Abstract
Backgrounds/Aims
Common bile duct (CBD) exploration has been a procedure necessary to remove stones which are not removable by endoscopic sphincterotomy (EST). T-tube was installed mainly in the concern of bile leakage after procedure. But T-tube itself can only cause bile peritonitis and thus, prolonged discomfort and care after operation. In addition, in the era of laparoscopy, T-tube insertion adds much operation time and is technically difficult for installation during the procedure.
Methods
Our case of open cholecystectomy and primary closure of CBD not leaving T-tube (n=28, group I) with reports dating from July 1998 to June 2007 is presented here to see whether primary closure without T-tube is safe as compared with T-tube inserted cases performed at the same center (n=15, group II). Operative cholangiography, CT scan, ultrasound and biochemical data were followed up for both groups and surveyed on operative complications as well to determine the outcomes.
Results
Bile leakage in 1, recurrent stone in 2 and obstructive jaundice in 1 were all considered during the follow up period among 28 group I patients (n=6), when compared to T-tube inserted group II patients with 2 bile peritonitis, 1 residual stones and 1 pancreatitis (n=4), showing no meaningful differences (p=0.07).
Go to : 
Choledochotomy to remove stones in biliary tree via open method was mainly carried out when endoscopic retrograde cholangiopancreaticography (ERCP) with endoscopic spincterotomy (EST) failed to remove them, or when imminent septic condition is threatening patient's life under instable diagnosis. At the end of above procedure, after opening and removing of stones from the common bile duct (CBD), by installing a T-tube through choledochotomy is suggested to be a classical method from beginning of the choledochotomy procedures since the end of the 19th century. T-tube is supposed to a draining route of bile juice outside the body to avoid bile peritonitis when leaking bile into peritoneal cavity through repaired wound of bile duct occurrence, and supposedly a route to evaluate and remove the possible remaining CBD stones additionally, and to reduce the chance of constriction of CBD later. But installing T-tube leaves room for debate in the sense that it causes bile peritonitis before and after the removal of tube,1-4 discomfort and prolonged out-patient care. When it comes to laparoscopic choledochotomy, albeit recent developments in instruments, due to technical demanding of choledochotomy and prolonged operation time, mostly in putting up the T-tube and closing the incision wound securely, there are limitations in adopting the procedure.
Recently, one step laparoscopic cholecystectomy and choledochotomy sparing ERCP or EST,5,6 method using pigtail,7 or installing endoscopic naso-biliary drainage (ENBD) tube before operation,8-12 and other methods like transcystic approach of CBD13,14 were initiated at various centers hoping to evade T-tubing, but we have treated patients in the most typical way by applying laparoscopic cholecystectomy after removal of bile duct stones by ERCP and EST, and also by applying open cholecystectomy and choledochotomy when endoscopic procedures could not remove stones in bile duct under many reasons.
