Abstract
Backgrounds/Aims
The aims of this study were to evaluate risk factors for acute cholecystitis that have been previously acknowledged and to evaluate several co-morbidities, such as hypertension, diabetes mellitus, cardiovascular disease, cerebrovascular accident and end-stage renal disease for which the prevalence rate has increased in the elderly.
Methods
We retrospectively reviewed 611 patients who underwent laparoscopic or open cholecystectomy for cholecystitis between January 2005 and January 2010. The relationships between the clinical outcomes and the clinico-demographic factors were analyzed by univariate and multivariate analyses.
Results
The diagnoses of the 611 patients who underwent laparoscopic cholecystectomy were acute cholecystitis (n=258; 42.2%) and chronic cholecystitis (n=353; 57.8%). Male gender (p<0.000), age >50 (p<0.000), fever (p<0.000), leukocytosis (p<0.000), AST elevation (p=0.009), alkaline phosphatase elevation (p<0.000) and an elevation of total bilirubin (p<0.000) were identified as risk factors for acute cholecystitis. The presence of diabetes mellitus (p=0.002) and hypertension (p=0.019) may be risk factors for acute cholecystitis.
Go to : 
Acute cholecystitis is one common cause of acute abdomen. It is associated with moderate to high severity due to its clinical potential to develop pyogenic cholecystitis, which may result in gallbladder necrosis, perforation, abscess or even peritonitis. In the elderly, the severity of acute cholecystitis increases immensely; thus, it is crucial to determine proper treatment times and methods. Despite its clinical significance, however, we still lack knowledge of predisposing factors and co-morbidities that may influence disease development and progression. Commonly known risk factors have been found mostly in epidemiologic studies, the reliability of which has often been questioned because different results were shown in different studies.
This study was designed to re-evaluate several known risk factors for cholecystitis, such as age, sex, and obesity. Furthermore, we investigated whether chronic diseases, including hypertension, diabetes mellitus, cardiovascular disease, cerebrovascular accident, or end-stage renal disease, are risk factors for developing acute onset cholecystitis.
Go to : 
We retrospectively reviewed 611 patients who underwent laparoscopic or open cholecystectomy for cholecystitis between January 2005 and January 2010.
A clinical diagnosis of cholecystitis was made by a combination of clinical data, including demographics, symptoms, laboratory data, radiographic findings, and peri-operative information. The demographic factors included sex, age, height and weight. Based on these, body mass index was also calculated. Hypertension, diabetes mellitus, cardiovascular disease, cerebrovascular accident, end stage renal disease, liver cirrhosis and medication history related to neuropsychiatric problems were co-morbidities that were documented. Cardiovascular diseases included all main categories of coronary disease (stable angina, unstable angina, myocardial infarction). Cerebrovascular accidents included both cerebral hemorrhage and infarction. Neuropsychiatric problems included depression and bipolar disease, schizophrenia and Parkinson's disease. Symptomatic factors included fever with a body temperature higher than 37.5℃ and right upper quadrant abdominal pain with tenderness or positive for Murphy's sign. Because the physical examination was performed by many different emergency room doctors, inaccuracy could be a confounding factor, so the physical exam was not considered. Available laboratory values were collected for the cohort, including white blood cell count, aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), total bilirubin, amylase, total cholesterol, and triglyceride levels. In cases with diabetes, the HbA1c level was also checked. Elevated laboratory values were converted to nominal variables and analyzed using chi-square test. Reference points for elevations were as follows: WBC ≥10.00×103/ul, AST/ALT ≥40 IU/L, total bilirubin ≥1.2 mg/dl, ALP ≥250 IU/L, amylase ≥125 U/L, total cholesterol ≥230 mg/dl, triglyceride ≥200 mg/dl, HbA1c ≥6.4%/total Hb. Radiographic factors included any ultrasound or computed tomography (CT) images, such as gallbladder wall thickening, increased blood flow around the gallbladder or pericholecystic fluid collection. But these findings were also excluded for the same reason as the physical examination. Peri-operative findings consisted of morphological changes of the gallbladder wall, adhesion to an adjacent organ, distortion of the biliary anatomy, gross inflammation of the gallbladder serosa, and gallstone characteristics. All subjective findings were used for grouping, but not for statistical analysis. Only gallstone characteristics were used for analysis. Gallstone characteristics included presence of stone, type of stone and number of stones. The types of stones were sorted by the surgeon who described the cutting edge of the stone after the operation. Stones were sorted into three subgroups: cholesterol stones, black pigmented stones, and brown pigmented stones. The cholesterol stone was grossly round or angular shaped, and had a smooth surface and a yellow color. The black pigmented stone was grossly irregular and hard, and had a black or dark green color. The brown pigmented stone had a brownish color or a small and clayey character.1 Through integration of these information, patients with cholecystitis were separated into two subgroups, those with acute cholecystitis and those with chronic cholecystitis.
