Abstract
Backgrounds/Aims
Few reports have validated the clinical postoperative pancreatic fistula (PF) after distal pancreatectomy. The study intended to validate the predictability for clinical PF of drain amylase and lipase and to find out more appropriate postoperative day (POD) for diagnostic criterion of PF.
Methods
A total of 154 patients underwent distal pancreatectomy. We used the clinical database registry system of the Gangnam Severance Hospital and Severance Hospital, Yonsei University Health System for these analyses. The receiver operating characteristic curve of the drain amylase or lipase concentration on each day was used to predict clinical PF (International Study Group on Pancreatic Fistula [ISGPF] grade B or C) and areas under the curves (AUC) were compared.
Results
Amylase and lipase AUC values poorly predicted clinical PF before POD 3 and, gradually increased until POD 5 and became well correlated with clinical PF (ISGPF grade B or C). In contrast, the prediction of clinical PF using drain lipase did not differ from that using drain amylase. The drain amylase concentration on POD 6 was most precisely correlated with clinical PF.
Conclusions
Clinical PF prediction was validated by using drain amylase and lipase concentrations, in which drain amylase assessment at POD 6 appeared to be an appropriate diagnostic criterion of PF after distal pancreatectomy. We suggest some modification of ISGPF definition, especially for distal pancreatectomy.
Go to : 
Distal pancreatectomy is performed for various benign and malignant pancreatic disease.1 Whether in pancreaticoduodenectomy or distal pancreatectomy, postoperative pancreatic fistula is still regarded as a major complication.2 Pancreatic fistula (PF) is asymptomatic in many patients, but it may precipitate clinically relevant complications including intra-abdominal abscess, hemorrhage and sepsis.3
According to the International Study Group of Pancreatic Fistula (ISGPF),4 PF is diagnosed when there is measurable drain output on or after postoperative (POD) 3 days, with an amylase content 3 times the upper limit of normal serum value. The ISGPF has proposed a classification scheme for PF based on clinical and laboratory parameters, but it has not been correlated with laboratory results and clinical course.5
Although clinical studies regarding PF after pancreaticoduodenectomy have been reported, the incidence and clinical course of PF after distal pancreatectomy have not been well investigated.5,6,7,8,9 Pancreatic lipase is also representative pancreas enzymes, but the ISGPF used only amylase concentration in the drain by expert opinions without explanation.
Therefore, the first aim of this study was to compare the predictability for clinical PF between drain amylase and lipase. The second aim was to evaluate the appropriate postoperative day (POD) for use as the diagnostic criterion of PF with clinical relevance.
Go to : 
