This article has been
cited by other articles in ScienceCentral.
Abstract
Laparoscopic cholecystectomy has resulted in various bile duct injuries. Treatment of these injuries is usually difficult and often leads to an intractable clinical course. We herein present a case of isolated right anterior sector (RAS) duct injury induced by laparoscopic cholecystectomy. The bile duct injury was successfully treated by hepatic atrophy induction. Imaging studies revealed that the RAS duct was severed, probably due to rare anatomical variations. Considering the difficulty in surgical reconstruction, atrophy induction of the involved hepatic parenchyma was attempted. This treatment consisted of embolization of the RAS portal branch to inhibit bile production, induction of heavy adhesion at the bile leak site to ensure percutaneous pigtail clamping, and sequential clamping and removal of pigtail catheters. This procedure took 3 months prior to pigtail catheter removal. She was free from other complications during the first 12 months and to date. She will be followed up for 5 years overall including surveillance for hepatobiliary complications. Although this therapeutic induction of atrophy approach is not universally applicable, it can be considered to be a feasible option in unique situations such as this one.
Go to :

Keywords: Laparoscopic cholecystectomy, Sectoral bile duct injury, Liver atrophy, Portal vein embolization
INTRODUCTION
Laparoscopic cholecystectomy (LC) has been long established as a surgical procedure that typically is minimally invasive. However, LC can result in various kinds of surgical complications that are not commonly associated with open cholecystectomy. Bile duct injury is the most common LC-associated complication, with an incidence of 0.5-1.4%, and it is diverse in terms of extent and location.
1234 Isolated injury of the right hepatic sectoral or segmental bile duct is an unusual form of major bile duct injury.
56 The usual causes of this injury type include direct cutting or clip clamping of the segmental duct, and thermal injury from irrelevant cauterization. Variant biliary anatomy such as a low-inserting right posterior duct and other rare variations of segmental duct union with the cystic duct are reported to be important predisposing conditions.