Here we present the clinical outcomes of 28 cases of open choledochotomies and primary closure sparing installment of T-tubes, from May 1998 to April 2007.
Go to : 
We reviewed retrospectively traceable patients who underwent open cholecystectomy and choledochotomy sparing T-tube (Group I, n=28) or with T-tube (Group II, n=15) among total of 53 operated patients.
All patients without T-tube had CBD diameter more than 11 mm on the outside, which is the little finger distal phalangeal diameter of operator, and thus, operation was conducted by one surgeon choosing choledochotomy closure methods alternatively.
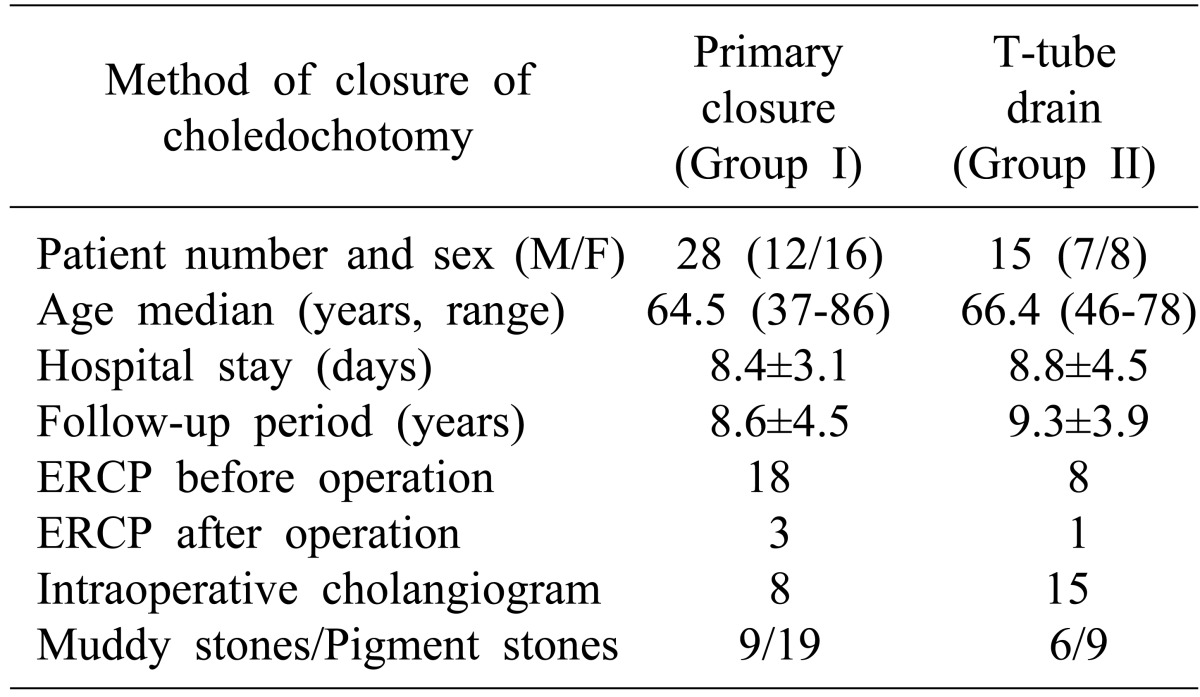
Patients' basic clinical feature is as shown in Table 1.
We followed up on patient's age, sex, condition of lesion, diameter of CBD at choledochotomy incision line before opening it, distribution and features of stones, operation method, status of early or late morbidity.
Means of interval follow up of patients and its results were mainly reviewed through liver function tests, CT scans, abdominal ultrasonography, or by ERCP as needed according to the condition of patients.
Cases of recurrent CBD stone, intrahepatic duct stone causing obstruction, previously performed choledoch-jejunostomy or anything else were excluded because of the altered chances of morbidities. Cases of recurrent CBD stone, intrahepatic duct stone causing obstraction, previously performed choledoch-jejunostomy or anything else were excluded because of possible chances of morbidities.
Laparotomy was performed through the right paramedian transrectus epigastric vertical incision, and longitudinal incision of CBD at its anterior portion was made at the most easily-exposed area near the origin of cystic duct, through which stones were removed and operative cholangiogram or cholangiography was carried out as needed.
Stone removal was made using stone forceps, Baker's dilator with saline irrigation by Nelaton tubing, and the patency of CBD to duodenum was confirmed by Nelaton catheter passed into duodenum and observing any regurgitation of saline shot through the occurence. Choledochotomy always accompanied cholecystectomy.
Choledochotomy was closed by 5-0 Vicryl suture material by continuous suturing in group I patients (n=28) primarily, and T-tube was installed in group II patients (n=15) using the same material and closure method. After then, leakage of bile was performed macroscopically, or else, cholangiogram was added to ensure the remaining stone or bile leakage for the suspected cases.
Negative suction drain was left from the operative area through the right flank to observe bile leakage from choledochotomy or other complications, and was usually removed around the postoperative 7th day.
Stapled skin wound was undone on postoperative 7th day, which was, however, delayed till 14th day when concerned about senile age or wound conditions.
