Abstract
Benign portal vein thrombosis (PVT) is a challenging complication of an otherwise successful liver transplantation. PVT is caused by various conditions and results in pathologic hemodynamics of hepatofugal diversion of porto-mesenteric blood flow. Thus, adequate restoration of portal blood flow to the liver graft is a major concern when trying to achieve successful liver transplantation in patients with PVT. This letter describes the surgical view point of PVT in liver transplantation.
Go to : 
The presence of portal vein thrombosis is considered to be one of the risk factors that make liver transplantation in liver cirrhosis patients difficult. Portal vein thrombosis not only leads to markedly increased collateral vessels that may result in excessive hemorrhaging during surgery, but also, it leads to technical problems such as inadequate post-operative establishment of blood flow to the portal vein. Only 30 years ago, the Pittsburgh liver transplantation center considered portal vein thrombosis to be an absolute contraindication for liver transplantation.1 In 1985, Shaw et al.,2 for the first time resected the portal vein including the thrombosis portion in a liver cirrhosis patient, followed by interposition of a graft with an allograft vessel, thus establishing the portal circulation and leading to a successful liver transplantation. Recent advances in medical technology have permitted accurate preoperative evaluation of patients with portal vein thrombosis and collateral vessels, safe anesthesia, and most of all, advances in many and various surgical techniques that lead to feasible liver transplantation protocols. This has significantly increased liver transplantation success rates. Thus, portal vein thrombosis is no longer considered to be a contraindication in patients undergoing liver transplantation.
Risk factors for portal vein thrombosis reported to date include age, cryptogenic liver cirrhosis of unknown etiology, Laennec's liver cirrhosis, autoimmune hepatitis, hypercoaguable states, while the duration and severity of liver cirrhosis is considered to be the most important factor predicting the occurrence of portal vein thrombosis.345 According to numerous studies to date, the incidence of portal vein thrombosis in liver transplantation patients has varied markedly, from 2.1% to 26%,36789 and this variability is thought to be due to the different transplantation selection criteria between institutions, or even between groups within the same center, and to different time periods. According to the literature before 2000, the 1 year survival rate for liver transplantation in patients with portal vein thrombosis varied between 58% and 88%, and the post-operative hospital mortality rate varied from 11% to 42%.4101112 These numbers are very poor when compared to patients without portal vein thrombosis, and are attributed to incomplete removal of the thrombus, leading to portal vein thrombosis (3~28.5%) and subsequent liver failure. Other reasons for poor survival are the pre-operative chronically ill state of liver cirrhosis patients accompanied by portal vein thrombosis compared to those without portal vein thrombosis. A recent study reported significantly enhanced liver transplantation rates accompanied by portal vein thrombosis, which is due to developments and improvements in pre- and postoperative patient care and surgical technology.1314 However, mortality rates remain high, and there still exists a need for careful patient selection and meticulous surgical techniques.15
There are many variations within the portal vein thrombosis classification and cases also differ from center to center, but the Yerdel classification is the most widely employed.8 Yerdel et al. divided portal vein thrombosis into 4 grades according to the degree and location of the lesion. Grades 1 and 2 include no invasion or minimal invasion of the origin of the superior mesenteric vein, with Grade 1 being defined as portal vein thrombosis of less than 50% of the internal diameter of the blood vessel, and Grade 2 as thrombosis more than 50%. Grade 3 is defined as cases where the blood vessel is completely obstructed by the portal vein thrombosis ad there is invasion of the origin of the superior mesenteric vein. Grade 4 is disease that has progressed further than Grade 3 with involvement of the distal superior mesenteric vein. The anatomical classification of portal vein thrombosis proposed by Yerdel et al. helps in planning surgery for portal vein thrombosis. According to the previous literature, approximately 90% of portal vein thrombosis cases are resolved by thrombectomy during liver transplantation. Several reports have suggested efficacious methods of thrombectomy: simple thrombectomy or balloon thrombectomy employing a Forgaty catheter for relatively acute thrombosis, where the thrombosis is not organized with the portal vein endothelium.16 