Laparoscopic cholecystectomy was performed as a first-line treatment for most of the patients with cholecystitis. Some had to undergo open cholecystectomy due to adhesions, bleeding or the possibility of bile duct injury. The operation was performed by the same surgical team using the standard 3- or 4-port technique. Laparoscopic cholecystectomy was electively performed in patients with chronic cholecystitis, and cholecystectomy was performed as soon as possible for the patients with acute cholecystitis during their initial hospital admission.
The histology of the gallbladder was confirmed by pathology report after the operation and the result was compared with previously set up clinical classifications. Using chi-square test, the correlation between the pathologic and the clinical classifications was analyzed. With a value of the κ index of 0.413 (p<0.000), the pathologic and the clinical classification have a verification of statistical likelihood.
Exclusion criteria were as follows: Patients who underwent major liver resection done for hepatocellular carcinoma or intrahepatic duct stone were excluded. We excluded patients who underwent radical cholecystectomy due to gallbladder malignancy. Patients who underwent gastrectomy for whatever reason were also excluded.
The relationships between the clinical outcomes and patient demographic factors and the co-morbidities and laboratory data were analyzed by performing univariate and multivariate analyses. Commercially available programs (release 19.0; SPSS Inc, Chicago, Illinois) were used to analyze the data. We assessed statistical significance using chi-square test. Tests were conducted for all variables in the patient cohort. For convenience, continuous variables were converted to nominal variables for analysis. A p-value less than 0.05 indicated statistical significance. Variables with statistical significance were then used in a multivariate logistic regression model.
Go to : 
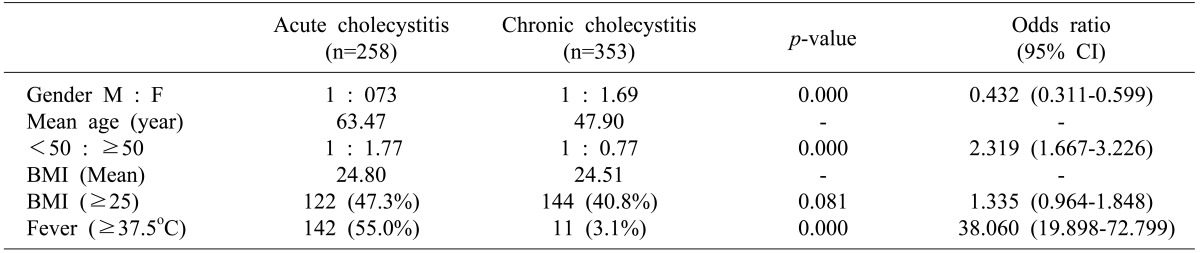
Diagnoses of the 611 patients who underwent cholecystectomy were acute cholecystitis (n=258; 42.2%), chronic cholecystitis (n=353; 57.8%). Patient characteristics in acute and chronic cholecystitis are compared in Table 1. There were 280 men (45.8%) and 331 women (54.2%). Sex ratios were 1 : 0.73 and 1 : 1.69, respectively, for the groups with acute and chronic cholecystitis (p<0.000). The mean ages for the two groups were 63 and 48, respectively. Patients with acute cholecystitis were older than those with chronic cholecystitis. We found statistically significant differences (p<0.000) in age distributions divided by the age of 50 years between the patients with acute and chronic cholecystitis. Among the 611 patients, the average height and weight were 162.9 cm (range: 132-188) and 65.4 kg (range: 32-113). We calculated the body mass index (BMI) and, using a BMI value of 25 as the controlling point, we found no statistically significant differences (p=0.081) between the two groups. Of the 258 patients that presented with acute cholecystitis, 142 (55%) presented with fever >37.5℃ compared with the patients with chronic cholecystitis (p<0.000).
