Abstract
Backgrounds/Aims
With development of imaging techniques, pancreatic tumors are being diagnosed more frequently. Applying the standard surgical procedures for pancreatic head tumors, such as pancreaticoduodenectomy and pylorus-preserving pancreaticoduodenectomy may seem too extensive for benign or low-grade malignant pancreas head tumors. Duodenum-preserving pancreatic head resection (DPPHR) has been safely performed in patients with chronic pancreatitis. Recently, DPPHR has been used as a limited surgical procedure to remove benign or low-grade malignant pancreatic head lesions. This study is aimed to evaluate the results of DPPHR in benign or low-grade malignant tumors.
Methods
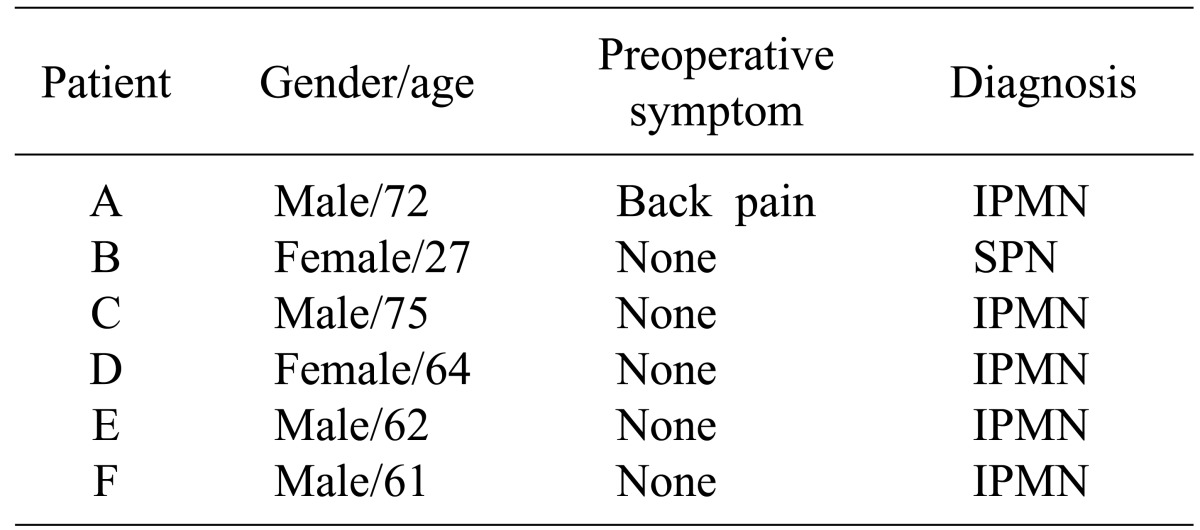
Between 2004 and 2012, six patients underwent DPPHR due to benign or low-grade malignant pancreas tumor. We performed this retrospective analysis based on the medical records.
Results
Five of six patients were diagnosed as intraductal papillary mucinous neoplasms. Remaining one patient was diagnosed as solid pseudopapillary neoplasm. The median age of patients was 60.3 (27-75) years, and the median follow-up period was 24 months. The operation time, blood loss and length of stay were 442.5 minutes, 680 ml and 19.2 days, respectively. There was no mortality. Five patients experienced complications including 1 delayed gastric empting, 2 bile duct strictures, 1 pancreatic fistula and 1 duodenal stricture. No recurrence or metastasis was found during follow-up.
