1. Sicklick JK, Camp MS, Lillemoe KD, Melton GB, Yeo CJ, Campbell KA, et al. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg. 2005; 241:786–792. PMID:
15849514.
2. McMahon AJ, Fullarton G, Baxter JN, O'Dwyer PJ. Bile duct injury and bile leakage in laparoscopic cholecystectomy. Br J Surg. 1995; 82:307–313. PMID:
7795992.

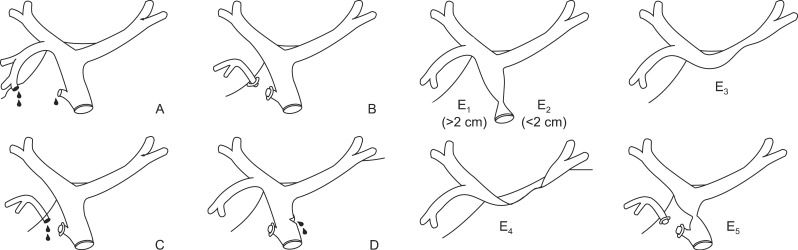
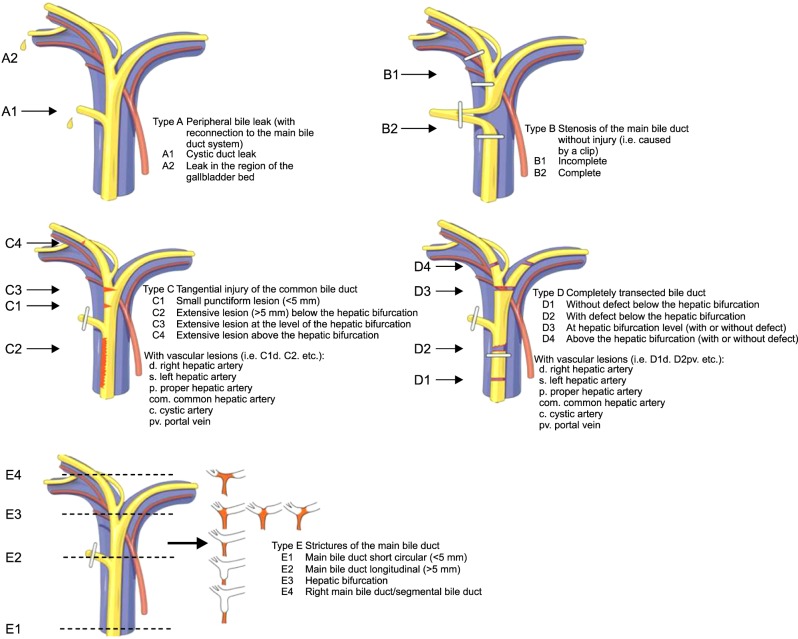
3. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995; 180:101–125. PMID:
8000648.
4. Shea JA, Healey MJ, Berlin JA, Clarke JR, Malet PF, Staroscik RN, et al. Mortality and complications associated with laparoscopic cholecystectomy. A meta-analysis. Ann Surg. 1996; 224:609–620. PMID:
8916876.
5. Targarona EM, Marco C, Balagué C, Rodriguez J, Cugat E, Hoyuela C, et al. How, when, and why bile duct injury occurs. A comparison between open and laparoscopic cholecystectomy. Surg Endosc. 1998; 12:322–326. PMID:
9543521.
6. Lillemoe KD, Melton GB, Cameron JL, Pitt HA, Campbell KA, Talamini MA, et al. Postoperative bile duct strictures: management and outcome in the 1990s. Ann Surg. 2000; 232:430–441. PMID:
10973393.

7. Gazzaniga GM, Filauro M, Mori L. Surgical treatment of iatrogenic lesions of the proximal common bile duct. World J Surg. 2001; 25:1254–1259. PMID:
11596885.

8. Savar A, Carmody I, Hiatt JR, Busuttil RW. Laparoscopic bile duct injuries: management at a tertiary liver center. Am Surg. 2004; 70:906–909. PMID:
15529848.
9. Moore DE, Feurer ID, Holzman MD, Wudel LJ, Strickland C, Gorden DL, et al. Long-term detrimental effect of bile duct injury on health-related quality of life. Arch Surg. 2004; 139:476–481. PMID:
15136346.