Between March 2010 and March 2014, a total of 154 patients underwent distal pancreatectomy at Yonsei Universty Health System, Gangnam Severance Hospital and Severance Hospital. All cancer patients were staged according to the 7th edition of American Joint Committee on Cancer staging system (AJCC).
The surgical procedures and perioperative management were performed as previously reported.10 Drains were used routinely in all patients and were placed in the resected stump of the pancreas. The drain fluid was daily collected and quantitatively analyzed for amylase and lipase content. The criteria for drain removal was the output was <100 ml/day for consecutive days or lack of PF, as well as absence of abnormal fluid collection, abscess or infection.
The receiver operating characteristics (ROC) curve of drain amylase or lipase concentration on each day was used to predict clinical PF (ISGPF grade B or C). To evaluate the appropriate POD to use as the diagnostic criterion of PF with clinical relevance, the AUC of ROC curve of drain amylase concentration on each day were compared. We considered the day for diagnostic criterion for PF POD with the most precise prediction of clinical PF (AUC closest to 1), and then modified the definition of ISGPF to reduce the clinically irrelevant PF (ISGPF grade A).
The ROC curve analysis of the drainage amylase concentration on each day and AUC value was used to predict the clinical PF (ISGPF grade B or C). R package, version 3.0.2 (http://www.R-project.org) was used to perform these analyses.
Go to : 
A total of 154 patients who underwent distal pancreatectomy were included in this study. The study group consisted of 67 men and 87 women whose mean age was 61.5±10.5 years. Of the 154 patients, 110 underwent open distal pancreatectomy, 38 underwent laparoscopic distal pancreatectomy, and 6 underwent robotic distal pancreatectomy. Their pathologic diagnoses were pancreatic carcinoma in 44, solid pseudopapillary tumor of pancreas in 26, neuroendocrine tumors in 23, mucinous cystic neoplasm in 17, pseudocyst in 16, intraductal papillary mucinous neoplasm in 12, metastatic cancer in 10, and pancreatic injury in 6 patients.
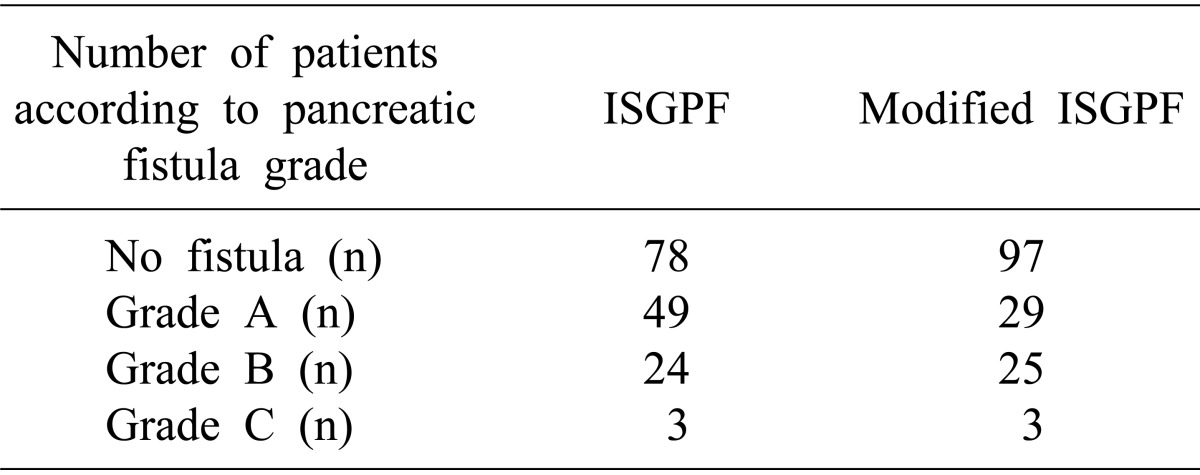
Of these 154 patients, PF developed in 76 (49.3%) patients. Grade A pancreatic fistula occurred in 49 (31.8%) patients, grade B in 24 (15.6%) patients, and grade C in 3 (1.9%) patients.
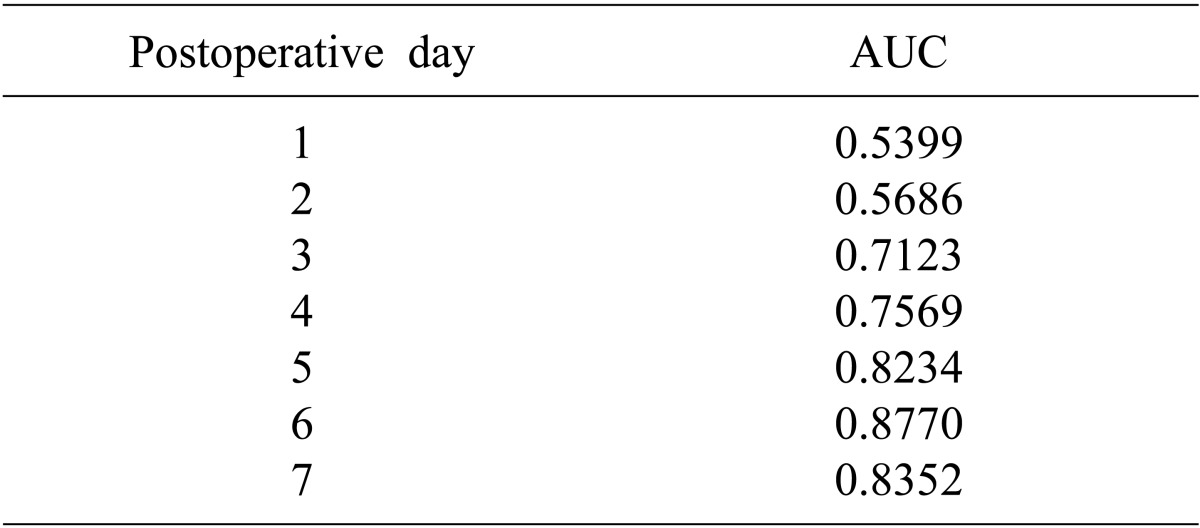
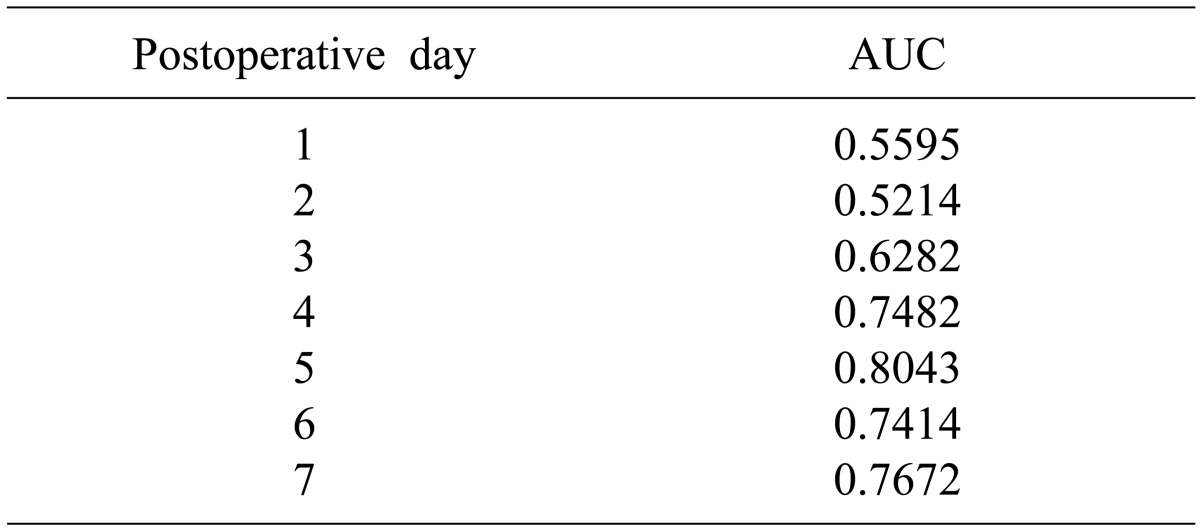
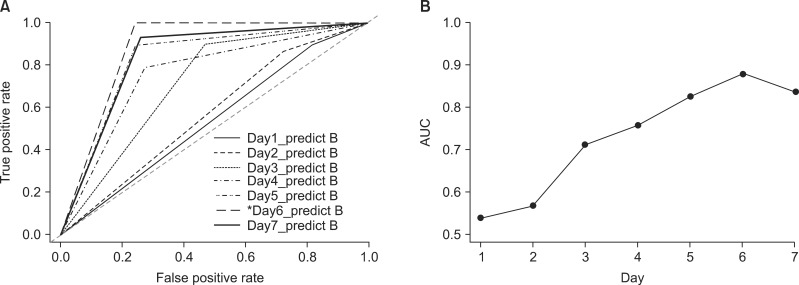
The AUC values of drain concentration for amylase poorly predicted clinical PF before POD 3, but became well correlated with clinical PF (ISGPF grade B or C) after POD 5 (Table 1). The AUC values of lipase poorly predicted clinical PF before POD 3, but was also well correlated with clinical PF after POD 5 (Table 2). In contrast, the prediction of clinical PF using drain lipase did not different from that using drain amylase.