Most patients were recommended postoperatively to routine labs, and scout films from 2 weeks to about 3 months, and to visit outpatient clinics once a year for interval check-ups on conditions. T-tube was removed on postoperative 28th day at the outpatient clinic. Ultrasonography, CT scan, or ERCP were executed on suspected patients whom have recurrences of stones or complications.
T-tube inserted patients, and complications were analyzed by chi-square test, giving statistical meaning when p<0.05, with 95% confidence interval. Specific data, like mortality, less than 5 were all regarded as insignificant.
Go to : 
In 43 cases of traceable patients of cholecystectomy, two cases of group II were carried out by laparoscopic choledochotomy and others via laparotomy.
Demography of patients was comparable between each groups, and to other reports in terms of age, sex, rate of complications, and follow up methods, except for differences in old-aged onsets of cholangitis and female predominant patient populations in the western area.
Hospital stays after the operation was similar between the groups, thus, indicating indifferences in recovery time at hospitals.
Characteristics of CBD stones, whether muddy or stony, were not related with operative indications or complications.
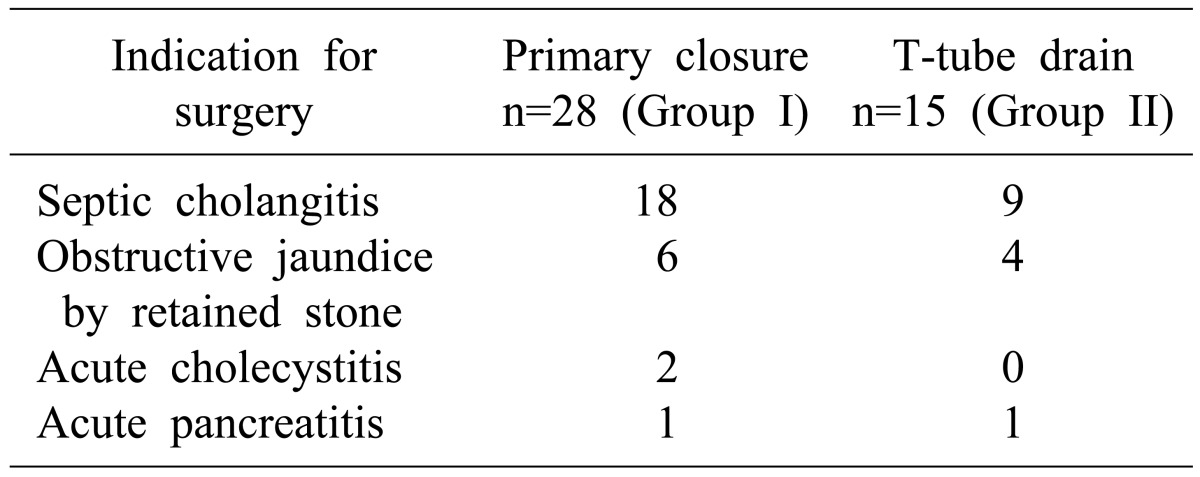
Various indications of operations were imminent septic conditions after the failure of CBD stone removals using ERCP and EST, previous gastric resection and Billroth II anastomosis state blocking endoscopic CBD stone removal, or refractory cholangitis or pancreatitis to antibiotics leading to septic condition (Table 2).
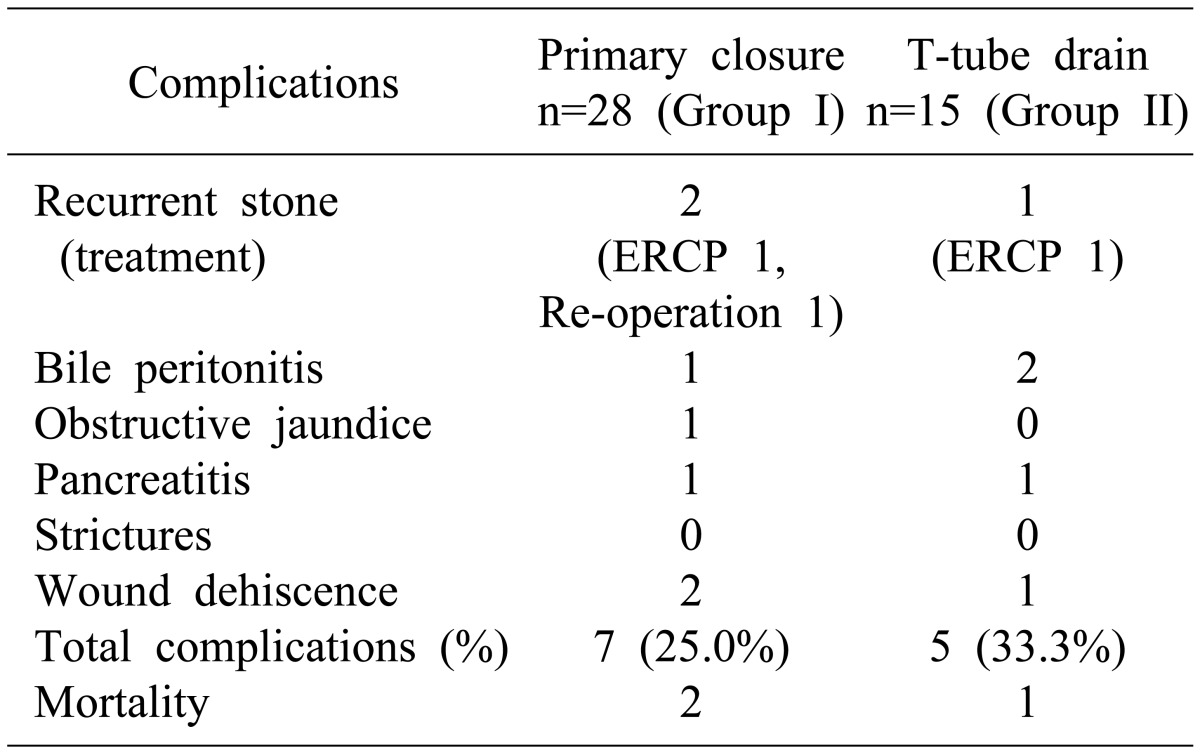
Complications after operation was compared between group I and II patients, which was 7, and 5 cases, respectively (p=0.07), as shown on Table 3. This was not statistically different, indicating that complication rates between primary closure patients and T-tube inserted patients showed no differences in complication rates.
In group I patients, 2 cases of immediate postoperative ERCP were due to pancreatic jaundice and suspected remnant CBD stones, and no such cases were found in group II patients. Another ERCP was necessary for patient in group I with patients having suspected recurrent CBD stones after more than 6 months of operation.
Recurrent stones were detected on 2, 1 case from each group I and II. Two cases in group I were managed by reoperations and ERCP accordingly, and 1 case in group II was cured by reoperation, which happened 6 months after initial operation thus, making us confused whether the stone was recurrent or retained.
Bile peritonitis after operations occurred in 1 and 2 cases within each group I and II. One case in group I was leaking of bile into peritoneal cavity through separated upper edge of closed line choledochotomy, and the leaking continued even after T-tube inserting reoperations causing bile peritonitis and multi-organ failures leading to death. Two cases of bile peritonitis in group II were managed successfully by keeping drainage.
