Abstract
Superior mesenteric vein (SMV) thrombosis caused by acute appendicitis is a very rare entity nowadays. We report a successfully treated case of a 21-year-old man with SMV thrombosis associated with severe acute appendicitis. Intravenous heparin was administered, and it was later substituted with warfarin. Systemic antibiotic therapy was continued for 1 week, and it was substituted with oral antibiotics, which were administered for 3 weeks. On the 45th postoperative day, follow-up computed tomography scan demonstrated dissolution of SMV thrombosis. Anticoagulation therapy was maintained for 3 months. He was discharged without any complications. SMV thrombosis can be treated successfully with emergency appendectomy, broad-spectrum antibiotics, and anticoagulation therapy.
Go to : 
Superior mesenteric vein (SMV) thrombosis caused by appendicitis is a very rare entity in the recent times due to improved high quality imaging techniques and use of broad spectrum antibiotics. However, it is important to be aware of the possibility of SMV thrombosis while managing patients with appendicitis as the mortality rate in SMV thrombosis associated with intra-abdominal infection was reported to be 30%-50%,1,2,3 with SMV thrombosis possibly causing intestinal edema, congestion, and necrosis. Moreover, the nonspecific symptoms of SMV thrombosis render the clinical diagnosis difficult and delayed.4
Go to : 
A 21-year-old male was transferred to the emergency department with a chief complaint of lower abdominal pain, nausea, and fever for 4 days. He had no past medical history or had not undergone any examination for assessing the coagulation status. He denied any family history of deep vein thrombosis or other coagulation disorder.
On arrival, his body temperature was 39.1℃, pulse rate was 104/minutes, respiratory rate was 18/minutes, and blood pressure was 108/49 mmHg. The abdomen was distended and rigid. Tenderness and rebound tenderness in the right lower quadrant of the abdomen were observed.
Blood analysis showed a white blood cell count of 10,870/µl (neutrophils 91.8%), platelet count of 80,000/µl, C-reactive protein level of 14.94 mg/dl, erythrocyte sedimentation rate of 17 mm/hr, total bilirubin level of 2.6 mg/dl, aspartate aminotransferase level of 47 IU/L, alanine aminotransferase level of 67 IU/L, and prothrombin time of 13.1 seconds (international normalized ratio 1.36).
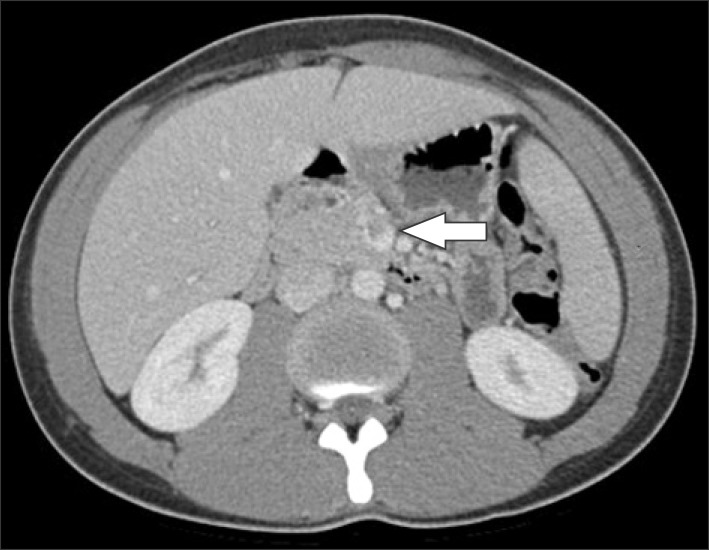
On the computerized tomography (CT) scan, appendicitis with a periappendiceal abscess and a non-occlusive thrombus in the SMV were noted (Fig. 1).
After performing blood culture, systemic intravenous antibiotics were started (ceftriaxone 2 g daily+metronidazole 500 mg thrice daily). Additional laboratory tests for measuring the coagulability state were also performed.
The patient underwent emergent laparoscopic appendectomy and monitoring for the occurrence of bowel infarction was performed. The postoperative course was uneventful.
Microorganisms were not found in the culture and coagulopathy was not detected. The fibrinogen degradation product level was <5 µg/ml (normal <5), and D-dimer level was <0.20 mg/L (normal <0.5). Antithrombin III (104%, normal 80-120%), protein C activity (86%, normal 70-130), protein S activity (91%, normal 77-143), and homocysteine levels (10.92 umol/L, normal 5.08-15.40) were within their normal ranges. The lupus anticoagulant screening test was negative and the level of anti-phospholipid antibodies (Ig G 3.2 GPL/ml, normal<10.0; IgM 1.0 MPL/ml, normal <10.0) was below the normal range.
On the 7th postoperative day, follow-up CT scan was performed and it showed a nearly occlusive thrombus in the SMV. There was no evidence of ischemic enteritis or active bleeding. Intravenous heparin administration was started, and it was later substituted with warfarin.