Subclinical pancreas cystic tumors are being found more frequently recently, owing to the development and widespread use of new imaging techniques.1 Pancreas cystic tumor consists of serous cysteadenoma, mucinous cystic neoplasm, intraductal papillary mucinous neoplasm and solid pseudopapillary neoplasm. Each tumor shows distinct biological features and malignant potential. However, it is difficult to distinguish the benign from malignant lesions preoperatively. It is a challenge to decide on a surgical treatment due to morbidity and mortality following the surgery.2,3
In particular, pancreaticoduodenectomy and pylorus-preserving pancreaticoduodenectomy have been traditionally performed on pancreatic head lesions. With the development of surgical techniques, the operations have shown low complication and mortality rates as compared to the past. However, it is inevitable that the pancreas and nearby organs lose some of their functions. To this end, various organ-preserving pancreatic resections have been researched to resolve the issues. The representative method for pancreatic head lesions is duodenum-preserving pancreatic head resection (DPPHR). DPPHR in pancreatic tumor was first introduced by Beger for chronic pancreatitis patients.4 The application has expanded to chronic pancreatitis, precancerous lesions and pancreatic head tumors with low malignance.5
We performed this study to investigate the efficacies of duodenum-preserving pancreatic head resection for cystic neoplasm of the pancreatic head by analyzing postoperative outcomes.
The number of patients who underwent DPPHR in pancreatic tumor at Yonsei University Severance Hospital (Seoul, Korea) between October 2004 and March 2012 was eight. Among them, six patients underwent operation due to benign or low malignant pancreatic tumor. The retrospective analysis was based on the medical records.
The total number of patients who received DPPHR in pancreatic head tumor was six. The average age of patients was 60.3 (27-75) years old, and there were 4 male and 2 female patients. One patient was symptomatic and the remaining five patients were discovered incidentally by imaging studies (Table 1).
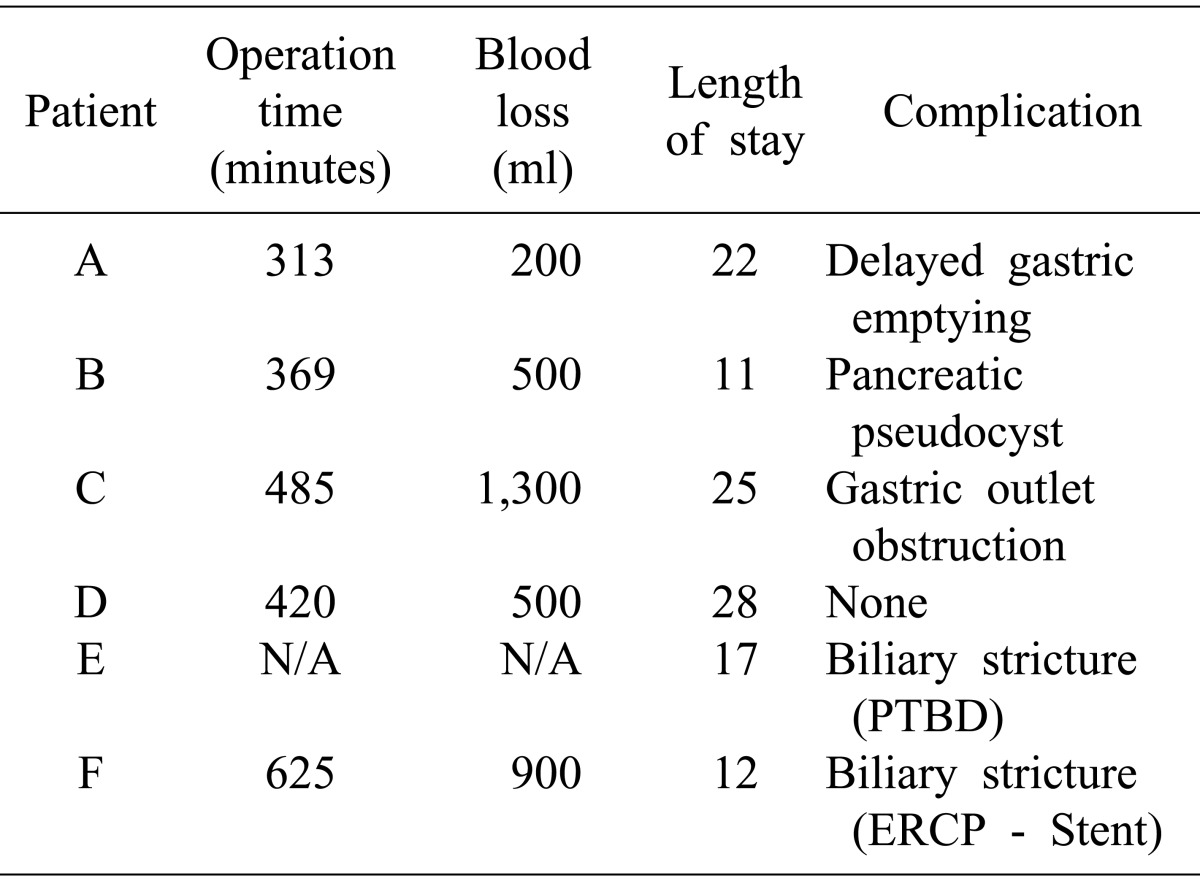
The average operation time, blood loss and length of stay were 442.5 minutes, 680 ml and 19.2 days, respectively. Combined organ resection was performed for one patient. The patient underwent DPPHR with right radical nephrectomy due to renal cell carcinoma (Table 2).