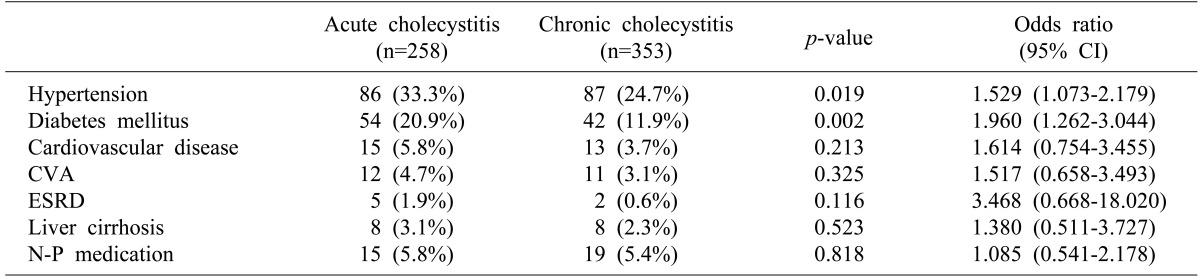
All patients were assessed for the presence of the seven co-morbidities listed in Table 2. The number of co-morbidities and their statistical significance are shown in Table 2. Among the 611 patients, 243 (39.8%) had one or more co-morbidities and hypertension was present in 173 (28.3%). Univariate analysis identified hypertension (p=0.019) and diabetes (p=0.002) as having a significant association with acute cholecystitis.
Analysis using laboratory values is reported in Table 3. Leukocytosis (p<0.000), an elevation of AST (p=0.009), an elevation of ALP (p<0.000) and an elevation of total bilirubin (p<0.000) were significantly different. AST was not significantly different than ALT.
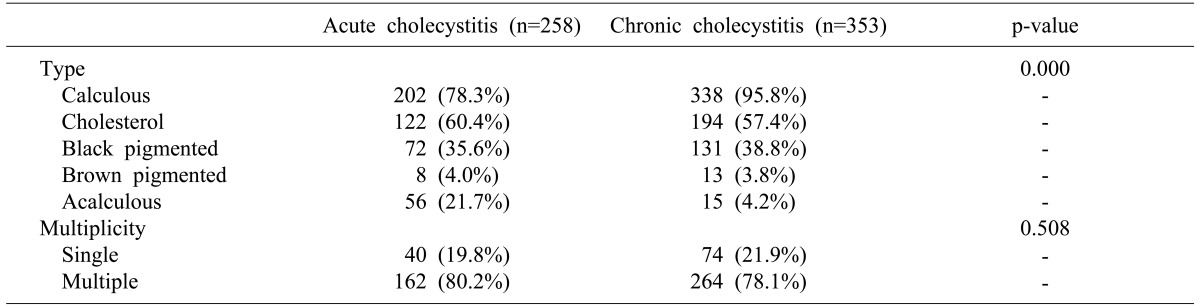
The characteristics of gallstones are summarized in Table 4. As confirmed by the surgical reports, 71 (11.6%) patients presented with acalculous cholecystitis. Among the acute cholecystitis group, 56 (21.7%) patients were treated for acalculous cholecystitis. Through a univariate analysis, the absence of gallstone was significant; the number of gallstones was not.