Systemic antibiotic therapy was continued for 1 week, and it was substituted with oral antibiotics (cefaclor 250 mg thrice daily), which were administered for 3 weeks.
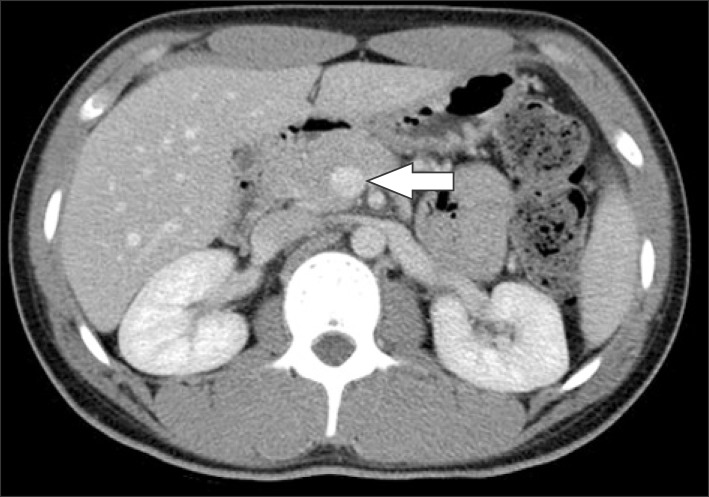
On the 45th postoperative day, follow-up CT scan demonstrated dissolution of SMV thrombosis (Fig. 2). Anticoagulation therapy was maintained for 3 months.
Go to : 
Pylephlebitis is defined as infective suppurative thrombosis of the portal vein or its branches. Infection in the organs that drains into the portal venous system possibly causes pylephlebitis. Diverticulitis is the most common cause, followed by appendicitis, cholecystitis, pancreatitis, tumors, and abdominal and pelvic infection.5 The primary source of infection was detected in 70% of the cases.6 Causative microorganisms are identified often, and E. coli, bacteroides fragilis, proteus mirabilis, klebsiella pneumoniae, and enterobacter spp. are the most common pathogens.1,7 However, in this case, microorganisms were not identified in blood culture. Recently, blood culture has become a very important test due to the resistance to antibiotics as antibiotic regimen could be reassessed for de-escalation.
The incidence of SMV thrombosis caused by appendicitis was approximately 0.4% before 1950, following which it has become an extremely rare entity because of adequate antibiotic use and prompt surgical treatment.8 The mortality rate was as high as 80%,7,9 and it has decreased to 30%-50%; however, it is still high enough for considering this entity important.
When the diagnosis of pylephlebitis is confirmed, appropriate treatment should be started promptly. Removal of the source of infection and a course of systemic broad spectrum antibiotics effective against common causative organisms are essential. Although Stlitzenberg et al.10 reported about interval appendectomy and Nishimori et al.2 reported about appendectomy with thrombectomy by using Fogarty catheter, emergency appendectomy is usually recommended.11 In this case, emergent appendectomy without manipulating SMV thrombosis was performed. Ceftriaxone and metronidazole were administered for 1 week for Gram-negative bacilli and anaerobes, and oral cefaclor (2nd-generation cephalosporin) was used consecutively for 3 weeks. The duration of use of antibiotics was determined based on previous studies.3,12,13
The use of anticoagulation therapy in the treatment of pylephlebitis is the most controversial issue. Some reports recommended using anticoagulation therapy to reduce the recurrence rate and mortality rate of pylephlebitis.2,14,15 However, Crowe et al.16 reported that anticoagulation therapy is not necessary for pylephlebitis when the primary disease such as appendicitis or diverticulitis is well-controlled. In this case, anticoagulation therapy was not started initially. After the follow-up CT scan performed on the 7th postoperative day revealed aggravation of SMV thrombosis which was nearly occlusive, anticoagulation therapy was started. Patient recovered without any catastrophic complications such as intestinal ischemia or necrosis, but early initiation of anticoagulation therapy could lead to safer management.
In conclusion, SMV thrombosis is a very rare complication of appendicitis; but it can lead to catastrophic consequences. SMV thrombosis can be treated successfully with emergency appendectomy, broad-spectrum antibiotics, and anticoagulation therapy.
Go to : 
References
1. Baril N, Wren S, Radin R, Ralls P, Stain S. The role of anticoagulation in pylephlebitis. Am J Surg. 1996; 172:449–452. PMID: 8942542.