7 Isolated injury to the right anterior sector (RAS) following LC is very rare, compared with that of the right posterior sector duct, and its surgical treatment is difficult due to its deep location.
We herein present an unusual case of isolated injury of the RAS duct following LC. This damage might be associated with accidental transection of the duct without identifying that the bile duct was a rare anatomic variant. This variation was recognized a few days after LC. The injury was successfully treated by induction of segmental liver atrophy through segmental portal vein embolization and segmental bile duct occlusion.
89
Go to :

CASE
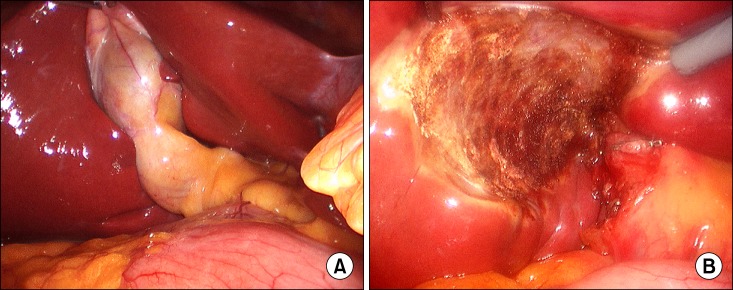
A 48 year-old female patient was transferred from another institution due to intractable bile leak after LC. It was reported that her primary diagnosis was calculous cholecystitis and all LC procedures were completed uneventfully according to standard techniques (
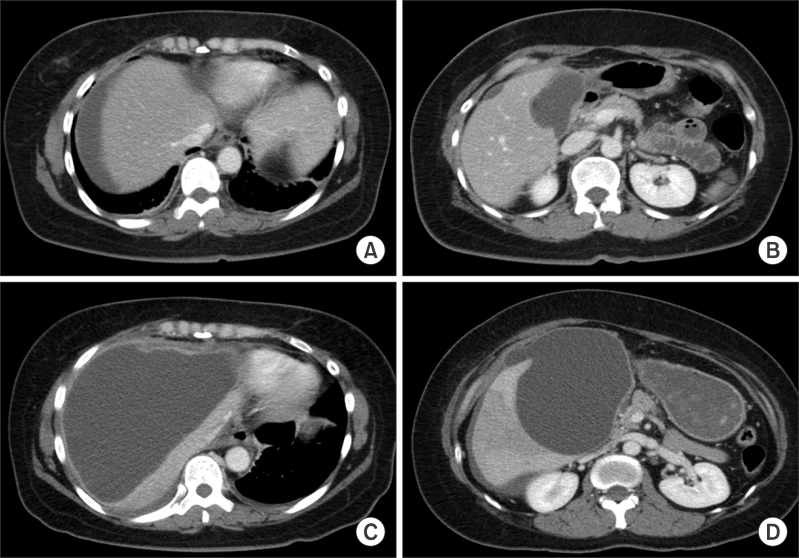
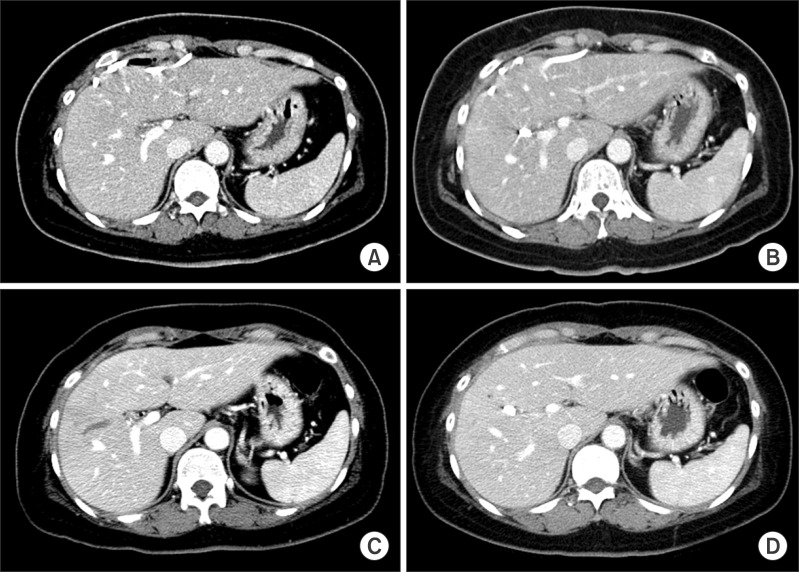
Fig. 1). The patient discharged on the second day after LC, but 4 days later she readmitted due to abdominal pain and fever. Abdomen computed tomography (CT) revealed abnormal fluid collection in the subhepatic and subphrenic areas (
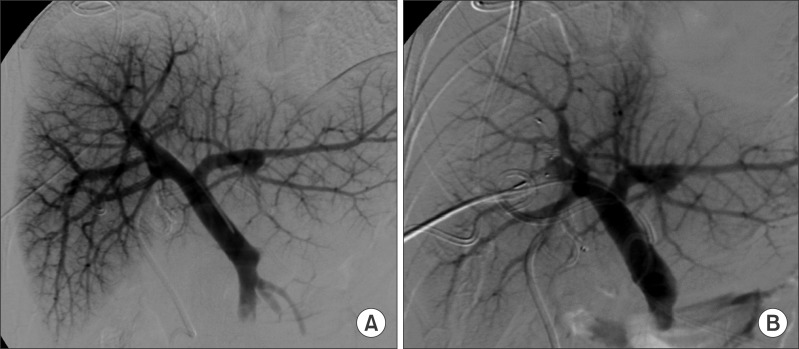
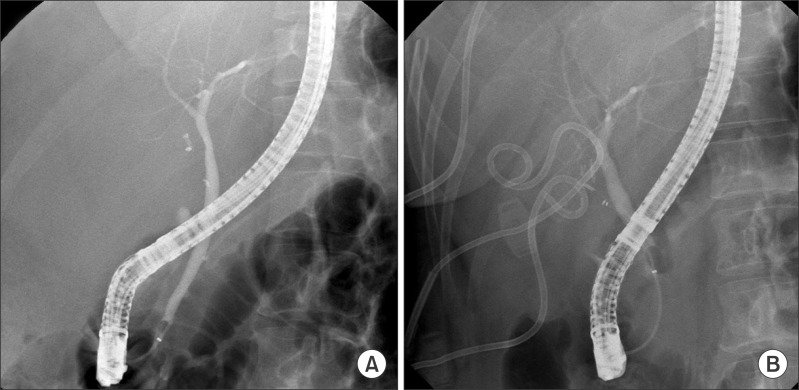
Fig. 2A, B). Endoscopic retrograde cholangiography (ERC) was performed under suspicion of bile leak, but no biliary injury was recognized at the time of the ERC procedure (
Fig. 3A). A retrospective review of the ERC images indicated that one of the right sectoral ducts was not visualized, but this finding was missed at the time of the ERC. Even after supportive care for 1 week, her symptoms had progressively become aggravated. Follow-up CT scans showed definite accumulation of a huge amount of perihepatic fluid (
Fig. 2C, D), which led to multiple pigtail insertion. The drained fluid was pure bile. A repeat ERC showed no evidence of a leak (
Fig. 3B), but pure bile of about 150 ml/day continuously drained from the abdominal pigtail catheters. Finally, she was transferred to our institution, 40 days after LC.
