Abstract
Emergent abdominal surgery in cirrhotic patients with ascites can result in dismal postoperative outcomes such as sepsis and hepatic failure. In the present case, small bowel resection followed by anastomosis by the hand-sewn method was performed for small bowel strangulation caused by an umbilical hernia; deceased donor liver transplantation was performed one week after the bowel resection because of deterioration of hepatic function. To the best of our knowledge, this is the first case of liver transplantation performed at only one week after small bowel resection; and although we obtained a good result, the optimal time to perform liver transplantation in this situation requires further evaluation.
Go to : 
Umbilical hernias occur in up to 20% of cirrhotic patients with ascites, and it remains controversial whether an elective herniorrhaphy should be performed.1 A "watchful waiting" strategy has been widely adopted to avoid operative complications; however, conservative management of an umbilical hernia exposes cirrhotic patients to an emergent operation due to complications such as rupture, incarceration, and strangulation of the bowel. If bowel strangulation occurs, an operation on the gastrointestinal tract is a major surgical challenge in these patients; and it often results in deterioration of hepatic function, postoperative bleeding, acute tubular necrosis, sepsis, and ultimately death.2 Especially, when a patient develops postoperative deterioration of hepatic function, surgeons face the dilemma of proceeding with liver transplantation because of the risk of uncontrolled infection in a cirrhotic patient with ascites.
We present a case of deceased donor liver transplantation (DDLT), which was performed one week after small bowel resection for an umbilical hernia, with a successful result.
Go to : 
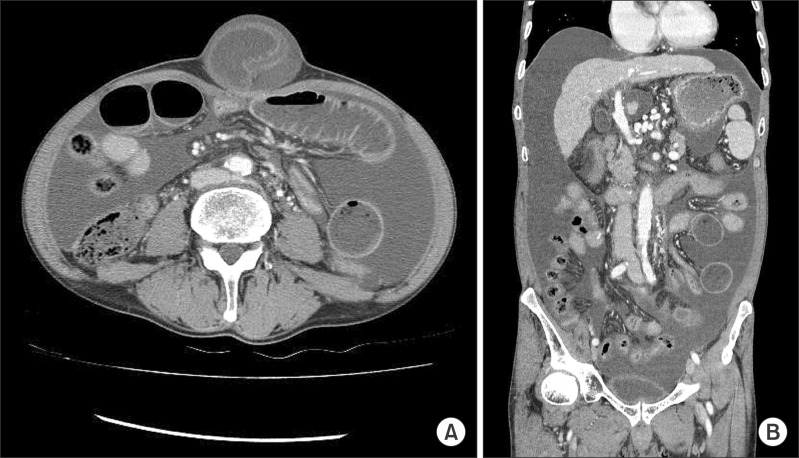
In October 2009, a 64-year-old male who have been listed on the KONOS (Korean Network for Organ Sharing) was referred to our hospital for acute-onset abdominal pain. He was diagnosed with hepatocellular carcinoma (HCC) in 2007, and transarterial chemoembolization (TACE) was performed four times for the management of HCC. After receiving the fourth TACE, ascites could not be controlled with conservative therapy; and shortly thereafter, he developed an umbilical hernia and suffered from two episodes of spontaneous bacterial peritonitis. On physical examination, there was marked tenderness in the umbilical area and a protruding mass; and he had a Model for End-Stage Liver Disease (MELD) score of 15. His serum bilirubin level was 2.6 mg/dl, INR was 1.63, and serum creatinine level was 0.9 mg/dl. Contrast-enhanced computed tomography scan of the abdomen showed a large amount of ascites and incarcerated small bowel in an umbilical hernia (Fig. 1). On laparotomy, the incarcerated bowel was dull gray or black in color and lacked motility; therefore, we resected the strangulated bowel and performed an end-to-end anastomosis by the hand-sewn method. Primary closure of the hernia defect was performed without placement of abdominal drainage tubes.
Bowel motility recovered on the fourth postoperative day, and he did not show any evidence of infection. However, the abdomen was distended and the liver function profile deteriorated. The serum bilirubin level steadily increased up to 6.3 mg/dl, and the INR increased up to 2.15. On the seventh postoperative day, the Child-Turcotte-Pugh (CTP) class deteriorated from Class B to Class C and his MELD score was 22 at postoperative day (POD) 7.
Fortunately, at one week postoperatively, a whole liver transplant from a brain-dead donor was allocated to the patient and we performed DDLT. Following transplantation, the patient had favorable graft function and is living in a satisfactory condition four years later (Fig. 2).
Go to : 
A "watchful waiting" strategy for umbilical hernias in cirrhotic patients, which obviates the operative risk, has been traditionally advocated and is still considered to be a component of an appropriate approach. However, the major drawback of the "watchful waiting" approach is the development of a complicated umbilical hernia; Telem et al. reported a mortality rate of 5% and a morbidity rate of 71% as the perioperative outcomes of patients with advanced liver cirrhosis who developed a complicated umbilical hernia.3 Especially, in cases where emergent gastrointestinal surgery becomes necessary, the results are dismal. Mansour et al. reported a mortality rate of 50% in the emergent operation group and a mortality rate of 39% after gastrointestinal surgery in patients with cirrhosis as a result of coagulopathy and sepsis.2 In addition, they reported a mortality rate of up to 66.6% after surgery for small bowel disease.
Recently, several studies have reported about elective umbilical hernia repair in the presence of cirrhosis and ascites with much improved surgical outcomes. Marsman et al. reported a complication rate of 18% after elective correction of umbilical hernias in patients with liver cirrhosis; they emphasized that elective hernia repair should be advocated because of the poor surgical outcome, with one-third mortality after emergency hernia repair.4 Furthermore, Park et al. reported that CTP C class was not a contraindication for elective hernia repair in patients with liver cirrhosis.5
In the present case, small bowel strangulation was detected at the time of surgery and small bowel resection was mandatory. As mentioned previously, we used the hand-sewn method for bowel anastomosis and drains were not placed. This approach was used to minimize anastomotic leak, intra-abdominal abscess formation, and secondary peritonitis (most postoperative deaths are due to sepsis and deterioration of hepatic function). There is no specific strategy for the bowel anastomosis technique in this situation; however, Brundage et al. reported superior outcomes with sutured anastomoses compared to stapled bowel repair in trauma patients.6
Chaudhary et al. reported about the simultaneous performance of bowel resection and liver transplantation for strangulated umbilical hernia in a patient with CTP Class C and emphasized the difficulty in determining the appropriate surgical timing.7 In our case, we performed liver transplantation one week after bowel resection and the patient did not show any evidence of anastomotic leak or peritonitis before the transplantation. We are of the opinion that simultaneous bowel resection and liver transplantation may carry a significant risk for developing an anastomotic leak, abscess, and uncontrolled sepsis under the conditions of receiving immunosuppressant treatment.
In conclusion, when deterioration of hepatic function, which requires liver transplantation, occurs after bowel surgery, sepsis should be ruled out. In addition, the method of anastomosis to achieve bowel continuity and the indication for liver transplantation in this situation needs further evaluation.
Go to : 
References
1. Belghiti J, Durand F. Abdominal wall hernias in the setting of cirrhosis. Semin Liver Dis. 1997; 17:219–226. PMID: 9308126.

