Abstract
Backgrounds/Aims
Mid bile duct cancers often involve the proximal intrapancreatic bile duct, and resection of the extrahepatic bile duct (EHBD) can result in a tumor-positive distal resection margin (RM). We attempted a customized surgical procedure to obtain a tumor-free distal RM during EHBD resection, so that R0 resection can be achieved without performing pancreaticoduodenectomy through extended EHBD resection.
Methods
We previously reported the surgical procedures of extended EHBD resection, in which the intrapancreatic duct excavation resembles a ≥2 cm-long funnel. This unique procedure was performed in 11 cases of mid bile duct cancer occurring in elderly patients between the ages of 70 and 83 years.
Results
The tumor involved the intrapancreatic duct in all cases. Deep pancreatic excavation per se required about 30-60 minutes. Cancer-free hepatic duct RM was obtained in 10 patients. Prolonged leakage of pancreatic juice occurred in 2 patients, but all were controlled with supportive care. Adjuvant therapies were primarily applied to RM-positive or lymph node-positive patients. Their 1-year and 3-year survival rates were 90.9% and 60.6%, respectively.
Go to : 
Cancers originating from the mid portions of the common bile duct show a variable extent of longitudinal tumor spread, often displaying a wider extent than the preoperative imaging study findings suggest. In patients with proximal-to-mid bile duct cancers, conventional resection of the extrahepatic bile duct has often resulted in tumor involvement at the proximal or distal longitudinal resection margin (RM). When the distal remnant bile duct RM is involved, pancreaticoduodenectomy is often suggested when there is intent for curative resection. However, the operative risks following pancreaticoduodenectomy are not negligible in patients with high operative risks such as elderly patients with major co-morbidities. Therefore, it is reasonable to perform pancreaticoduodenectomy only after careful assessment of the risk-benefit balance.
When the distal bile duct RM is tumor-positive, palliative resection of the bile duct as an R1 resection is occasionally performed, especially in patients with high operative risks or whose prognosis is expected to be poor due to advanced extent of the tumor such as is seen in radial bile duct RM involvement or wide lymph node metastasis. Microscopic tumor involvement of the bile duct RM frequently results in tumor recurrence.1,2
It seems essential to develop a customized surgical procedure to obtain a tumor-free distal bile duct RM during extrahepatic BD resection, through which R0 resection can be achieved without performing pancreaticoduodenectomy. We have previously presented the technique of extended extrahepatic bile duct (EHBD) resection to demonstrate its surgical feasibility.3 During an extension of the study period, we performed this surgical procedure in 11 cases. We herein present our experience with special attention to its technical feasibility and ability to achieve cure.
Go to : 
From February 2006 to December 2009, 11 patients with mid bile duct cancer underwent EHBD resection performed by one surgeon (SH).
In practice, informed consent and permission for both pancreaticoduodenectomy and EHBD resection were obtained from most of the patients with mid bile duct cancers during the study period. During the operation, the type of resection (pancreaticoduodenectomy, EHBD resection or palliative bile duct resection) was determined after complete evaluation of the tumor extent including assessment by preoperative imaging studies, intraoperative gross specimen findings and frozen-section biopsies. For patients showing tumor involvement of the distal bile duct RM after initial resection, pancreaticoduodenectomy was the treatment of choice if the general condition of the patient permitted. When the patient was elderly (>70 years) or had major co-morbidity or advanced tumor showing extensive lymph node metastasis, EHBD resection was preferentially selected instead of palliative bile duct resection. Through this process of patient selection, 11 patients finally underwent EHBD resection with curative intent.
Following surgery, multi-detector computed tomography was performed after 1 and 2 weeks as a screening test for surgical complications. These patients were followed up every 2 or 3 months at the outpatient clinic.
The surgical procedures of EHBD resection were previously described in detail.3 EHBD resection was performed based on the usual surgical procedure, but the hilar bile duct was first transected to assess the status of the proximal bile duct RM. After extensive mobilization of the duodenum from the upper part of the head of the pancreas, the pancreatic parenchyma was tangentially excised bit by bit after numerous meticulous ligations to prevent pancreatic leakage and bleeding. The longitudinal running course of the main pancreatic duct was directly identified during surgery.
When the outer surface of the proximal intrapancreatic bile duct was exposed, the depth of the pancreatic excavation was adjusted according to the location of the main tumor. If the distal intrapancreatic bile duct appeared to be tapered and had a normal appearance and there was no microscopic involvement of tumor cells on frozen-section biopsy, the intrapancreatic bile duct stump was securely repaired. In the case of RM involvement, a critical decision was made as to whether further bile duct excision should be performed or conversion to pancreaticoduodenectomy should be made.
To prevent potential leakage from the excavated pancreatic surface within the head of the pancreas, the dimpled portion was securely sutured with non-absorbable monofilaments and then two abdominal drains were placed crossing this area. In addition, a portion of the greater omentum was mobilized to cover the dissected space if possible, in order to manage potential pancreatic leakage.4
Go to : 
Ten of these 11 patients were diagnosed with mid or proximal bile duct cancer and one cancer of the cystic duct was suspected but the patient was finally diagnosed with bile duct cancer. Their mean age was 75.8±5.2 years (range: 70-83) and male patients were 9.