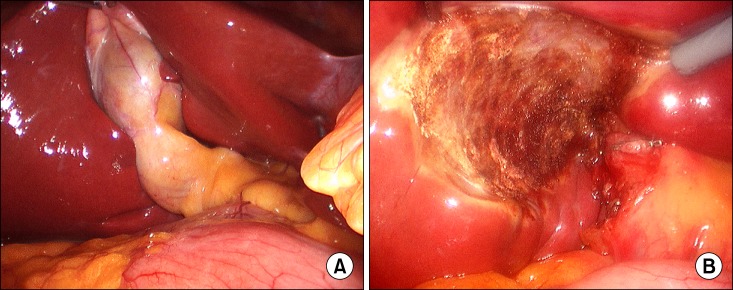 | Fig. 1Laparoscopic findings of the gallbladder (A) and gallbladder bed after cholecystectomy (B). Only the cystic duct stump was ligated except for small clips applied to the cystic artery. There was no evidence of bile leak from the dissected surface.
|
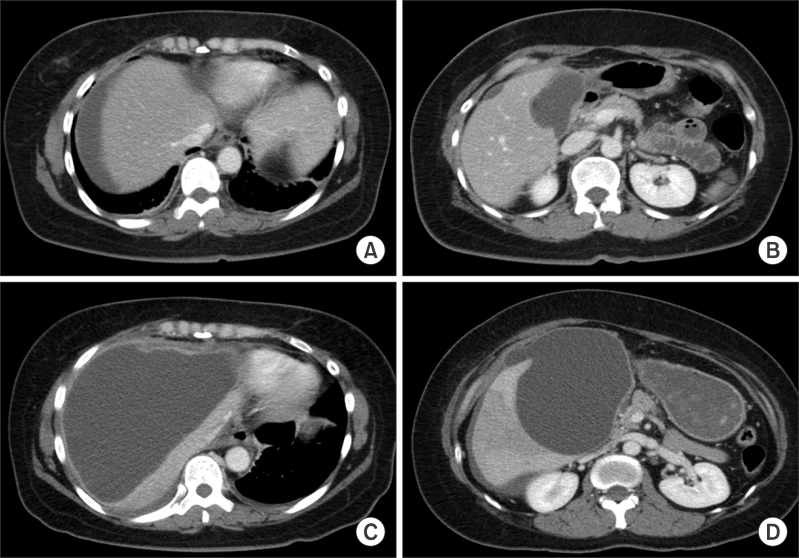 | Fig. 2Abdomen computed tomography scan showing progressive accumulation of abnormal fluid collection in the subhepatic and subphrenic areas at 1 week (A and B) and 2 weeks (C and D) after laparoscopic cholecystectomy.
