Abstract
Backgrounds/Aims
The rates of surgery-related complications during and after pancreaticoduodenectomy (PD) remain very high, reaching up to 41%. They were primarily caused by leakage of pancreatic juice. We evaluated the effectiveness of external drainage of the bile duct using a pigtail drain to prevent pancreatic leakage in patients undergoing PD.
Methods
We evaluated 79 patients who underwent PD using a single-layer continuous suture between the pancreatic parenchyma and jejunum after duct-to-mucosa anastomosis by a single surgeon from April 2005 to December 2008. Of the 79, 44 underwent external drainage (ED) of the bile duct using a pigtail drain, performed in the intraoperative field via a retrograde transhepatic approach, whereas 35 did not undergo ED.
Results
Age, sex distribution, number of total complications, pancreatic duct size, pancreatic texture and duration of hospital stay did not differ between patients who did and did not undergo ED. In groups with or without ED, 0 and 4 patients, respectively, showed leakage of pancreatic juice and the difference was statistically significant (p=0.02).
Conclusions
The fact that none of the patients who underwent external drainage experienced pancreatic leakage, suggests that external drainage of the bile duct with a pigtail drain to decompress the jejunum and to drain pancreatic and bile juice is useful in preventing the complications of pancreatic leakage.
Go to : 
Pancreaticoduodenectomy (PD) is a standard surgical procedure for benign and malignant diseases of the pancreatic head and periampullary region. The first successful resection of a periampullary cancer was described in 1898,1 and the first successful PD, a two-stage procedure for ampullary cancer, was reported in 1912 by Kausch. The Whipple operation, a two-stage procedure for carcinoma of the ampulla of Vater, first described in 1935 by Whipple et al.,2 became a standard surgical method, and has been modified by many surgeons, but the mortality rate of patients undergoing PD has been as high as 30%, decreasing to about 25% in the decade from 1960 to 1970.1 Due to improvements in surgical technique and perioperative patient care, the mortality rate in patients undergoing PD has declined to <5% in many institutions around the world.13456 But the surgery-related complication rate remains at about 40-50%.137891011 Leakage of pancreatic juice at the pancreatoenteric anastomosis remains a major complication of PD.1121314 Pancreaticojejunostomy is frequently performed to manage complications related to a remnant pancreas. We have evaluated the effectiveness of external drainage (ED) of the bile duct using a pigtail drain to prevent leakage of pancreatic juice in patients undergoing PD.