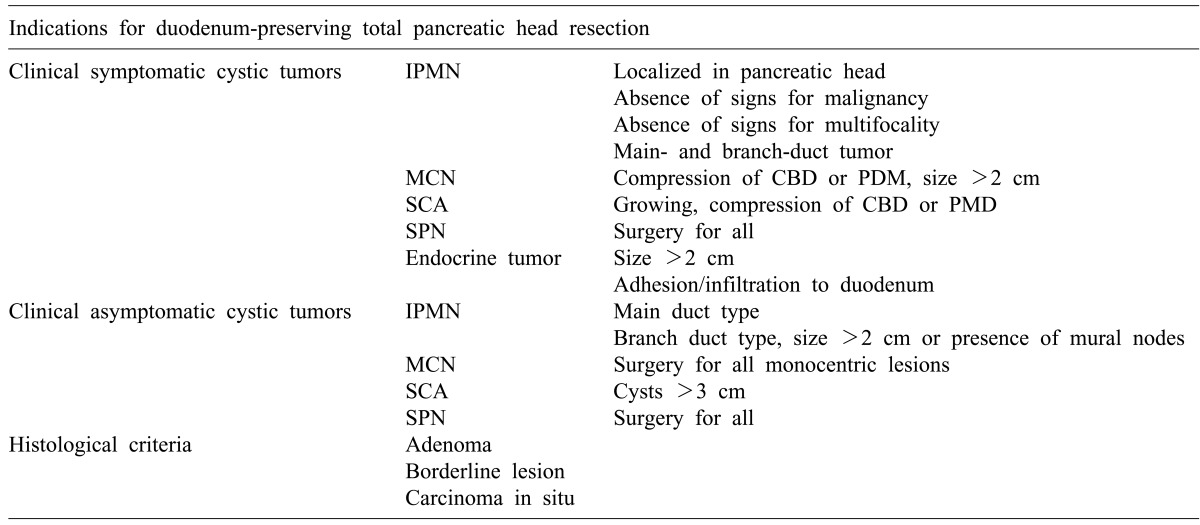
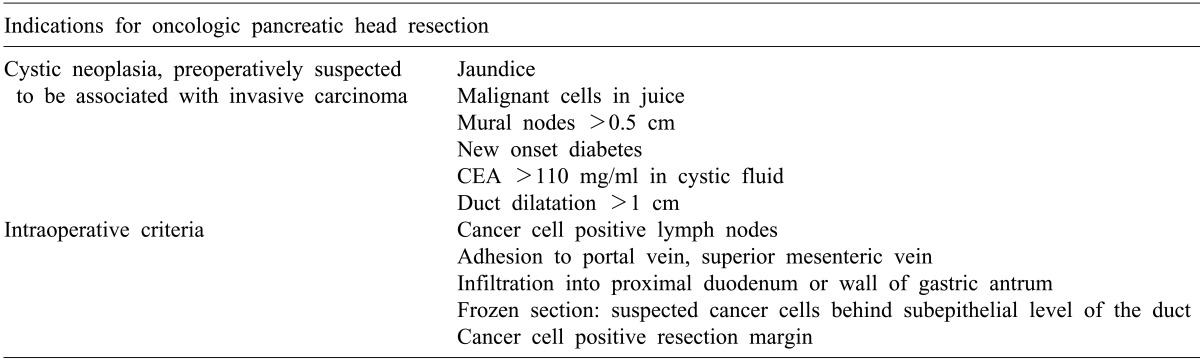
The histopathologic examination showed that 5 of 6 cases were the intraductal papillary mucinous neoplasms and the remaining one case was solid pseudopapillary neoplasm. No lymph node metastases were found among intraductal papillary mucinous neoplasms from the histopathologic examinations. Solid pseudopapillary neoplasm showed less than 5% of cytologic atypia and atypical mitosis, and β-catenin was positive to nuclear pattern from the immunohistochemical examination (Fig. 1).
