This article has been
cited by other articles in ScienceCentral.
Abstract
The conventional management of pancreatoenteric fistulas and pancreatic abscess with aggressive surgery or percutaneous drainage catheter placement are associated with increased surgery-related morbidity and mortality, and a longer hospitalization. We report here a case of successful closing pancreatoduodenal fistula, which remained open after the percutaneous catheter drainage of pancreatic abscess, by using vascular coil embolization and fibrin glue injection. This procedure is a less invasive, more effective and better tolerated strategy for the management of pancreatoenteric fistula in a selected group of high risk patients and needs further investigation.
Go to :

Keywords: Pancreatoduodenal fistula, Embolization, Fibrin glue
IINTRODUCTION
Pancreatoenteric fistulas and pancreatic abscess are rare complications of severe acute pancreatitis
1,
2 and their traditional management which includes aggressive surgery or percutaneous drainage catheter placement is associated with increased surgery-related morbidity and mortality as well asa longer hospitalization.
3,
4 Recently, a variety of occlusion methods of external or internal pancreatic fistula performed with minimally invasive techniques such as endoscopy and fibrin glue sealant.
5,
6 We here report a case of successfull closure of pancreatoenteric fistula, which remained open after the percutanous catheter drainage of pancreatic abscess,using vascular coil embolization and fibrin glue injection. This procedure is a less invasive, more effective and better tolerated strategy for the management of pancreatoenteric fistula in a selected group of high risk patients.
Go to :

CASE
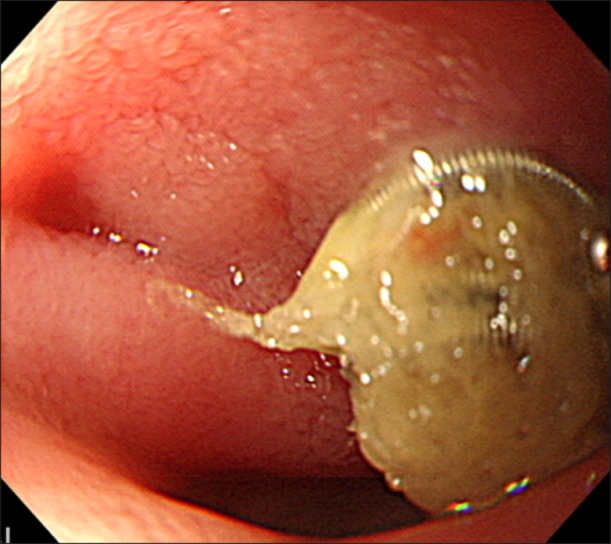
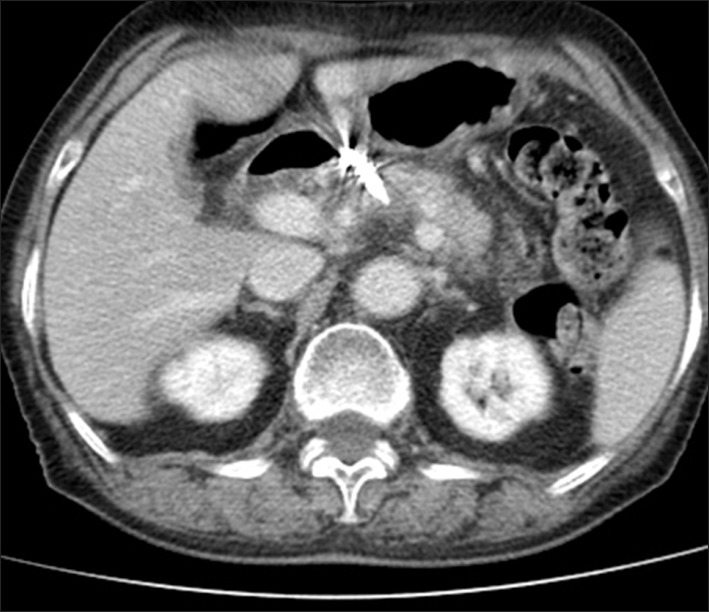
A 79-year-old female patient with initial presentation of acute biliary pancreatitis and cholecystitis and subsequently underwent uneventful laparoscopic cholecystectomy. Three days after the hospital discharge, she was admitted with epigastric pain and diarrhea. Abdominal computed tomography (CT) scan on admission revealed a new air containing peripancreatic abscess, while the pancreas swelling and infiltration were significantly improved, when compared with her previous abdominal CT scan (
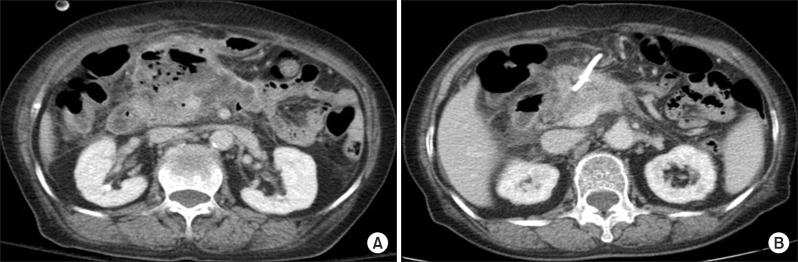
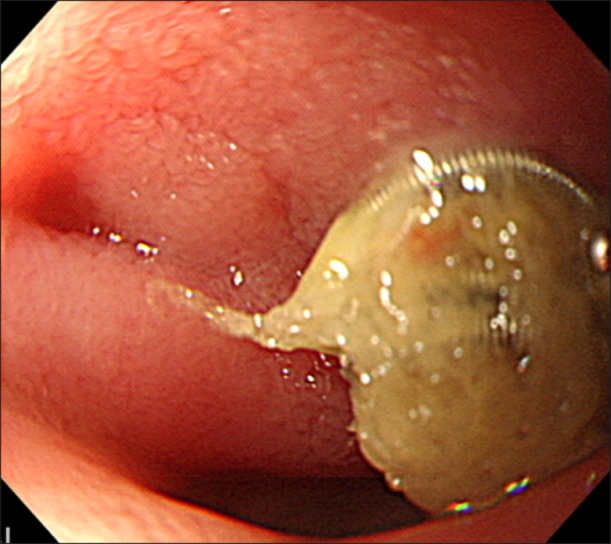
Fig. 1). The laboratory tests were unremarkable except elevated levels of white blood cell count (18,100/µl) and CRP (13 mg/dl). During the process of inserting a percutaneous pigtail catheter to drain the abscess, we detected two fistulous tracts between a pancreatic abscess and the medial side of duodenum (
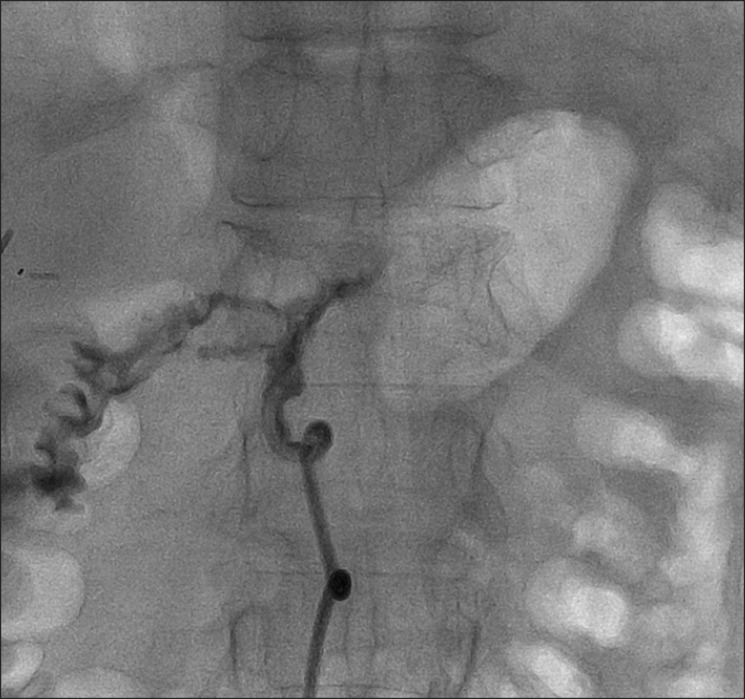
Fig. 2). The subsequent esophagogastroduodenoscopy (EGD) confirmed a fistulous hole with pus draining into the duodenal wall (
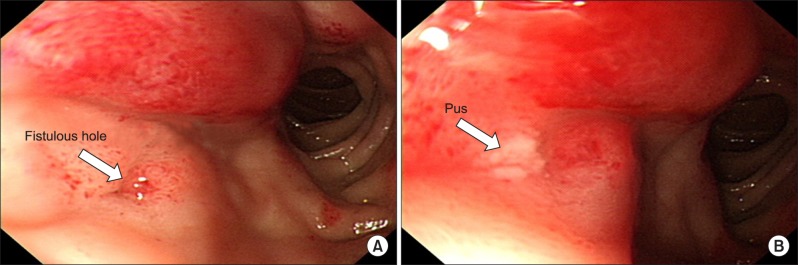