In patients with chronic liver cirrhosis accompanied by portal vein thrombosis, where the thrombosis is organized with the portal vein endothelium, the above treatment may be difficult to implement. In the latter group of patients, an alternative is eversion thrombectomy whereby the organized portal vein endothelium is separated by everting extravascularly, or by performing a longitudinal incision on one side of the portal vein and removing the thrombosis followed by surgical closure (incisional thrombectomy).1718 An incisional thrombectomy is closed by inserting a patch longitudinally in between the incision. This also resolves, simultaneously, portal vein atrophy deformations that result from chronic portal vein thrombosis. Complete removal of the thrombosis during thrombectomy should be attained since anastomosis of the graft liver portal vein and recipient portal vein is to be performed. After thrombectomy, an increase in the portal blood flow must be confirmed.
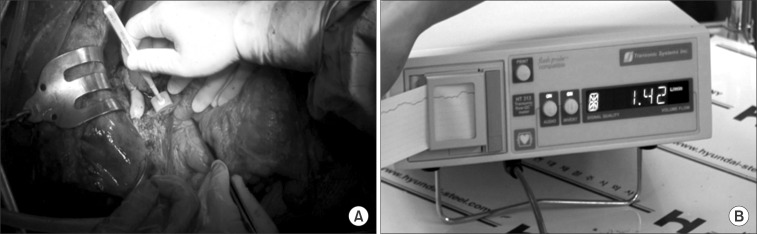
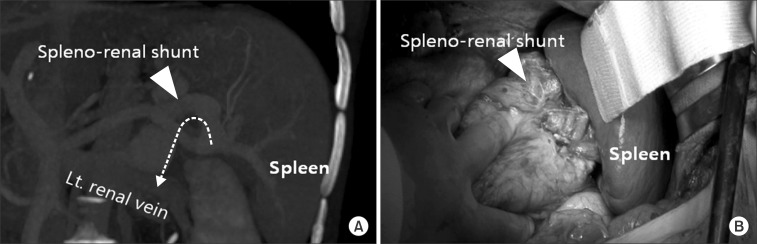
In our institution, confirmation of portal blood flow after thrombectomy is done by grossly observing an adequate degree of bleeding from the portal vein, and by employing a Doppler flowmeter to check that at least 1 L/min of portal blood flow reperfusion is present in the grafted portal vein (Fig. 1). In patients with a complete thrombosis that occludes the portal vein, the portal collateral vessels are highly developed in the portal circulation. Therefore, even though the portal thrombosis is removed, the developed portal flow is diverted to the collateral vessels, sometimes resulting in Portal Steal syndrome. Therefore, checking that portal blood flow after portal reperfusion of the graft liver is adequate is an important step in the liver transplantation procedure. Additional ligation of the collateral vessels may be necessary during surgery. In the majority of cases, collateral vessels form between the spleen and the left renal vein, and may necessitate a splenectomy that will completely and effectively block the collateral circulation of the portal vein and systemic circulation (Fig. 2).
For patients who are Yerdel classification Grade 3 and for whom thrombectomy of the portal vein is not feasible, and where there is cavernous change or atrophy and stenosis of the portal vein, an interposition vessel graft between the superior mesenteric vein and the portal vein utilizing cryopreserved allograft vessels is necessary. The ideal location of the graft vessel is between the gastroduodenal transition portion and the pancreas.8 For patients who are Yerdel classification Grade 4, the superior mesenteric vein cannot be utilized to sustain the graft liver portal blood supply. The only option is using the collateral vessels of the portal vein. Reports to date have described interposition of cryopreserved or autologous vessels between graft portal vein and left renal vein is effective when spleno-renal shunt is present.19 However, in patients in whom the splenic vein-left renal vein collateral vessels are not developed, the surgical procedure described above may become complex. These patients display development of the coronary vein collateral vessels, and although anastomosis of the coronary vein and portal vein has been studied, difficulties have been encountered since the vessel wall of the of coronary vein collateral vein is too thin for anastomosis with the portal vein.8 Although very rarely employed, a radical cavoportal hemitransposition technique that anastomoses the inferior vena cava to the grafted liver portal vein has been reported.2021 But this method does not correct the abnormal portal circulation of the recipient, and the patient will be subjected to continuous post-operative portal hypertension. Therefore, unless there is absence of any other alternative, the above technique is not recommended.
In conclusion, due to advances in medical and technological fields, liver transplantation may be provided to patients with portal vein thrombosis. This can now produce favorable outcomes. For successful liver transplantation in the above group of patients, not only are meticulous surgical techniques required, but also, careful and precise pre-operative evaluation of the degree of thrombosis and understanding of the patient's collateral circulation are essential. Each individual patient with liver cirrhosis that is accompanied by portal vein thrombosis should be uniquely characterized with respect to the pattern of thrombosis and portal collateral veins. Therefore, for successful outcomes, adequate establishment of portal circulation and the type of surgical method to be implemented are topics that need to be addressed by the liver transplantation surgeon.
References
1. Van Thiel DH, Schade RR, Starzl TE, et al. Liver transplantation in adults. Hepatology. 1982; 2:637–640. PMID: 6749636.