Wound dehiscence appeared on 2 cases in group 2 and 1 case of group II. All the cases were over 75 years old of age, and were cured by irrigation and re-approximation.
Obstructive jaundice in 1 case of group I derived from pancreatic edema without apparent evidences of pancreatitis, and was subsided 20 days after operation.
Each one of the case of postoperative pancreatitis in group I and II was recovered uneventfully through routine care.
Postoperative 30-day mortality occurred in 2, 1 case from each group respectively.
A case of death in group I had bile peritonitis complicating conditions to wound dehiscence and sepsis which eventually lead to death as described above. Causes of mortalities amongst others were: one with pneumonia and pleural effusion with resultant multi-organ failure, and one with congestive heart failure from myocardial infarction. Thus, the mortality rates between group I and II showed no difference, though it was not evaluated statistically because of the small amounts.
Go to : 
Questions on the necessity of T-tube installments at the end of choledochotomy, be it open or laparoscopic, were sustained by virtue of recent developments in perioperative diagnostic tools and operative instruments with techniques.
As the experience of laparoscopic choledochotomy increases, the technical demanding and prolonged operation time in T-tube insertion has been replaced by primary closures, ENBD, pigtail intubations,14 and other ways to aid decompressions of CBD postoperatively with allegedly successful results.
Recently, many reports were published on successful primary closures of choledochtomy wounds without T-tube during open or laparoscopic procedures without devices of the CBD drainage,1,2,15-19 thus, resulting in even more successful healings of choledochotomy without T-tube in some cases20 similar to our experience.
Usually before the operation, we are all well-informed about the stone patterns in the biliary tree, and through more meticulous operative procedures focusing on CBD clearance and patency, possibilities of retained stones are mostly negligible. That fact raises more suspicion on the necessity of T-tube installments and makes us ask whether the T-tube bile drainage would help healing of choledochotomy wound to be more secure. Moreover, through primary closures, we could expect reduced patient discomforts one month postoperatively for the maturation time and thus, followed by financial benefits.
We traced 28 cases of primary closures without T-tube (group I) and 15 cases of T-tube stenting (group II) during the period of 10-year experience showing statistically insignificant different complication rates, and less leakage rates of bile through closed choledochotomy when primarily closed in 1 case of the group I than in 2 cases of T-tube inserted group II patients.
We did not practice transcystic choledocotomy after a few trials, due to its inconveniences in getting good operation field, as most insertions of cystic duct to CBD was rather posteriorly positioned and often too near to the pancreatic upper border.