|
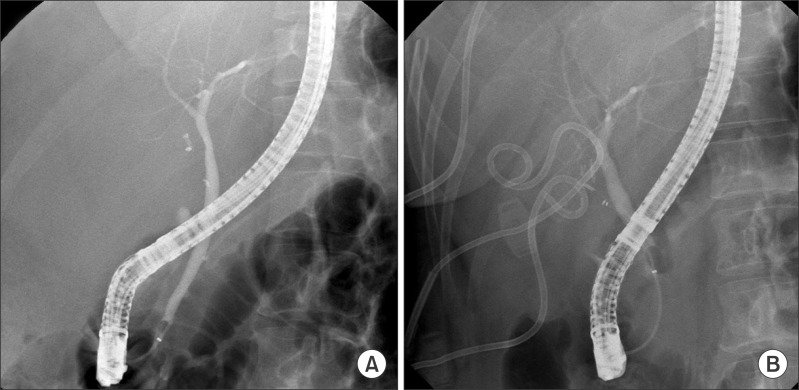 | Fig. 3Endoscopic retrograde cholangiography images showing no evidence of bile leak. Each was taken at 1 week (A) and 3 weeks (B) after laparoscopic cholecystectomy. Subhepatic pigtail catheters are shown together (B). There is an abnormal finding showing only one right sectoral duct.
|
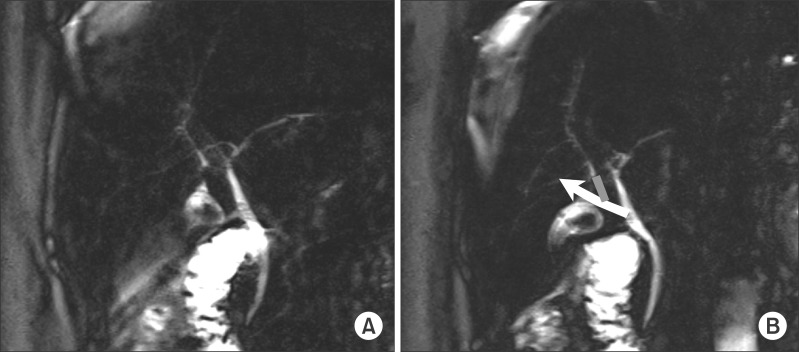
We assessed the extent of LC-associated bile duct injury. Magnetic resonance cholangiography (MRC) was carried out to delineate the biliary anatomy of the missing duct. The RAS duct had been transected close to the liver parenchyma, but there was no recognizable duct stump at the common bile duct except the cystic duct clipping (
Fig. 4A). This biliary anatomy implicates that the RAS duct might be aberrantly inserted into the cystic duct and both cystic duct and RAS duct were transected altogether (
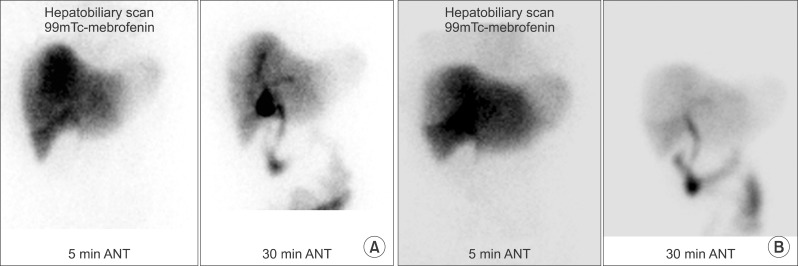
Fig. 4B). Hepatobiliary scintigraphy showed major bile leak from the gallbladder fossa (
Fig. 5A). There was no intrahepatic duct dilatation in the right liver, implicating that bile drained freely from the transected RAS duct (
Fig. 6A).