Fig. 3) and approximately 10-20 ml per day of yellowish pus drained through the catheter. After a week of catheter drainage, the follow-up tubography and abdominal CT scan indicated that the fistulous tract remained open while the size of abscess reduced significantly. We attempted to close the fistula tract initially with the injection of 1 : 1 mixture of tissue adhesive glue (Histoacryl; B/Braun, Tuttlingen, Germany) and radiopaque fluid (Lipiodol Ultra-Fluide; Guerbet, Aulnay-sous-Bois, France) using an 8-Fr sheathed catheter and microcatheter without any success. At the third week of the catheter placement, when the drainage was decreased to 5-10 ml per day (
Fig. 4), a vascular occluding coil embolization (Nester Embolization Coil, 0.035 inch, 4 mm×14 cm; Cook Incorporated, Bloomington, IN, USA) was carried out and, subsequently, 2 ml of fibrin glue (Greenplast; Green Cross, Seoul, Korea) as a filling was injected (
Fig. 5). The patient well tolerated the procedure without any complications. On the third day after coil embolization, the follow up tubography showed the successful closure of fistulous tract. The patient was discharged without catheter and monitored after discharge with CT scan and EGD regularly up to 6 months (
Fig. 6). The patient remained asymptomatic.
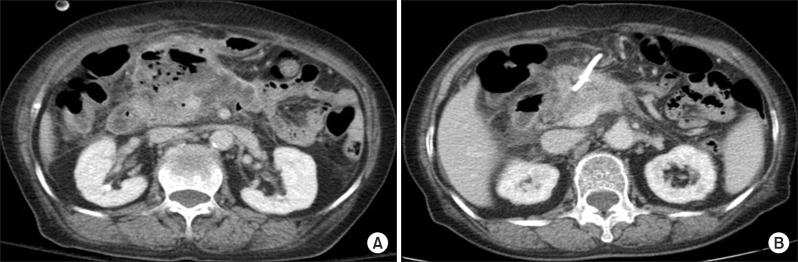 | Fig. 1Abdomen CT scan showing air-containing peripancreatic abscess (A). Pancreas swelling and infiltration were improved after percutaneous drainage (B). 
|
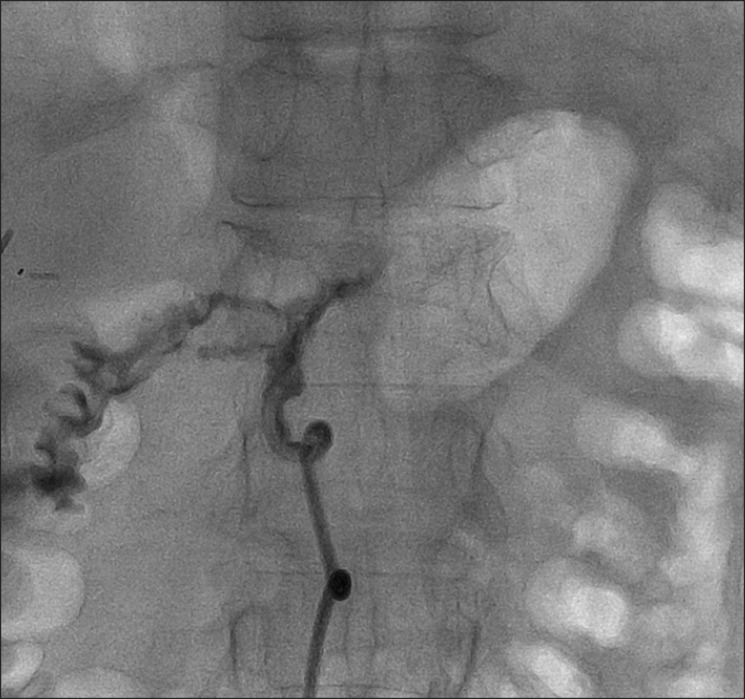 | Fig.2Direct visualization of the two fistulous tracts between a pancreatic abscess and the medial side of duodenum. 