Stenting of ampulla of Vater at the end of choledochotomy21 was also not practiced, considering financial issues and troublesome removals. Instead, two cases of primary closure patients kept ENBD postoperatively for suspected retained stones in CBD which was proven to be negative at the end, but contributed to good drainage of immediate bile postoperatively which helped the healing of choledochotomy wound when the classic concept is applied.
Effects of T-tube drainage of bile for decompression to aid choledochotomy wound healing by keeping down intraluminal pressures of CBD seemed to be not the case when considering our cases of choledochotomies. Among 27 successful primary closure patients in group I, 8 cases were drained by ENBD (n=2) and EST (n=6), while the other 10 cases were left intact for ampulla of Vater perioperatively, thus, maintaining normal CBD physiologic secretions and intraluminal pressures. Decompressions of CBD by EST or no drains at all did not affect wound healing results in primarily closed choledochotomy. Besides, the T-tube drained 13 cases of group II patients also showed uneventful healings of choledochotomy wound healing, representing intraluminal pressure is not an issue for healing of CBD incision wound.
Two cases of bile peritonitis from leaking occurred to T-tube drained group II patients, in a rather young age of 54 and 62 years unexpectedly, but both of them were cured smoothly by keeping drainage and supportive care. Their ampulla of Vater remained intact perioperatively. Leakage through choledochotomy suspected to be through the side hole of T-tube could be healed under normal pressures of CBD, offering another example of evidence to healing the choledochotomy wound whether being drained or not, or whether it was under decompression or kept within normal intraluminal CBD pressure.
Failures of choledochotomy wound healing, leading to bile peritonitis and septic multiorgan failure and to death, occurred in 1 case of group I patient, an 86-year-old male patient under imminent septic condition by large CBD stones, which hastened operation, and efforts to save operation time included omitting the T-tube installment. After performing reoperation using T-tube, leakage occurred and sepsis was aggravated leading to death.
On balance, although the T-tubes have effects on elucidation of residual stones in immediate CBD postoperatively, it has no room for helping with the healing of choledochotomy wounds by decompression. When the operation is confronted with suspicious retained stones in CBD at the end, leaving the ENBD in position could be an option for additional endoscopic stone removal procedures. Recent laparoscopic trials of choledochotomy and primary closure can be accepted as feasible as it prevails.22,23
Go to : 
References
1. Zhu QD, Tao CL, Zhou MT, et al. Primary closure versus T-tube drainage after common bile duct exploration for choledocholithiasis. Langenbecks Arch Surg. 2011; 396:53–62. PMID: 20582601.

