14,646 operations were carried out in different specialties, with general surgery accounting for 25% (3,612). A total of 1,223 patients were booked for day-surgery LC between February 2009 and February 2014. Of these, 1,140 patients were operated, and 83 patients (5%) were cancelled for different reasons. There were 136 men and 1,004 women, with a mean age of 34, and a range of 16-69 years.
All of them were classified as ASA PS I and II (Table 1). The mean surgery time was 40 minutes, range 32-110 minutes. The average total operating time was 65 minutes. An average of 25 minutes (38%) of the operating time was utilized for preparation. All the patients were discharged by 7 PM (recovery time between 5-6 hours).
Only 46 patients (4% unexpected admission) failed to be discharged on the same day (Table 2). All patients were discharged the next day in good condition. Five patients (0.4%) who underwent day-surgery LC successfully had to be readmitted. The patients presented with abdominal pain, abdominal wall hematoma, and vomiting, which were treated conservatively. None of the patients had major complications, and all were discharged within 48 hours.
Go to : 
Most authors agree that day-surgery LC offers many advantages compared with inpatient LC. It allows the patient to recuperate at home, and reduces hospitalization costs. At the Prince Sultan Military Medical City, the costs for inpatient management can add up to a substantial amount. This ranges from Saudi Arabian Riyal 3,500-4,000 for an overnight admission, depending on the class of admission and the amount of consumables used during the stay. The day-surgery LC is also beneficial for the Hospital as this means that more inpatient beds are available for emergency cases. In addition, day-surgery LC frees up operating spaces in major operating rooms, which can then be better utilized.
In many institutions, an intermediate form of postoperative care is adopted, where patients are not admitted, but are lodged in an overnight recovery ward for less than 24 hours. This has been termed "ambulatory LC," and has been shown to be safe and feasible. However, this still requires an additional establishment to accommodate these patients overnight, when they could be better taken care of by their immediate relatives in the comfort of their homes. The proximity and easy accessibility of patients to major hospitals mean that in the rare event that urgent medical care is required, the care will not be delayed. In some countries, one of the selection criteria for ambulatory LC is the distance of the patient's residence from the hospital.56
The success rate (96%) and re-admission rate (0.4%) in this study is comparable with other studies performing day-surgery LC or ambulatory LS,378 with success rates of 86%-95%, and re-admission rates of 1.5%-8%. This suggests that an overnight stay does not add value to the level of medical care and monitoring. As for the 5 cases requiring re-admission, even inpatient management would not have prevented this as the complications appeared much later. It is important to maintain a high success rate for patients planned for day-surgery LC, the failure of which means additional costs to the institution. In addition, there will be more inconvenience encountered by the caregiver and the rest of the family members. Many authors have suggested that careful patient selection helps to increase the success rate of day-surgery LC.79 Some of these factors include the age of the patient, ASA physical status, and the presence of other comorbidities.
During the same study period, we carried out 2,116 elective LCs at the same institute. They were all admitted to the general ward for an average of 4.2 days, with a conversion rate of 3.6%. Our day-surgery LC accounted for 54% of total cholecystectomies at Prince Sultan Military Medical City.
In conclusion, we think that day-surgery LC is a safe and feasible procedure, which is likely to show increasing popularity among both patients and surgeons in view of its practical benefits. However, careful patient selection and adequate preoperative education of the patients following a clinical pathway are necessary to ensure a high success rate. Our suggested inclusion criteria for day-surgery LC include an age of less than 70 years and ASA physical status of I or II. As a follow-up to this preliminary study, we suggest that a prospective study be conducted to look into factors that can increase the likelihood of same-day discharge for patients scheduled for day-surgery LC. This may include methods to reduce postoperative pain and emesis, such as selecting the most appropriate anesthetics, analgesics, and preoperative anti-emetics.
Go to : 
References
1. Reynolds W Jr. The first laparoscopic cholecystectomy. JSLS. 2001; 5:89–94. PMID: 11304004.
2. Hendolin HI, Pääkönen ME, Alhava EM, Tarvainen R, Kemppinen T, Lahtinen P. Laparoscopic or open cholecystectomy: a prospective randomised trial to compare postoperative pain, pulmonary function, and stress response. Eur J Surg. 2000; 166:394–399. PMID: 10881952.
3. Chok KS, Yuen WK, Lau H, Lee F, Fan ST. Outpatient laparoscopic cholecystectomy in Hong Kong Chinese -- an outcome analysis. Asian J Surg. 2004; 27:313–316. PMID: 15564186.

4. Leeder PC, Matthews T, Krzeminska K, Dehn TC. Routine day-case laparoscopic cholecystectomy. Br J Surg. 2004; 91:312–316. PMID: 14991631.

5. Chauhan A, Mehrotra M, Bhatia PK, Baj B, Gupta AK. Day care laparoscopic cholecystectomy: a feasibility study in a public health service hospital in a developing country. World J Surg. 2006; 30:1690–1695. PMID: 16902738.

6. Kaman L, Verma GR, Sanyal S, Bhukal I. Relevance of day care laparoscopic cholecystectomy in a developing nation. Trop Gastroenterol. 2005; 26:95–97. PMID: 16225056.
7. Ammori BJ, Davides D, Vezakis A, Martin IG, Larvin M, Smith S, et al. Day-case laparoscopic cholecystectomy: a prospective evaluation of a 6-year experience. J Hepatobiliary Pancreat Surg. 2003; 10:303–308. PMID: 14598151.

8. Jain PK, Hayden JD, Sedman PC, Royston CM, O'Boyle CJ. A prospective study of ambulatory laparoscopic cholecystectomy: training economic, and patient benefits. Surg Endosc. 2005; 19:1082–1085. PMID: 16021378.

9. Vuilleumier H, Halkic N. Laparoscopic cholecystectomy as a day surgery procedure: implementation and audit of 136 consecutive cases in a university hospital. World J Surg. 2004; 28:737–740. PMID: 15457349.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download