Go to : 
We evaluated 79 consecutive patients who underwent PD using a single-layer continuous suture between the pancreatic parenchyma and jejunum after duct-to-mucosa anastomosis,15 performed by a single surgeon between April 2005 and December 2008. Of these 44 underwent ED of the bile duct using a pigtail drain, performed in the intraoperative field via a retrograde transhepatic approach; 35 did not undergo ED. Pancreatic leakage was defined as drainage of 50 ml of amylase-rich (>10,000 U/L) and pus-like fluid with symptoms on or after 7-10 days postoperatively.
We performed mirrored L-shaped skin incision laparotomies, along with the Kocher maneuver. Resection of the pancreatic head, including the duodenum, the first 15 cm of the jejunum, the common bile duct and the gall bladder, was performed using the standard methods. In addition, the lymph nodes of the hepatoduodenal ligament, celiac trunk and the right side of the superior mesenteric artery were totally excised. The pancreas was cut with Metzenbaum scissors, and bleeding was controlled by electrocauterization or suture ligation. The cut proximal jejunum was lifted through the mesentery of the transverse colon to the right side of the superior mesenteric vessel. A hole corresponding to the size of the pancreatic duct in the jejunum was made by the needle tip of the electrocautery device, and a single-layer continuous suture was loosely made between the posterior side of the pancreatic parenchyma and the posterior side of the hole on the jejunum. A duct-to-mucosa anastomosis using interrupted sutures was made on the lateral, superior and inferior parts. A stent was inserted into the pancreatic duct and fixed to maintain its inner strength. The opposite end of this stent was placed about 5 cm distal to the choledochojejunostomy (CJ) site to avoid direct contact of the pancreatic juice with the anastomosis site. Both threads of the single layer continuous suture on both sides were pulled to attach the pancreatic parenchyma and jejunum. One thread was fixed and the other thread was used to make a single layer continuous suture between the anterior side of the pancreatic parenchyma and the jejunum. These surgical procedures have been described in detail elsewhere.15
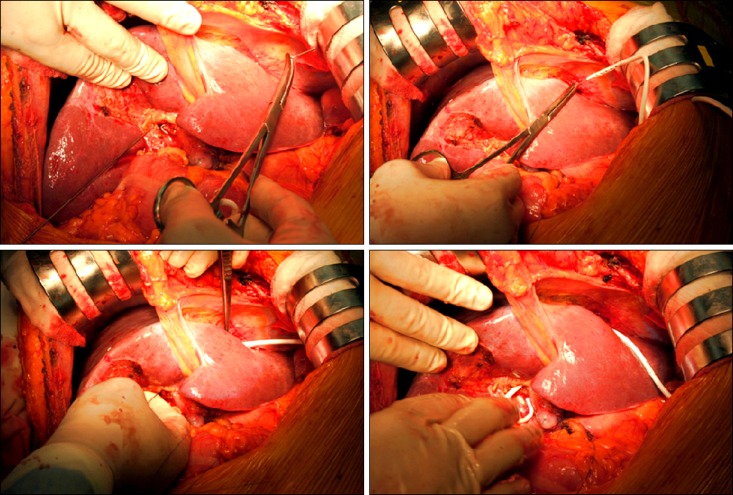