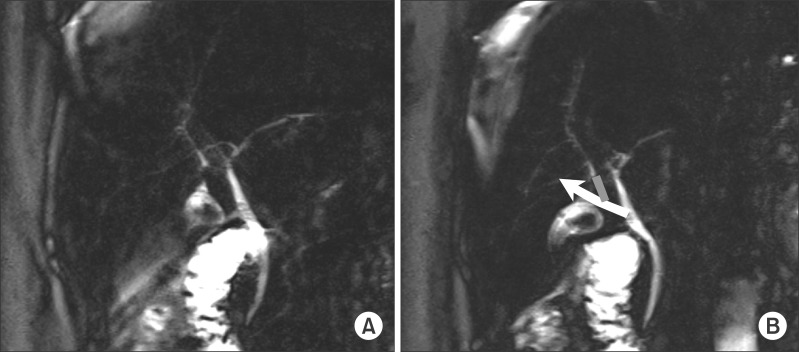 | Fig. 4Magnetic resonance cholangiography images showing the extent of bile duct injury. Bile is leaking from the right anterior sectoral duct and scattered to the subhepatic and subphrenic areas (A). The missed portion of the right anterior segmental duct (red) and its imaginary insertion into the cystic duct (green) are illustrated (B).
|
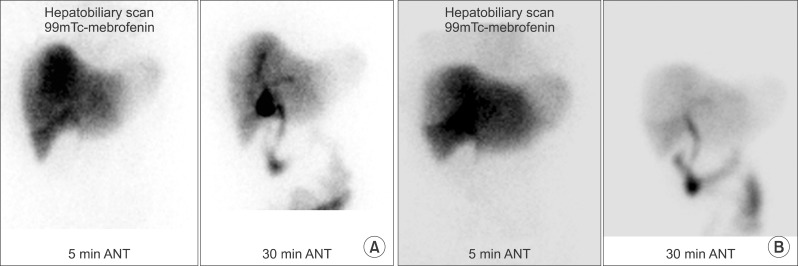 | Fig. 5Hepatobiliary scan images taken before (A) and 6 months after (B) embolization of the portal branch of the right anterior sector. The territory of the right anterior sector appears to be deficient in bile production.
|
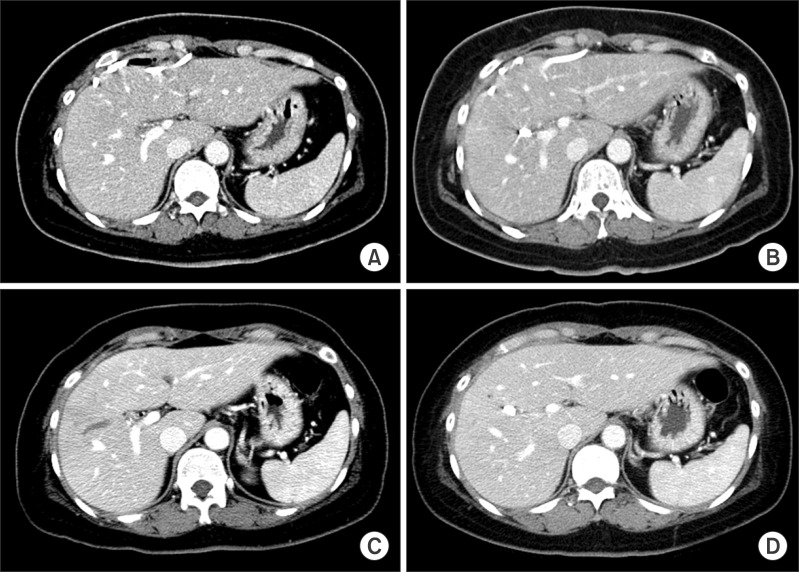 | Fig. 6Sequences of liver computed tomography scans showing progressive atrophy of the right anterior sector. The images were taking before (A), and 1 week (B), 1 month (C), and 6 months (D) after segmental portal vein embolization.