10. Misra S, Melton GB, Geschwind JF, Venbrux AC, Cameron JL, Lillemoe KD. Percutaneous management of bile duct strictures and injuries associated with laparoscopic cholecystectomy: a decade of experience. J Am Coll Surg. 2004; 198:218–226. PMID:
14759778.

11. Gentileschi P, Di Paola M, Catarci M, Santoro E, Montemurro L, Carlini M, et al. Bile duct injuries during laparoscopic cholecystectomy: a 1994-2001 audit on 13,718 operations in the area of Rome. Surg Endosc. 2004; 18:232–236. PMID:
14691705.

12. Kaman L, Sanyal S, Behera A, Singh R, Katariya RN. Comparison of major bile duct injuries following laparoscopic cholecystectomy and open cholecystectomy. ANZ J Surg. 2006; 76:788–791. PMID:
16922899.

13. Ahrendt SA, Pitt HA. Surgical therapy of iatrogenic lesions of biliary tract. World J Surg. 2001; 25:1360–1365. PMID:
11596904.

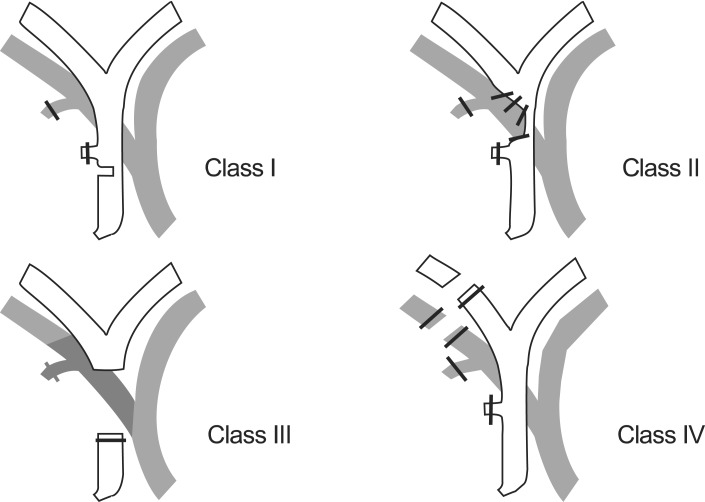
14. Bismuth H, Majno PE. Biliary strictures: classification based on the principles of surgical treatment. World J Surg. 2001; 25:1241–1244. PMID:
11596882.

15. Stewart L, Domingez CO, Way LW. Bile duct injuries during laparoscopic cholecystectomy: a sensemaking analysis of operative reports. In : Mosier K, Fischer U, editors. Proceedings of the 8th International NDM Conference. 2007 Jun; Pacific Grove, CA. [publisher unknown]: 2007.
16. Bektas H, Schrem H, Winny M, Klempnauer J. Surgical treatment and outcome of iatrogenic bile duct lesions after cholecystectomy and the impact of different clinical classification systems. Br J Surg. 2007; 94:1119–1127. PMID:
17497652.

17. Mattox KL, Feliciano DV, Moore EE. Trauma. 3rd ed. Stamford, CT: Applenton & Lange;1996. p. 515–519.
18. Schmidt SC, Settmacher U, Langrehr JM, Neuhaus P. Management and outcome of patients with combined bile duct and hepatic arterial injuries after laparoscopic cholecystectomy. Surgery. 2004; 135:613–618. PMID:
15179367.

19. Bergman JJ, van den Brink GR, Rauws EA, de Wit L, Obertop H, Huibregtse K, et al. Treatment of bile duct lesions after laparoscopic cholecystectomy. Gut. 1996; 38:141–147. PMID:
8566842.

20. Csendes A, Navarrete C, Burdiles P, Yarmuch J. Treatment of common bile duct injuries during laparoscopic cholecystectomy: endoscopic and surgical management. World J Surg. 2001; 25:1346–1351. PMID:
11596901.

21. Lau WY, Lai EC. Classification of iatrogenic bile duct injury. Hepatobiliary Pancreat Dis Int. 2007; 6:459–463. PMID:
17897905.
22. Sahajpal AK, Chow SC, Dixon E, Greig PD, Gallinger S, Wei AC. Bile duct injuries associated with laparoscopic cholecystectomy: timing of repair and long-term outcomes. Arch Surg. 2010; 145:757–763. PMID:
20713928.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download