|
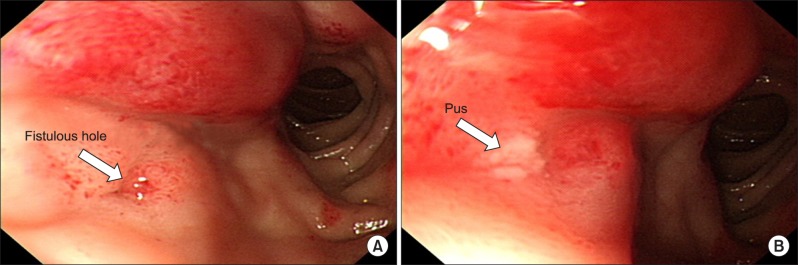 | Fig. 3Esophagogastroduodenoscopic findings showing a fistulous hole (A) with pus draining into the duodenal wall (B). 
|
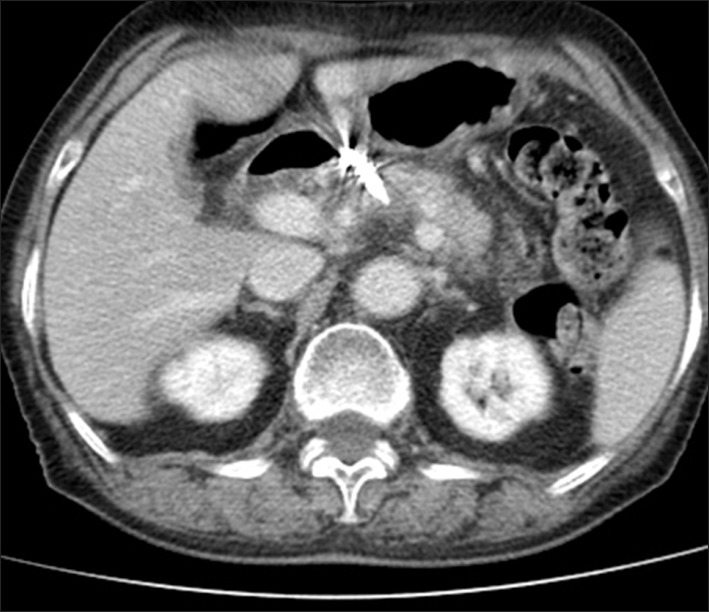 | Fig. 4Abdomen CT scan showing improvement of peripancreatic abscess. 
|
 | Fig. 5Occlusion of the fistula tract with coils and fibrin glue. 
|
 | Fig. 6Follow-up esophagogastroduodenoscopic finding showing no recurrence of fistula. 
|
Go to :

DISCUSSION
The conventional management of pancreatoenteric fistulas and pancreatic abscess with aggressive surgery or percutaneous drainage catheter placement are associated with increased surgery-related morbidity and mortality, and a longer hospitalization.
3,
4,
7,
8 Though the peripancreatic abscess may be addressed by various drainage methods the complete closure of the entire fistula remains difficult. Recently, a variety of occlusion methods of external or internal pancreatic fistula are reported with minimally invasive techniques such as endoscopy and fibrin glue sealant. Recently, a long list of embolic agents, including blood clots, gelatin, silicon rubber plugs, various sponge materials, fibrin glue, metallic coils, have been introduced and the endobronchial vascular occlusion coils for control of a bronchopleural fistula has been reported.
9,
10
In the present case, we attempted to close the fistula tract initially by injecting tissue adhesive glue mixed with radiopaque fluid, which is generally used by interventional radiology field, however, we did not succeed. Several weeks later, when the drainage was decreased 5-10 ml per day, we used metallic coils and fibrin glue as filler which is successfully closed the fistula tract.
The present case is a rare example of a pancreatoenteric fistula which remained open after the percutaneous catheter drainage of pancreatic abscess is successfully closed by using vascular coil embolization and fibrin glue injection. We believe this is a less invasive, more effective, and better tolerated strategy for the management of pancreatoenteric fistula in a selected group of high risk patients, and needs further investigation.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download