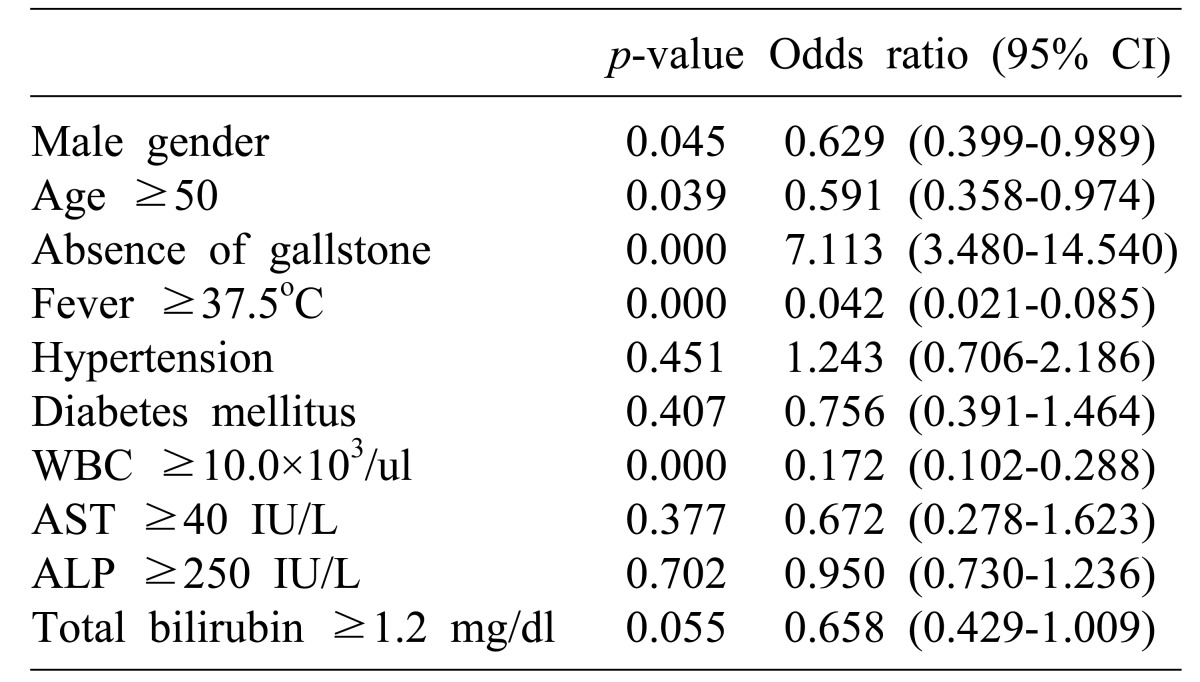
Univariate analysis identified 10 variables with a significant association with acute cholecystitis (Table 5). We included all ten variables in a multivariate logistic regression model. In the multivariate analysis, hypertension, diabetes, elevation of ALP, elevation of AST and ALT, and elevation of total bilirubin were not independently associated with acute cholecystitis.
Go to : 
It is quite a meager description to say that cholecystitis is an inflammatory change in the gallbladder, thereby identifying only the pathologic conditions. Clinically cholecystitis is characterized by symptoms of dyspepsia, right upper quadrant abdominal pain, and fever. Moreover, it is accompanied by changes in laboratory results, reflecting biliary inflammation or cholestasis. Thus, the concept of cholecystitis includes all the above changes in addition to the pathologic changes. Often it occurs in association with gallbladder stones. However, acalculous cholecystitis may occur, especially in patients in a critical, unstable condition. In contrast to the cholecystitis associated with gallbladder stones, the progression of acalculous cholecystitis is abrupt and fatal.23 Thus, we analyzed the presence of gallbladder stones as one risk factor requiring emergency cholecystectomy.4
It is known that cholecystitis is often caused by obstruction of the cystic duct. Known risk factors for gallbladder stones include old age, female gender, obesity, multiparity, family history, rapid weight loss, physical inactivity, dietary habit, oral contraceptives and others. However, acalculous cholecystitis is not just caused by obstruction of the cystic duct. Ischemia or hypomotility of the gallbladder and cholestasis associated with hypomotility are presumed to be the underlying causes.4 This study was focused on determining whether or not objective factors such as sex, age, and obesity are associated with different clinical manifestations of cholecystitis.