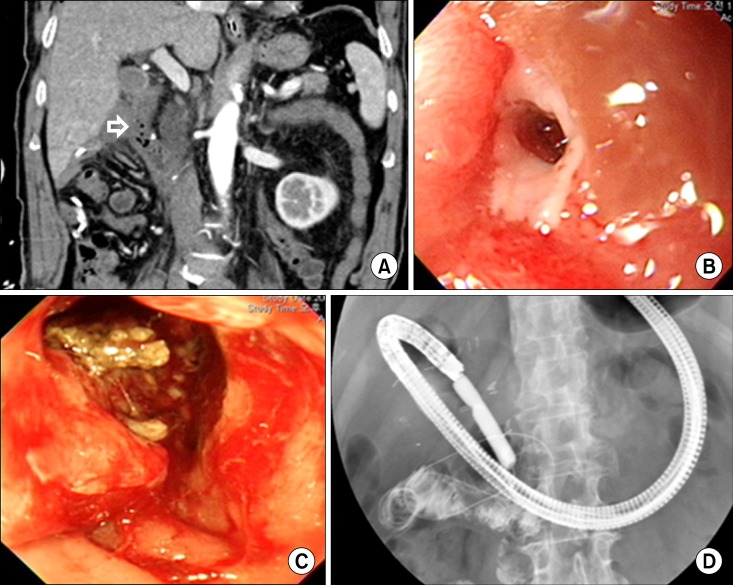
There was no mortality, and five patients showed complications including 1 delayed gastric stricture. The delayed gastric empting was improved by conservative treatment. A pancreatic fistula was found in one patient post-operation due to solid pseudopapillary neoplasm-formed cyst and was treated by cysto-pancreatic double-sided pigtail insert by the endoscopic approach. Bile duct strictures were found in 2 patients: percutaneous transhepatic biliary drainage (PTBD) was performed for one patient; and endoscopic retrograde biliary drainage was performed for the other patient. One patient suffered from repetitive duodenal ulcer due to ischemia. He experienced frequent vomiting from duodenal stricture caused by ulcer. To relieve obstructive symptoms, we conducted endoscopic balloon dilatation, only to be unsuccessful. Finally, we performed gastrojejunostomy (Fig. 2).
No recurrence of pancreatic lesions was found on the clinical shadow tracking. Average observation period was 24 months.
The advantage of DPPHR compared to traditional pancreaticoduodenectomy and pylorus-preserving pancreaticoduodenectomy is the preservation of duodenum, which has a key role in the digestive and absorptive functions. In addition, preservation of more pancreatic tissues and normal biliary tree makes it possible to improve the patient's quality of life.6,7 The most significant reason for duodenum resection with pancreas head is the danger of duodenal ischemia.
Duodenum receives arterial blood from the pancreaticoduodenal artery, which originates from the gastroduodenal artery and superior mesenteric artery. It forms an arcade, contacting duodenum at the front and pancreas head at the rear. Beger preserved thin pancreatic layers with arcade blood vessels near the internal duodenum to preserve duodenum and they resected pancreas head of chronic pancreatitis patients. Beger's technique has been modified in various forms, including a complete resection of pancreas head and preservation of duodenal blood vessels. It has been reported that a resection of pancreas head, bile duct inside the pancreas and the arcade have been performed while maintaining the blood supply from a small artery on the abdominal walls of the duodenum.8 Takada et al.9,10 designed a technique by completely resecting the pancreas head and preserving posterior arcade Miyakawa et al.11 published a technique which preserved the anterior arcade.