AUC of ROC analysis showed that drain pancreatic enzyme measurement POD 6 was the most appropriate diagnostic criterion for postoperative PF (Fig 1).
We used the value on POD 6 to predict clinical PF and then modified the definition of ISGPF, and then defined the criterion as an amylase concentration greater than three times that of normal upper limit. After this modification of ISGPF, the number of patients with the clinically irrelevant PF (grade A) were reduced from 49 to 29, but the incidence of clinical PF was not changed (Table 3).
Go to : 
The ISGPF defines PF by amylase concentration but does not explain why it alone was chosen. Lipase is more accurate parameter than amylase for the diagnosis of acute pancreatitis.11,12 Due to this point, the use of lipase for the diagnosis of postoperative PF was investigated in this study. There was one study reporting that the lipase level in the drainage fluid is more sensitive parameter for prediction of clinical complications with pancreatic leakage than amylase concentration in gastrectomy.13 In this study, clinical PF was strongly correlated lipase concentrations in the drains. Therefore, measurement of lipase concentration would have some diagnostic significance for clinical PF.
The purpose of the present study was to determine if modified definition for PF can be used to predict which patients will develop a clinically significant PF. This question is important because current ISGPF may increase the rate of clinical irrelevance PF (grade A). In this study, the number of patients with clinically irrelevant or laboratory PF (grade A) according to modified ISGPF definition was reduced from 49 to 29 after modification of PF definition. In previous studies, amylase concentration was elevated during the early postoperative period and then gradually decreased to nearly normal levels by POD 4 in most patients.10 However, in the clinical postoperative PF group, the drain amylase concentration was continuously high or re-elevated due to failure of healing process and followed a bimodal distribution during the postoperative period. This may explain why the values on POD 6 were more closely correlated with PF than those on POD 3.
This study has limitations that performed retrospectively and was not verified to other clinical settings. Nonetheless, it showed that the predictability for clinical PF was assessed between drain amylase and lipase, and that POD 6 value was appropriate as a diagnostic criterion of PF with clinical relevance after distal pancreatectomy. Modification of the current ISGPF classification may be needed to improve the clinical correlation with the pancreatic enzyme drain concentrations during the postoperative period, especially in patients undergoing distal pancreatectomy.
Go to : 
References
1. Lillemoe KD, Kaushal S, Cameron JL, Sohn TA, Pitt HA, Yeo CJ. Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg. 1999; 229:693–698. PMID: 10235528.