ED of the bile duct using a pigtail drain was performed in the intraoperative field via a retrograde transhepatic approach. A pigtail catheter was pulled through the opening of the bile duct and the liver parenchyma, to the anterior abdominal wall (Fig. 1). After duodenojejunal anastomosis, fibrin glue was applied to the anastomotic sites. A nasogastric tube was inserted into the afferent loop from the nasal end to about 90 cm. Finally, 4 closed-suction drain tubes were inserted through the lesser sac, and the abdomen was closed.
Continuous data are presented as mean±SD unless indicated otherwise. Pre-, intra- and post-operative laboratory data were compared between ED and non-ED groups using the Mann-Whitney U test for continuous variables and Fisher's exact test for categorical variables. SPSS version 12.0 (SPSS Inc., Chicago, IL) was used for all statistical analyses. A p-value less than 0.05 was considered statistically significant.
Go to : 
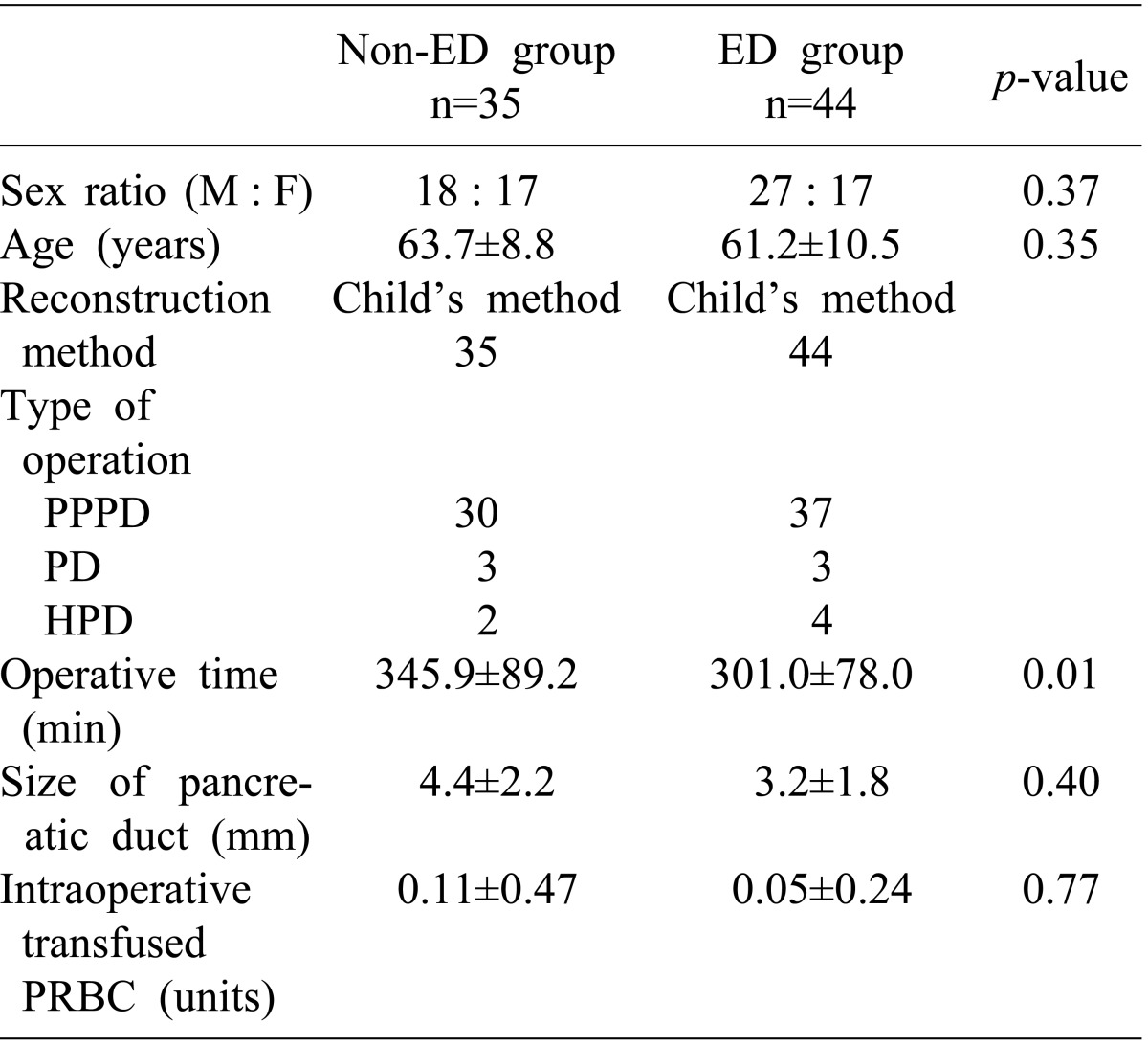
Of the 79 patients, 44 underwent ED of the bile duct using a pigtail drain and 35 did not undergo ED. The non-ED group consisted of 18 males and 17 females, whereas the ED group consisted of 27 males and 17 females (p=0.37). The mean ages of these two groups were 63.7±8.8 years and 61.2±10.5 years (p=0.35). Of the 79 patients, 67 (30 in the non-ED and 37 in the ED group) underwent pylorus-preserving pancreaticoduodenectomy (PPPD), 6 (3 in each group) underwent pancreaticoduodenectomy (PD) and 6 (2 in the non-ED and 4 in the ED) underwent hepatopancreaticoduodenectomy (HPD). Following duct-to-mucosa anastomosis, the anastomosis between the remnant pancreas and the jejunum in all 79 patients consisted of a single layer continuous suture between the pancreatic parenchyma and the jejunum. Mean operative time was significantly longer in the non-ED than in the ED group (345.9±89.2 min vs. 301.0±78.0 min; p=0.01). The mean size of the pancreatic duct was similar in these two groups (4.4±2.2 mm vs. 3.2±1.8; p=0.40), as was the mean transfusion of packed red blood cells (0.11±0.47 units vs. 0.05±0.24 units; p=0.77) (Table 1).
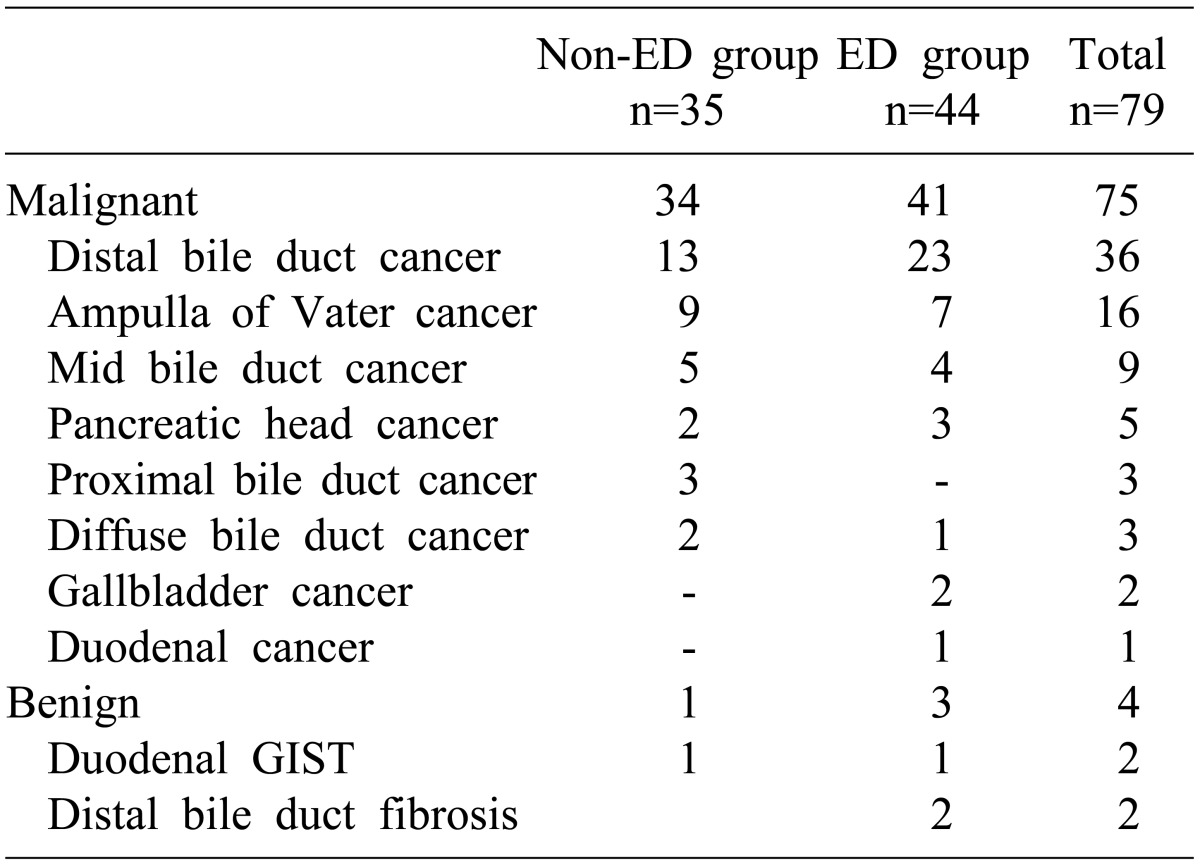
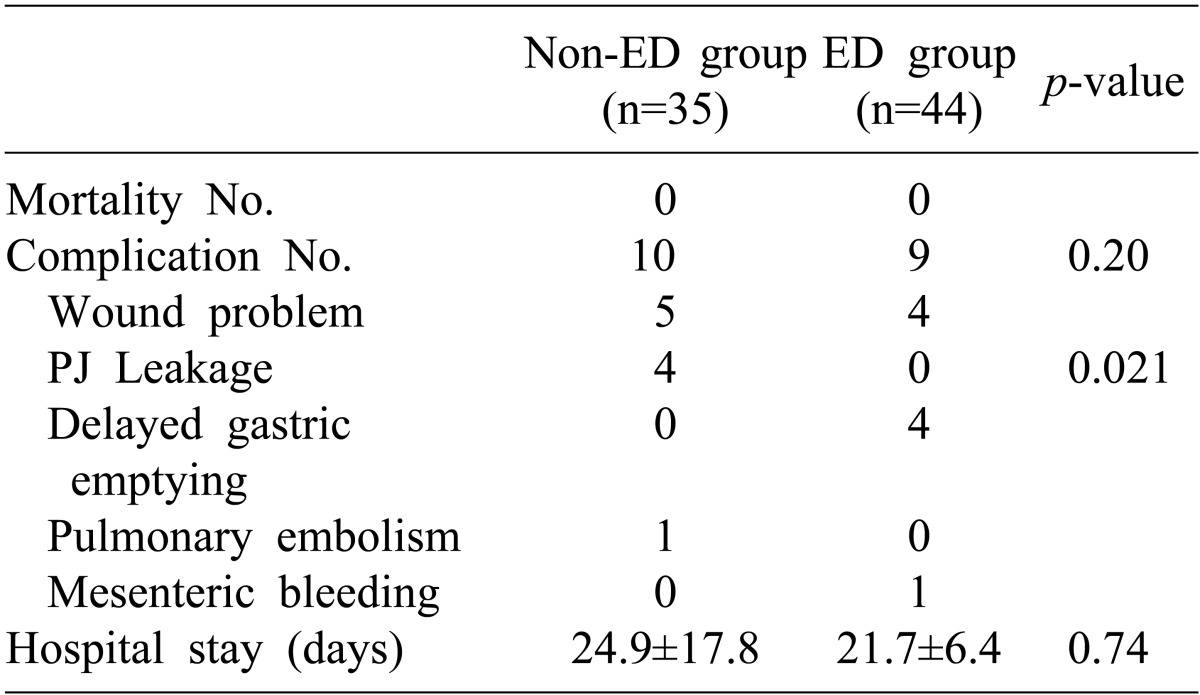
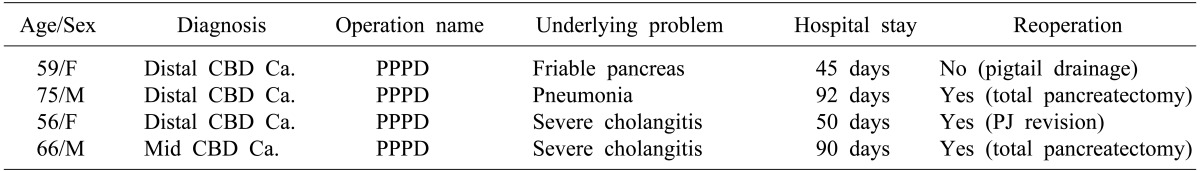
Of the 79 patients, 75 were diagnosed with malignant diseases, including 36 with distal common bile duct cancer, 16 with ampulla of Vater cancer, 9 with mid common bile duct cancer, 5 with pancreatic head cancer, 3 with proximal common bile duct cancer, 3 with diffuse common bile duct cancer, 2 with gallbladder cancer and 1 with duodenal cancer. The remaining 4 patients had benign diseases, including 2 with duodenal gastrointestinal stromal tumor and 2 with distal common bile duct fibrosis (Table 2). None of the patients died, but overall 19 patients, 10 in the non-ED and 9 in the ED group (p=0.20), experienced postoperative