2. Mansour A, Watson W, Shayani V, Pickleman J. Abdominal operations in patients with cirrhosis: still a major surgical challenge. Surgery. 1997; 122:730–735. PMID: 9347849.

3. Telem DA, Schiano T, Divino CM. Complicated hernia presentation in patients with advanced cirrhosis and refractory ascites: management and outcome. Surgery. 2010; 148:538–543. PMID: 20346479.

4. Marsman HA, Heisterkamp J, Halm JA, Tilanus HW, Metselaar HJ, Kazemier G. Management in patients with liver cirrhosis and an umbilical hernia. Surgery. 2007; 142:372–375. PMID: 17723889.

5. Park JK, Lee SH, Yoon WJ, Lee JK, Park SC, Park BJ, et al. Evaluation of hernia repair operation in Child-Turcotte-Pugh class C cirrhosis and refractory ascites. J Gastroenterol Hepatol. 2007; 22:377–382. PMID: 17295770.

6. Brundage SI, Jurkovich GJ, Hoyt DB, Patel NY, Ross SE, Marburger R, et al. WTA Multi-institutional Study Group. Western Trauma Association. Stapled versus sutured gastrointestinal anastomoses in the trauma patient: a multicenter trial. J Trauma. 2001; 51:1054–1061. PMID: 11740250.

7. Chaudhary A, Daga S, Goyal N, Ramaswamy VK, Agarwal S, Pareek S, et al. Emergency liver transplant in patient with Child-Pugh class C cirrhosis and strangulated umbilical hernia. Exp Clin Transplant. 2013; 11:66–67. PMID: 23190414.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download