2. Wang H, Xiu D, Jiang B, Ma C, Yuan C. Postoperative pancreatic fistula in distal pancreatectomy: experience from 1 institution. Pancreas. 2014; 43:588–591. PMID: 24713670.
3. Shrikhande SV, D'Souza MA. Pancreatic fistula after pancreatectomy: evolving definitions, preventive strategies and modern management. World J Gastroenterol. 2008; 14:5789–5796. PMID: 18855976.

4. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13. PMID: 16003309.

5. Goh BK. Clinical and economic validation of the international study group of pancreatic fistula classification scheme. Ann Surg. 2007; 246:909–910. PMID: 17968191.

6. Liang TB, Bai XL, Zheng SS. Pancreatic fistula after pancreaticoduodenectomy: diagnosed according to International Study Group Pancreatic Fistula (ISGPF) definition. Pancreatology. 2007; 7:325–331. PMID: 17627097.

7. Park CM, Park JS, Cho ES, Kim JK, Yu JS, Yoon DS. The effect of visceral fat mass on pancreatic fistula after pancreaticoduodenectomy. J Invest Surg. 2012; 25:169–173. PMID: 22583013.

8. Shin HW, Kim JK, Park JS, Yoon DS. Can we predict postoperative pancreatic leakage after pancreaticoduodenectomy using preoperative fecal elastase-1 level? J Clin Lab Anal. 2013; 27:379–383. PMID: 24038223.

9. Shyr YM, Su CH, Wu CW, Lui WY. Does drainage fluid amylase reflect pancreatic leakage after pancreaticoduodenectomy? World J Surg. 2003; 27:606–610. PMID: 12715232.

10. Kim JK, Park JS, Hwang HK, Shin HW, Yoon DS. Drainage volume after pancreaticoduodenectomy is a warning sign of chyle leakage that inversely correlates with a diagnosis of pancreatic fistula. World J Surg. 2013; 37:854–862. PMID: 23389668.

11. Yadav D, Agarwal N, Pitchumoni CS. A critical evaluation of laboratory tests in acute pancreatitis. Am J Gastroenterol. 2002; 97:1309–1318. PMID: 12094843.

12. Smith RC, Southwell-Keely J, Chesher D. Should serum pancreatic lipase replace serum amylase as a biomarker of acute pancreatitis? ANZ J Surg. 2005; 75:399–404. PMID: 15943725.

13. Seo KW, Yoon KY, Lee SH, Shin YM, Choi KH, Hwang HY. Amylase, lipase, and volume of drainage fluid in gastrectomy for the early detection of complications caused by pancreatic leakage. J Korean Surg Soc. 2011; 81:402–407. PMID: 22200041.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download