We performed gastrojejunostomy for one patient due to repetitive ulcer and stricture from duodenal ischemia. Extra caution needs to be taken with duodenal stricture, because DPPHR in pancreatic tumor completely resects pancreatic tissues inside the duodenum to secure the boundary surface from the center for pancreatic cystic disease. Multi-detector computed tomography may be considered to check the bloodstream around duodenum before the surgery.12
Issues including duodenal ischemia, proper operation indication and securing oncologic radicality are other concerns when applying DPPHR to pancreatic head tumor.
Frequent pancreatic cystic tumors include intraductal papillary mucinous neoplasm, mucinous cystic neoplasm, serous cystadenoma, and solid pseudopapillary neoplasm. Indication for DPPHR is a tumor placed on the pancreas head with clinical symptoms. The operative indications shall be judged as depending on the size and features of each lesion and connection with the pancreatic duct, if there are no clinical symptoms. There needs also be no evidence of malignancy or multifocality (Table 3).13,14 Clinical aspects suspicious malignance include jaundice, new diabetes, pancreatic duct expansion (>1 cm), increasing carcinoembryonic antigen (CEA) in cystic fluids and existence of mural node. Clinical opinions with strong suspicion of malignance shall be considered for pancreaticoduodenectomy or pylorus-preserving pancreaticoduodenectomy (Table 4).13
Lastly, oncologic radicality is important in applying DPPHR in precancerous lesions and malignant cystic diseases. Frozen section examination shall be applied in the operation room to secure the sufficient resection margin to prevent recurrence of the precancerous lesion and existence of malignant lesion. Additional resection is required on the resection margin if borderline atypia, pancreatic intraepithelial neoplasm (PanIN 3) is found.13
In conclusion, DPPHR in pancreas head tumor with precancerous lesions and low malignance may be replaced with a typical operation. It is required to secure a sufficient resection margin by utilizing the frozen section examination and checking for indications thorough preoperative examination. The operation must be performed by experienced surgeons due to the possibility of damaging the bile duct and causing duodenal ischemia.
References
1. Klöppel G, Kosmahl M. Cystic lesions and neoplasms of the pancreas. The features are becoming clearer. Pancreatology. 2001; 1:648–655. PMID: 12120249.
2. Ferrone CR, Correa-Gallego C, Warshaw AL, et al. Current trends in pancreatic cystic neoplasms. Arch Surg. 2009; 144:448–454. PMID: 19451487.

3. Salvia R, Malleo G, Marchegiani G, et al. Pancreatic resections for cystic neoplasms: from the surgeon's presumption to the pathologist's reality. Surgery. 2012; 152(3 Suppl 1):S135–S142. PMID: 22766364.

4. Beger HG, Krautzberger W, Bittner R, et al. Duodenum-preserving resection of the head of the pancreas in patients with severe chronic pancreatitis. Surgery. 1985; 97:467–473. PMID: 3983823.
5. Beger HG, Gansauge F, Siech M, et al. Duodenum-preserving total pancreatic head resection for cystic neoplastic lesions in the head of the pancreas. J Hepatobiliary Pancreat Surg. 2008; 15:149–156. PMID: 18392707.

6. Möbius C, Max D, Uhlmann D, et al. Five-year follow-up of a prospective non-randomised study comparing duodenum-preserving pancreatic head resection with classic Whipple procedure in the treatment of chronic pancreatitis. Langenbecks Arch Surg. 2007; 392:359–364. PMID: 17375317.

7. Pedrazzoli S, Canton SA, Sperti C. Duodenum-preserving versus pylorus-preserving pancreatic head resection for benign and premalignant lesions. J Hepatobiliary Pancreat Sci. 2011; 18:94–102. PMID: 20694480.