2. Nishimori H, Ezoe E, Ura H, Imaizumi H, Meguro M, Furuhata T, et al. Septic thrombophlebitis of the portal and superior mesenteric veins as a complication of appendicitis: report of a case. Surg Today. 2004; 34:173–176. PMID: 14745623.

3. Plemmons RM, Dooley DP, Longfield RN. Septic thrombophlebitis of the portal vein (pylephlebitis): diagnosis and management in the modern era. Clin Infect Dis. 1995; 21:1114–1120. PMID: 8589130.

4. Singh P, Yadav N, Visvalingam V, Indaram A, Bank S. Pylephlebitis--diagnosis and management. Am J Gastroenterol. 2001; 96:1312–1313. PMID: 11316205.

5. Saxena R, Adolph M, Ziegler JR, Murphy W, Rutecki GW. Pylephlebitis: a case report and review of outcome in the antibiotic era. Am J Gastroenterol. 1996; 91:1251–1253. PMID: 8651182.
6. Waxman BP, Cavanagh LL, Nayman J. Suppurative pyephlebitis and multiple hepatic abscesses with silent colonic diverticulitis. Med J Aust. 1979; 2:376–378. PMID: 390346.
7. Balthazar EJ, Gollapudi P. Septic thrombophlebitis of the mesenteric and portal veins: CT imaging. J Comput Assist Tomogr. 2000; 24:755–760. PMID: 11045699.

8. Chang TN, Tang L, Keller K, Harrison MR, Farmer DL, Albanese CT. Pylephlebitis, portal-mesenteric thrombosis, and multiple liver abscesses owing to perforated appendicitis. J Pediatr Surg. 2001; 36:E19. PMID: 11528636.

9. Dean JW, Trerotola SO, Harris VJ, Snidow JJ, Hawes D. Percutaneous management of suppurative pylephlebitis. J Vasc Interv Radiol. 1995; 6:585–588. PMID: 7579869.

10. Stitzenberg KB, Piehl MD, Monahan PE, Phillips JD. Interval laparoscopic appendectomy for appendicitis complicated by pylephlebitis. JSLS. 2006; 10:108–113. PMID: 16709373.
11. Kasper DL, Sahani D, Misdraji J. Case records of the Massachusetts General Hospital. Case 25-2005. A 40-year-old man with prolonged fever and weight loss. N Engl J Med. 2005; 353:713–722. PMID: 16107625.
12. Lim HE, Cheong HJ, Woo HJ, Kim WJ, Kim MJ, Lee CH, et al. Pylephlebitis associated with appendicitis. Korean J Intern Med. 1999; 14:73–76. PMID: 10063317.

13. Vanamo K, Kiekara O. Pylephlebitis after appendicitis in a child. J Pediatr Surg. 2001; 36:1574–1576. PMID: 11584411.

14. Condat B, Pessione F, Helene Denninger M, Hillaire S, Valla D. Recent portal or mesenteric venous thrombosis: increased recognition and frequent recanalization on anticoagulant therapy. Hepatology. 2000; 32:466–470. PMID: 10960436.

15. Karam MM, Abdalla MF, Bedair S. Isolated superior mesenteric venous thrombophlebitis with acute appendicitis. Int J Surg Case Rep. 2013; 4:432–434. PMID: 23500734.

16. Crowe PM, Sagar G. Reversible superior mesenteric vein thrombosis in acute pancreatitis. The CT appearances. Clin Radiol. 1995; 50:628–633. PMID: 7554738.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download