complications, including 9 patients with wound problems, 4 with delayed gastric emptying, 4 with pancreatic leakage, 1 with pulmonary embolism and 1 with mesenteric bleeding. Mean hospital stays were similar in the non-ED and ED groups (24.9±17.8 days vs. 21.7±6.4days; p=0.74). Four patients in the non-ED, but none in the ED group, experienced pancreatic leakage (p=0.021) (Table 3). One patient with pancreatic leakage was treated by insertion of a pigtail drain without reoperation; the other 3 required secondary surgery, including a pancreaticojejunostomy revision in 1 and total pancreatectomy in 2 (Table 4).
Go to : 
Although the mortality rate of patients undergoing PD has been as high as 20%,161718 it has recently declined to less than 5%.1371019 Yeo et al. reported that the mortality rate in 650 patients who underwent PD at a single center was 1.4%,1 whereas Gouma et al. reported that the mortality rate of PD was lower (<1%) in high-volume experienced hospitals.20 These reductions in the death rate are thought to be related to improvements in surgical and anesthetic techniques, postoperative intensive care, nutritional care and interventional radiology.6
Despite the reduction in the death rate, the rate of complications in patients undergoing PD remains high, about 41%,20 and has not decreased much over the last 30 years. Even specialized hospitals have reported pancreatic leakage rates after PD of about 20-30%. Disease-related risk factors associated with pancreatic leakage include pancreatic texture and pathology, pancreatic duct size and pancreatic juice output; patient-related risk factors include age, sex, co-morbid illnesses, and jaundice; operation-related risk factors include intraoperative blood loss, operative technique and the surgeons' experience.21222324252627282930
Pancreatic leakage is a major complication for pancreas and biliary surgeons. Among the surgical techniques used to handle the pancreas remnant are duct-to-mucosa anastomosis of pancreaticojejunostomy and external pancreatic duct stenting, both of which have been found to reduce the incidence of pancreatic leakage. In our institution, pancreaticojejunostomy is a routine reconstruction method, since pancreatic enzymes are activated and digestion and absorption occur physiologically. If a pancreatic leakage occurs, however, activation of the pancreatic enzymes may lead to an intra-abdominal abscess, sepsis and life-threatening massive bleeding.