8. Takada T, Yasuda H, Amano H, et al. A duodenum-preserving and bile duct-preserving total pancreatic head resection with associated pancreatic duct-to-duct anastomosis. J Gastrointest Surg. 2004; 8:220–224. PMID: 15036200.

9. Takada T, Yasuda H, Amano H, et al. A duodenum-preserving and bile duct-preserving total pancreatic head resection with associated pancreatic duct-to-duct anastomosis. J Gastrointest Surg. 2004; 8:220–224. PMID: 15036200.

10. Takada T, Yasuda H, Uchiyama K, et al. Duodenum-preserving pancreatoduodenostomy. A new technique for complete excision of the head of the pancreas with preservation of biliary and alimentary integrity. Hepatogastroenterology. 1993; 40:356–359. PMID: 8406305.
11. Miyakawa S, Horiguchi A, Mizuno K, et al. Preservation of arterial arcades during duodenum-preserving total pancreatic head resection for intraductal papillary tumor. Hepatogastroenterology. 2003; 50:993–997. PMID: 12845965.
12. Horiguchi A, Miyakawa S, Ishihara S, et al. Surgical design and outcome of duodenum-preserving pancreatic head resection for benign or low-grade malignant tumors. J Hepatobiliary Pancreat Sci. 2010; 17:792–797. PMID: 19894017.

13. Beger HG, Rau BM, Gansauge F, et al. Duodenum-preserving total pancreatic head resection for cystic neoplasm: a limited but cancer-preventive procedure. Langenbecks Arch Surg. 2008; 393:589–598. PMID: 18379818.
14. Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management ofintraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006; 6:17–32. PMID: 16327281.
Fig. 1
A case of solid pseudopapillary neoplasm. (A) A 10 cm-sized, septated, cystic mass in the pancreas head. (B) Duodenum, distal common bile duct and posterior inferior pancreaticoduodenal artery (PDA) were preserved during the duodenum-preserving pancreatic head resection. (C) Atypical mitosis; Tripolar mitosis (arrow) (H-E, ×400). (D) β-catenin was found to be positive for nuclear pattern (×400).
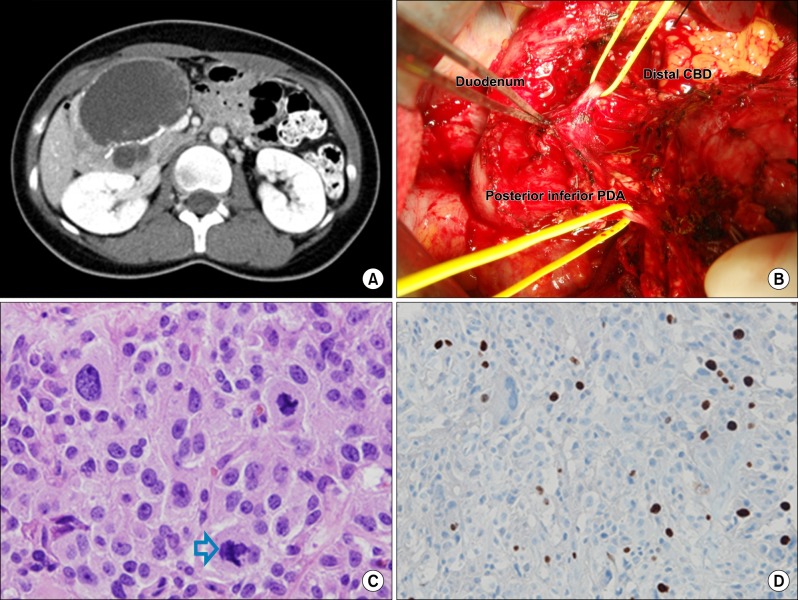
Fig. 2
Complications presenting duodenal stricture. (A) Ischemic change at the duodenal 2nd portion (arrow). (B) Huge ulcero-infiltrative lesion at duodenum. (C) Duodenal stricture. (D) Pneumatic balloon dilatation of the duodenum.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download