2. Ambreen M, Shaikh AR, Jamal A, et al. Primary closure versus T-tube drainage after open choledochotomy. Asian J Surg. 2009; 32:21–25. PMID: 19321398.

3. Leida Z, Ping B, Shuguang W, et al. A randomized comparison of primary closure and T-tube drainage of the common bile duct after laparoscopic choledochotomy. Surg Endosc. 2008; 22:1595–1600. PMID: 18202889.

4. Wills VL, Gibson K, Karihaloot C, et al. Complications of biliary T-tubes after choledochotomy. ANZ J Surg. 2002; 72:177–180. PMID: 12071447.

5. Memon MA, Hassaballa H, Memon MI. Laparoscopic common bile duct exploration: the past, the present, and the future. Am J Surg. 2000; 179:309–315. PMID: 10875992.

6. Campbell-Lloyd AJ, Martin DJ, Martin IJ. Long-term outcomes after laparoscopic bile duct exploration: a 5-year follow up of 150 consecutive patients. ANZ J Surg. 2008; 78:492–494. PMID: 18522572.

7. Kanamaru T, Sakata K, Nakamura Y, et al. Laparoscopic choledochotomy in management of choledocholithiasis. Surg Laparosc Endosc Percutan Tech. 2007; 17:262–266. PMID: 17710045.

8. Martínez Cecilia D, Valentí Azcárate V, Qurashi K, et al. Advantages of laparoscopic stented choledochorrhaphy. Six years experience. Cir Esp. 2008; 84:78–82. PMID: 18682185.
9. Tang CN, Tai CK, Ha JP, et al. Antegrade biliary stenting versus T-tube drainage after laparoscopic choledochotomy--a comparative cohort study. Hepatogastroenterology. 2006; 53:330–334. PMID: 16795965.
10. Pérez G, Escalona A, Jarufe N, et al. Prospective randomized study of T-tube versus biliary stent for common bile duct decompression after open choledocotomy. World J Surg. 2005; 29:869–872. PMID: 15951939.

11. Wani MA, Chowdri NA, Naqash SH, et al. Primary closure of the common duct over endonasobiliary drainage tubes. World J Surg. 2005; 29:865–868. PMID: 15951929.

12. Wei Q, Hu HJ, Cai XY, et al. Biliary drainage after laparoscopic choledochotomy. World J Gastroenterol. 2004; 10:3175–3178. PMID: 15457567.

13. Wu JS, Soper NJ. Comparison of laparoscopic choledochotomy closure techniques. Surg Endosc. 2002; 16:1309–1313. PMID: 12235508.

14. Chen CC, Wu SD, Tian Y, et al. The fading role of T-tube in laparoscopic choledochotomy: primary choledochorrhaphy and over pigtail j and endonasobiliary drainage tubes. J Laparoendosc Adv Surg Tech A. 2010; 20:807–811. PMID: 21029026.

15. Naraynsingh V, Hariharan S, Ramdass MJ, et al. Open common bile duct exploration without T-tube insertion- two decade experience from a limited resource setting in the Caribbean. Indian J Surg. 2010; 72:185–188. PMID: 23133244.

16. Yin Z, Xu K, Sun J, et al. Is the end of the T-tube drainage era in laparoscopic choledochotomy for common bile duct stones is coming? A systematic review and meta-analysis. Ann Surg. 2013; 257:54–66. PMID: 23059495.

17. Cai H, Sun D, Sun Y, et al. Primary closure following laparoscopic common bile duct exploration combined with intraoperative cholangiography and choledochoscopy. World J Surg. 2012; 36:164–170. PMID: 22086256.

18. Savita KS, Bhartia VK. Laparoscopic CBD exploration. Indian J Surg. 2010; 72:395–399. PMID: 21966140.

19. Jameel M, Darmas B, Baker AL. Trend towards primary closure following laparoscopic exploration of the common bile duct. Ann R Coll Surg Engl. 2008; 90:29–35. PMID: 18201497.

20. Petelin JB. Laparoscopic common bile duct exploration. Surg Endosc. 2003; 17:1705–1715. PMID: 12958681.

21. Bandyopadhyay SK, Khanna S, Sen B, et al. Antegrade common bile duct (CBD) stenting after laparoscopic CBD exploration. J Minim Access Surg. 2007; 3:19–25. PMID: 20668614.
22. Ha JP, Tang CN, Siu WT, et al. Primary closure versus T-tube drainage after laparoscopic choledochotomy for common bile duct stones. Hepatogastroenterology. 2004; 51:1605–1608. PMID: 15532787.
23. Zhang LD, Bie P, Chen P, et al. Primary duct closure versus T-tube drainage following laparoscopic choledochotomy. Zhonghua Wai Ke Za Zhi. 2004; 42:520–523. PMID: 15196362.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download