There are no agreed on standard criteria for pancreatic leakage, as the leakage rate may be misinterpreted and comparisons are difficult. Therefore, a consensus definition of pancreatic leakage is required. The definition of pancreatic leakage we used included drainage of more than 50 ml of amylase-rich (>10,000 U/L) and pus-like fluid with symptoms (fever, abdominal pain, or leukocytosis) on or after the 7th postoperative day.31
We found no evidence of pancreatic leakage in any of our patients who underwent pigtail drain insertion via the bile duct, whereas pancreatic leakage occurred in four patients who did not undergo drainage (p=0.02). The two groups were similar in age, sex distribution, number of total complications, pancreatic duct size, pancreatic texture and duration of hospital stay, but differed in operation time. Pancreatic juice in the pancreatic duct was completely removed through a long internal stent inserted into the duct. External drainage of bile has the potential additional advantage of restricting pancreatic enzyme activation by bile juice. These two safety devices, internal drainage of pancreatic juice through a long internal stent and external drainage of bile juice by a pigtail drain, result in a more complete diversion of pancreatic juice and bile juice and inhibition of pancreatic enzyme activation by biliary secretion. In addition, external drainage of bile by a pigtail drain is effective in decompressing the jejunal loop. Postoperative inhibition of coordinated bowel activity causes secretions to accumulate in the jejunal loop, thereby increasing intraluminal pressure.
ED with a pigtail drain is not difficult to perform and does not require much time. Indeed we found that the average operation time was significantly shorter in the ED than in the non-ED group (p=0.01), suggesting that it is an easy surgical technique to be performed to prevent pancreatic leakage in high risk patients.
Although PD has been shown to reduce pancreatic leakage, there have been few prospective trials evaluating the techniques and their standardization. Our findings suggest that intra-operative external drainage of the bile duct with a pigtail drain for selected patients with risk factors for pancreatic leakage, including small pancreatic duct size, friable pancreatic parenchyma, underlying co-morbidities, or older age, may prevent the complications of pancreatic leakage.
Go to : 
References
1. Yeo CJ, Cameron JL, Sohn TA, et al. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg. 1997; 226:248–257. PMID: 9339931.
2. Whipple AO, Parsons WB, Mullins CR. Treatment of carcinoma of the ampulla of vater. Ann Surg. 1935; 102:763–779. PMID: 17856666.
3. Fernández-del Castillo C, Rattner DW, Warshaw AL. Standards for pancreatic resection in the 1990s. Arch Surg. 1995; 130:295–299. PMID: 7887797.