|
The morphological features of this isolated injury to the RAS duct suggested that primary reconstruction using Roux-en-Y hepaticojejunostomy was not feasible or was technically very difficult and RAS resection appeared to be very complicated. Based on our previous experience with hepatic atrophy induction therapy for LC- and hepatectomy-associated segmental bile duct injuries,
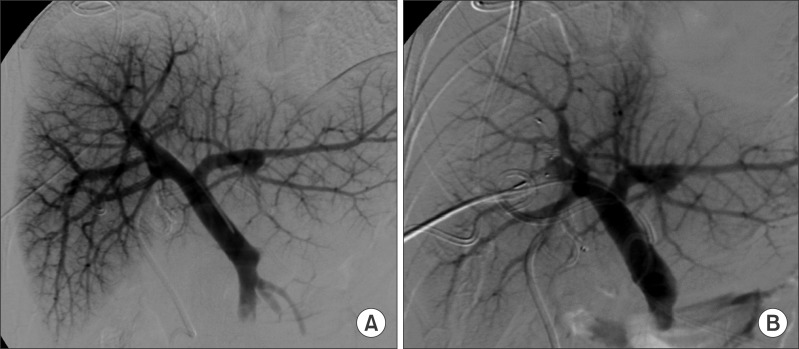
89 we decided to perform portal vein embolization (PVE) of the RAS portal branch to induce atrophy of the RAS parenchyma (
Fig. 7). Thereafter, the amount of bile drained from the pigtail diminished dramatically, and the fluid color became much paler. CT scans taken after 1 and 4 weeks showed that the RAS parenchyma had atrophied markedly (
Fig. 6B, C).
 | Fig. 7Percutaneous direct portogram images taken before (A) and after (B) embolization of the portal branch of the right anterior sector.
|
Two weeks after PVE, one subphrenic pigtail catheter was removed. Ten weeks after PVE, the amount of pigtail drainage became scanty. Thus, the single subhepatic pigtail catheter was left clamped for additional 2 weeks. Thereafter, we removed the last clamp after ensuring the occurrence of heavy adhesions around the bile leak site. The pigtail was kept in place for a total of 3 months after PVE, as initially planned. At 6 months after PVE, the RAS parenchyma was definitely atrophied (
Fig. 6D) and bile production disappeared completely on follow-up hepatobiliary scans (
Fig. 5B). She was free from any other complications during the first 12 months and to date. She will be followed up for 5 years including surveillance for hepatobiliary complications.
Go to :

DISCUSSION
Although most major bile duct injuries are detected during the LC procedure or within a few days, some biliary injuries are not recognized due to the absence of significant symptoms and signs.
10 Present case revealed bile leak as the major sign of bile duct injury. Initially this injury had not been suspected because the records of operative fields were transparently free from abnormal findings. This LC-induced RAS duct injury must be very rare because we have not encountered such an injury after about 20,000 LCs over 20 years in our institution.
ERC can result in an accidental isolated injury to the segmental bile duct.
56 The presence of bile leak despite normal-looking ERC findings is a diagnostic dilemma. Under such circumstances, MRC should be carried out as it can disclose the whole configuration of the biliary tree even after total transection of the bile duct.
1112
After a thorough review of dynamic CT, MRC, ERC and hepatobiliary scan findings, we concluded that the injury site was located deep within the hepatic hilum. As this site might be deep seated and surrounding tissues would be necrotic due to biloma, primary biliary reconstruction did not appear feasible. Removal of the bile-leaking RAS parenchyma can be considered, but it must be the last choice of treatment. Thus, non-surgical treatment should be attempted first whenever it is available.
We have reported the effectiveness and usefulness of hepatic atrophy induction treatment for isolated segmental bile duct injury following LC and central hepatectomy.
89 There are two primary mechanisms associated with hepatic parenchymal atrophy, deprivation of portal blood flow and bile duct obstruction. Methods to induce both were applied sequentially to all of our reported patients, including this case. The treatment procedure consisted of three major steps, the first being embolization of the segmental portal branch, which effectively inhibited the quantity and quality of bile production.
1314 The second step was closure of the leak site through induction of heavy adhesion to ensure clamping of the percutaneous transhepatic biliary drainage or pigtail drainage. After a series of testclampings, the abdominal drain was removed. The third step was inhibition of bile drainage through spontaneous occlusion of the segmental duct to accelerate atrophy of the segmental parenchyma. After these steps, the segmental intrahepatic duct became rather dilated, but no further dilatation was observed on follow-up imaging studies. These three-step procedures usually took 3-4 months.
In conclusion, our experience from this case and others suggests that percutaneous segmental portal vein embolization followed by intentional clamping of the external biliary drainage can effectively treat intractable bile leaks caused by segmental bile duct injury of various causes, including LC.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download