2. Shaw BW Jr, Iwatsuki S, Bron K, Starzl TE. Portal vein grafts in hepatic transplantation. Surg Gynecol Obstet. 1985; 161:66–68. PMID: 3892734.
3. Molmenti EP, Roodhouse TW, Molmenti H, et al. Thrombendvenectomy for organized portal vein thrombosis at the time of liver transplantation. Ann Surg. 2002; 235:292–296. PMID: 11807371.

4. Davidson BR, Gibson M, Dick R, Burroughs A, Rolles K. Incidence, risk factors, management, and outcome of portal vein abnormalities at orthotopic liver transplantation. Transplantation. 1994; 57:1174–1177. PMID: 8178342.

5. Sobhonslidsuk A, Reddy KR. Portal vein thrombosis: a concise review. Am J Gastroenterol. 2002; 97:535–541. PMID: 11922544.

6. Stieber AC, Zetti G, Todo S, et al. The spectrum of portal vein thrombosis in liver transplantation. Ann Surg. 1991; 213:199–206. PMID: 1998400.

7. Seu P, Shackleton CR, Shaked A, et al. Improved results of liver transplantation in patients with portal vein thrombosis. Arch Surg. 1996; 131:840–844. PMID: 8712907.

8. Yerdel MA, Gunson B, Mirza D, et al. Portal vein thrombosis in adults undergoing liver transplantation: risk factors, screening, management, and outcome. Transplantation. 2000; 69:1873–1881. PMID: 10830225.
9. Manzanet G, Sanjuán F, Orbis P, et al. Liver transplantation in patients with portal vein thrombosis. Liver Transpl. 2001; 7:125–131. PMID: 11172396.

10. Gayowski TJ, Marino IR, Doyle HR, et al. A high incidence of native portal vein thrombosis in veterans undergoing liver transplantation. J Surg Res. 1996; 60:333–338. PMID: 8598664.

11. Cherqui D, Duvoux C, Rahmouni A, et al. Orthotopic liver transplantation in the presence of partial or total portal vein thrombosis: problems in diagnosis and management. World J Surg. 1993; 17:669–674. PMID: 8273391.

12. Moreno González E, García García I, Gómez Sanz R, González-Pinto I, Loinaz Segurola C, Jiménez Romero C. Liver transplantation in patients with thrombosis of the portal, splenic or superior mesenteric vein. Br J Surg. 1993; 80:81–85. PMID: 8428302.

13. Ravaioli M, Zanello M, Grazi GL, et al. Portal vein thrombosis and liver transplantation: evolution during 10 years of experience at the University of Bologna. Ann Surg. 2011; 253:378–384. PMID: 21183851.
14. Kim SJ, Kim DG, Park JH, et al. Clinical analysis of living donor liver transplantation in patients with portal vein thrombosis. Clin Transplant. 2011; 25:111–118. PMID: 20184630.

15. Englesbe MJ, Schaubel DE, Cai S, Guidinger MK, Merion RM. Portal vein thrombosis and liver transplant survival benefit. Liver Transpl. 2010; 16:999–1005. PMID: 20677291.

16. Kadry Z, Selzner N, Handschin A, Müllhaupt B, Renner EL, Clavien PA. Living donor liver transplantation in patients with portal vein thrombosis: a survey and review of technical issues. Transplantation. 2002; 74:696–701. PMID: 12352888.

17. Dumortier J, Czyglik O, Poncet G, et al. Eversion thrombectomy for portal vein thrombosis during liver transplantation. Am J Transplant. 2002; 2:934–938. PMID: 12482145.

18. Egawa H, Tanaka K, Kasahara M, et al. Single center experience of 39 patients with preoperative portal vein thrombosis among 404 adult living donor liver transplantations. Liver Transpl. 2006; 12:1512–1518. PMID: 17004256.

19. Marubashi S, Dono K, Nagano H, et al. Living-donor liver transplantation with renoportal anastomosis for patients with large spontaneous splenorenal shunts. Transplantation. 2005; 80:1671–1675. PMID: 16378059.

20. Tzakis AG, Kirkegaard P, Pinna AD, et al. Liver transplantation with cavoportal hemitransposition in the presence of diffuse portal vein thrombosis. Transplantation. 1998; 65:619–624. PMID: 9521194.

21. Yan P, Yan LN. Cavoportal hemitransposition in liver transplantation: a new technique. Hepatobiliary Pancreat Dis Int. 2003; 2:202–205. PMID: 14599969.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download