4. Lieberman MD, Kilburn H, Lindsey M, Brennan MF. Relation of perioperative deaths to hospital volume among patients undergoing pancreatic resection for malignancy. Ann Surg. 1995; 222:638–645. PMID: 7487211.

5. Poon RT, Fan ST, Lo CM, et al. Pancreaticoduodenectomy with en bloc portal vein resection for pancreatic carcinoma with suspected portal vein involvement. World J Surg. 2004; 28:602–608. PMID: 15366753.

6. Miedema BW, Sarr MG, van Heerden JA, Nagorney DM, McIlrath DC, Ilstrup D. Complications following pancreaticoduodenectomy. Current management. Arch Surg. 1992; 127:945–949. PMID: 1353671.
7. Poon RT, Fan ST, Chu KM, Poon JT, Wong J. Standards of pancreaticoduodenectomy in a tertiary referral centre in Hong Kong: retrospective case series. Hong Kong Med J. 2002; 8:249–254. PMID: 12167728.
8. Eyre-Brook IA. Low mortality following resection for pancreatic and periampullary tumours in 1026 patients: UK survey of specialist pancreatic units. Br J Surg. 1998; 85:425. PMID: 9529513.

9. Böttger TC, Junginger T. Factors influencing morbidity and mortality after pancreaticoduodenectomy: critical analysis of 221 resections. World J Surg. 1999; 23:164–171. PMID: 9880426.