Deep excavation of the intrapancreatic bile duct portion per se required 20-60 minutes, and the learning curve of this part took relatively less time. Initial frozen-section biopsy of the distal bile duct RM showed tumor positivity in 2 cases and high-grade dysplasia in 1 and adenoma in 1, but the results of repeated biopsies after further resection were tumor-free in 9, tumor-positive in 1, and adenoma in 1.
Prolonged leakage of the pancreatic juice from the excavated pancreas occurred in 2 patients, but all were controlled with supportive care. In these patients, the concentrations of amylase and lipase in the abdominal drainage fluid were greater than 5,000 IU/L for the first 7 days after surgery, but their amount and enzyme levels were gradually decreased within 2-3 weeks. No patient underwent radiologic intervention to manage abnormal fluid collection around the hepatoduodenal ligament.
Adjuvant therapies after surgery were applied to RM-positive or lymph node-positive patients, including radiotherapy alone in 1 and concurrent chemoradiation therapy in 2.
Tumor recurrence occurred in 6 patients. Types of recurrence were recurrence at the hepaticojejunostomy site (n=3), abdominal lymph node metastasis (n=1), peritoneal seeding (n=1), and recurrence in the remnant intrapancreatic bile duct (n=1).
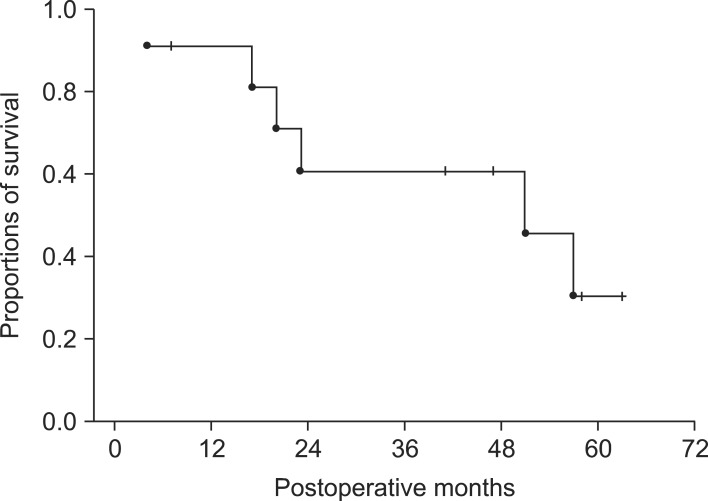
Their overall 1-year, 3-year and 5-year survival rates were 90.9%, 60.6% and 30.3%, respectively (Fig. 1).
Go to : 
Since the extent of mid bile duct cancers varies depending on the tumor growth pattern and size, extensive surgery, including pancreaticoduodenectomy and/or hepatectomy, is often necessary to achieve R0 resection. Limited curative surgery that is applied toward the liver side, known as extended hilar bile duct resection for prevention of hepatectomy, has been described before.5 Thus, this study was focused on the opposite side, facing the pancreas. The primary reason for performing EHBD resection is to reduce operative risks for patients at high risk, especially elderly individuals with co-morbidities. When considering the whole surgical procedure, pancreaticoduodenectomy or hepatectomy is a more practical and curative procedure than EHBD resection, but the latter is much less invasive, thus being safer than the former two procedures.
Following surgical treatment of bile duct cancers, the two most important prognostic factors are tumor involvement of the longitudinal and radial RMs and lymph node metastasis.6 While EHBD resection appears beneficial for obtaining a tumor-free longitudinal bile duct RM, involvement of the radial bile duct RM is another risk factor when the tumor extends to the periductal soft tissue. It has been reported that a 10-mm RM in both the proximal and distal longitudinal directions of the bile duct is required to eradicate invasive carcinoma cells, and that a 20-mm RM is required for removal of non-invasive carcinoma cells.7 Carcinoma in-situ or severe dysplasia at the bile duct RM is also associated with late local recurrence.8 For mid bile duct cancers, obtainment of a tumor-free distal bile duct RM as long as 10-20 mm is impractical without performing pancreaticoduodenectomy. Thus, the target for the longitudinal bile duct RM during EHBD resection has been adjusted to obtaining a tumor-free RM regardless of its width.
Patients with mid bile duct cancer often showed poorer prognoses than patients with hilar or distal bile duct cancer.9-12 Based on our experience, mid bile duct cancer has a poorer prognosis than distal bile duct cancer probably due to following reasons: the mid bile duct is nearer to the hepatic hilum, making it more difficult to obtain a tumor-free longitudinal bile duct RM; mid bile duct cancer cells can more easily infiltrate the hepatoduodenal ligament and extend to the serosal surface, making it more difficult to obtain a tumor-free radial bile duct RM; and the choice of surgical procedure for mid bile duct cancer has not been clearly determined, whereas pancreaticoduodenectomy is inevitable for distal bile duct cancer.13 For mid bile duct cancers with periductal infiltration and extensive lymph node metastasis, it may be difficult to improve the survival outcome through making the longitudinal bile duct RMs tumor-free, following pancreaticoduodenectomy or EHBD resection.
Conventional resection of the EHBD has often been performed to excavate some portion of the proximal intrapancreatic bile duct to increase the width of the tumor-free RM. However, such a conventional approach does not include the deep excavation of intrapancreatic bile duct dissection. Our EHBD resection can be distinguished from conventional intrapancreatic bile duct excavation since the former more aggressively attempts to obtain tumor-free longitudinal and radial RMs around the pancreas.
Deep excavation of the intrapancreatic bile duct carries a risk of damage to the pancreatobiliary union, leading to iatrogenic pancreatic duct injury. To prevent injury of this type, it is useful to explore the lumen of the intrapancreatic bile duct with a coronary dilator or other probes to estimate the depth of the remnant bile duct. Despite these precautions, iatrogenic damage of the ampulla of Vater can still occur. This situation leads to total extirpation of the entire extrahepatic bile duct. We devised a method to implant the pancreatic duct without an increase of the operative risk. This approach involves transfixing the pancreatic duct stump to the duodenal wall, placement of an internal pancreatic stent to secure drainage, and then primary repair of the duodenal wall defect after removal of the ampulla of Vater. We performed this type of pancreatic duct implantation after the study period ended and the patients recovered uneventfully and did not experience any surgical complications.
This EHBD resection is a useful procedure for resection in longitudinally advanced bile duct cancer, enabling obtainment of a tumor-free distal bile duct RM, and through which R0 resection is achievable without performing hepatopancreatoduodenectomy which carries high risks of morbidity and mortality.14,15
In conclusion, EHBD resection seems to be beneficial to obtain a tumor-free distal BD RM in proximal-to-mid bile duct cancer patients, enabling R0 resection to be achieved without performing pancreaticoduodenectomy.
Go to : 
References
1. Stein DE, Heron DE, Rosato EL, et al. Positive microscopic margins alter outcome in lymph node-negative cholangiocarcinoma when resection is combined with adjuvant radiotherapy. Am J Clin Oncol. 2005; 28:21–23. PMID: 15685030.