10. Cameron JL, Pitt HA, Yeo CJ, Lillemoe KD, Kaufman HS, Coleman J. One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg. 1993; 217:430–435. PMID: 8098202.

11. Jimenez RE, Fernandez-del Castillo C, Rattner DW, Chang Y, Warshaw AL. Outcome of pancreaticoduodenectomy with pylorus preservation or with antrectomy in the treatment of chronic pancreatitis. Ann Surg. 2000; 231:293–300. PMID: 10714621.

12. Strasberg SM, Drebin JA, Soper NJ. Evolution and current status of the Whipple procedure: an update for gastroenterologists. Gastroenterology. 1997; 113:983–994. PMID: 9287993.

13. Trede M, Schwall G. The complications of pancreatectomy. Ann Surg. 1988; 207:39–47. PMID: 3276272.

14. Cullen JJ, Sarr MG, Ilstrup DM. Pancreatic anastomotic leak after pancreaticoduodenectomy: incidence, significance, and management. Am J Surg. 1994; 168:295–298. PMID: 7524375.

15. Kim KH, Lee HJ, Lee YJ, et al. Effect of a single layer continuous suture between pancreatic parenchyma and jejunum after duct-to-mucosa anastomosis in pancreaticoduodenectomy: a single surgeon's experiences. Hepatogastroenterology. 2007; 54:1368–1372. PMID: 17708256.
16. Crile G Jr. The advantages of bypass operations over radical pancreatoduodenectomy in the treatment of pancreatic carcinoma. Surg Gynecol Obstet. 1970; 130:1049–1053. PMID: 4192028.
17. Shapiro TM. Adenocarcinoma of the pancreas: a statistical analysis of biliary bypass vs Whipple resection in good risk patients. Ann Surg. 1975; 182:715–721. PMID: 1190874.
18. Herter FP, Cooperman AM, Ahlborn TN, Antinori C. Surgical experience with pancreatic and periampullary cancer. Ann Surg. 1982; 195:274–281. PMID: 6277259.

19. Trede M, Schwall G, Saeger HD. Survival after pancreatoduodenectomy. 118 consecutive resections without an operative mortality. Ann Surg. 1990; 211:447–458. PMID: 2322039.
20. Gouma DJ, van Geenen RC, van Gulik TM, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 2000; 232:786–795. PMID: 11088073.

21. Yeo CJ, Cameron JL, Maher MM, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 1995; 222:580–580. PMID: 7574936.

22. Yeo CJ, Cameron JL, Lillemoe KD, et al. Does prophylactic octreotide decrease the rates of pancreatic fistula and other complications after pancreaticoduodenectomy? Results of a prospective randomized placebo-controlled trial. Ann Surg. 2000; 232:419–429. PMID: 10973392.
23. Sato N, Yamaguchi K, Chijiiwa K, Tanaka M. Risk analysis of pancreatic fistula after pancreatic head resection. Arch Surg. 1998; 133:1094–1098. PMID: 9790207.

24. Bartoli FG, Arnone GB, Ravera G, Bachi V. Pancreatic fistula and relative mortality in malignant disease after pancreaticoduodenectomy. Review and statistical meta-analysis regarding 15 years of literature. Anticancer Res. 1991; 11:1831–1848. PMID: 1685076.
25. van Berge Henegouwen MI, De Wit LT, Van Gulik TM, Obertop H, Gouma DJ. Incidence, risk factors, and treatment of pancreatic leakage after pancreaticoduodenectomy: drainage versus resection of the pancreatic remnant. J Am Coll Surg. 1997; 185:18–24. PMID: 9208956.

26. Marcus SG, Cohen H, Ranson JH. Optimal management of the pancreatic remnant after pancreaticoduodenectomy. Ann Surg. 1995; 221:635–645. PMID: 7794068.

27. Hamanaka Y, Nishihara K, Hamasaki T, et al. Pancreatic juice output after pancreatoduodenectomy in relation to pancreatic consistency, duct size, and leakage. Surgery. 1996; 119:281–287. PMID: 8619183.

28. Ishikawa O, Ohigashi H, Imaoka S, et al. Concomitant benefit of preoperative irradiation in preventing pancreas fistula formation after pancreatoduodenectomy. Arch Surg. 1991; 126:885–889. PMID: 1854249.

29. Matsusue S, Takeda H, Nakamura Y, Nishimura S, Koizumi S. A prospective analysis of the factors influencing pancreaticojejunostomy performed using a single method, in 100 consecutive pancreaticoduodenectomies. Surg Today. 1998; 28:719–726. PMID: 9697265.

30. Yeh TS, Jan YY, Jeng LB, et al. Pancreaticojejunal anastomotic leak after pancreaticoduodenectomy--multivariate analysis of perioperative risk factors. J Surg Res. 1997; 67:119–125. PMID: 9073557.

31. Shyr YM, Su CH, Wu CW, Lui WY. Does drainage fluid amylase reflect pancreatic leakage after pancreaticoduodenectomy? World J Surg. 2003; 27:606–610. PMID: 12715232.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download