2. Oh D, Lim do H, Heo JS, et al. The role of adjuvant radiotherapy in microscopic tumor control after extrahepatic bile duct cancer surgery. Am J Clin Oncol. 2007; 30:21–25. PMID: 17278890.

3. Hwang S, Lee SG, Kim KH, et al. Extended extrahepatic bile duct resection to avoid performing pancreatoduodenectomy in patients with mid bile duct cancer. Dig Surg. 2008; 25:74–79. PMID: 18292664.

4. Seyama Y, Kubota K, Kobayashi T, et al. Two-staged pancreatoduodenectomy with external drainage of pancreatic juice and omental graft technique. J Am Coll Surg. 1998; 187:103–105. PMID: 9660033.

5. Shimada H, Endo I, Fujii Y, et al. Procedure of extended hilar bile duct resection and its application for hilar cholangiocarcinoma. Hepatogastroenterology. 2002; 49:300–305. PMID: 11995438.
6. Murakami Y, Uemura K, Hayashidani Y, et al. Prognostic significance of lymph node metastasis and surgical margin status for distal cholangiocarcinoma. J Surg Oncol. 2007; 95:207–212. PMID: 17278119.

7. Ebata T, Watanabe H, Ajioka Y, et al. Pathological appraisal of lines of resection for bile duct carcinoma. Br J Surg. 2002; 89:1260–1267. PMID: 12296893.

8. Wakai T, Shirai Y, Moroda T, et al. Impact of ductal resection margin status on long-term survival in patients undergoing resection for extrahepatic cholangiocarcinoma. Cancer. 2005; 103:1210–1216. PMID: 15685618.

9. Bhuiya MR, Nimura Y, Kamiya J, et al. Clinicopathologic factors influencing survival of patients with bile duct carcinoma: multivariate statistical analysis. World J Surg. 1993; 17:653–657. PMID: 8273388.

10. Nagorney DM, Donohue JH, Farnell MB, et al. Outcomes after curative resections of cholangiocarcinoma. Arch Surg. 1993; 128:871–877. PMID: 8393652.

11. Todoroki T, Kawamoto T, Koike N, et al. Treatment strategy for patients with middle and lower third bile duct cancer. Br J Surg. 2001; 88:364–370. PMID: 11260100.

12. Kayahara M, Nagakawa T, Ohta T, et al. Role of nodal involvement and the periductal soft-tissue margin in middle and distal bile duct cancer. Ann Surg. 1999; 229:76–83. PMID: 9923803.

13. Sakamoto Y, Kosuge T, Shimada K, et al. Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery. 2005; 137:396–402. PMID: 15800484.

14. Hirono S, Tani M, Kawai M, et al. Indication of hepatopancreatoduodenectomy for biliary tract cancer. World J Surg. 2006; 30:567–573. PMID: 16568228.

15. D'Angelica M, Martin RC 2nd, Jarnagin WR, et al. Major hepatectomy with simultaneous pancreatectomy for advanced hepatobiliary cancer. J Am Coll Surg. 2004; 198:570–576. PMID: 15051011.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download