Being a female is a risk factor of gallstone. However, several studies have shown that severe cholecystitis occurs frequently in males. Lein and Huang5 insisted that male sex and age over 60 are risk factors for acute cholecystitis. Although several groups investigated sex as a risk factor for developing acute cholecystitis, not a single study was able to provide a reason for differences in prevalence by sex. It is only presumed that such a difference might have arisen from complex multi-factorial interactions among different variables. These variables include biological differences such as peritoneal cavity size, fat composition, or hormones, differences in co-morbidity, dietary habits, and even the conventional idea that males are reluctant to ask for medical advice.678
Considered as a risk factor for developing gallbladder stones, obesity has been investigated in several epidemiologic studies for its relationship with cholecystitis or gallbladder stones. However, our results showed that it would not be adequate to use BMI as a predictor of clinical manifestations of cholecystitis.9 Moreover, some studies reported that there was a negative correlation between obesity and acute cholecystitis. Although a detailed explanation was not provided, it was postulated that fat tissues might prevent progressive inflammatory reactions in gallbladder.10
The prevalence of cholecystitis has increased along with a gradual increase in lifespan.11 Complications of cholecystitis are increased in frequency in the elderly. Supported by several previous studies and this study, disease progression in the elderly exhibits an abrupt and arduous character.1213 However, as mentioned in previous studies, elderly patients often present with atypical symptoms and signs. They also frequently suffer from diseases other than biliary disease, such as diabetes mellitus, cardiovascular disease, cerebrovascular disease, and respiratory disease, leading to poor general condition. Thus, it is more likely to present with atypical clinical manifestations and a poor prognosis. Considering many diseases and poor general condition of the elderly, it is inappropriate to draw the conclusion that a higher prevalence rate of acute cholecystitis is observed in the elderly.
Most studies on risk factors investigated a single risk factor, and each study showed a different result for the same risk factor. Hence, this variability makes it difficult to standardize results. It is quite obscure to compare our study result to previous ones.
Recently, Cho et al.14 reported that there is a correlation between the development of acute cholecystitis and cerebrovascular disease. Atherosclerosis was suggested as the underlying cause, with effects on the functioning of the cystic artery. Ischemic change to the gallbladder induces acute cholecystitis. Until now, the correlation between cholecystitis and cerebrovascular disease has not been studied; nor has cerebrovascular disease been considered as a risk factor, it is highly valuable to recognize cerebrovascular disease as one possible cause of cholecystitis. Although our study did not show statistical significance for the difference between acute cholecystitis and cerebrovascular disease in the elderly (p=0.300), a larger sample size and better control of confounding variables might show significance. Further studies on the correlation between acute cholecystitis and cerebrovascular disease in the elderly should be carried out.
In contrast to cerebrovascular disease, the correlation between cardiovascular disease and acute cholecystitis has been persistently investigated in many epidemiologic studies.15 However, a direct correlation is still inexplicable, and interpretation of the results encompasses obscurity, and has led to an enormous debate on possible reasons for the correlation. Reflecting on past epidemiologic studies on either cardiovascular disease or cholecystitis, some risk factors for cardiovascular disease coincide partly with risk factors for cholecystitis. Such study results support the hypothesis that there is a correlation between cardiovascular disease and cholecystitis. Moreover, in the San Antonio Heart Study, Diehl et al.16 reported that moderate hypercholesterolemia and moderate to severe hyperlipidemia are observed in patients with cholecystitis. On the other hand, the level of HDL-cholesterol had an inverse relationship with cholecystitis, although this remains to be confirmed by further studies.
Additionally the correlation between diabetes mellitus and gallbladder stones has been constantly reported. Patients with diabetes tend to exhibit detrimental clinical manifestations, and they are recommended for early surgical treatment if a symptomatic gallbladder stone is present.171819 Some studies even assert that, regardless of symptoms and signs of cholecystitis, patients with diabetes should be considered for prophylactic cholecystectomy if gallbladder stone is present.20
Laparoscopic cholecystectomy is considered the treatment of choice for symptomatic gallbladder stone due to several advantages, including a low rate of morbidity, reduced postoperative pain, fewer hospital days, more rapid recovery and return to the normal lifecycle, and cosmetic effects.21 Indeed, this procedure is now widely used in diseases such as acute cholecystitis, gallbladder empyema, and common bile duct stones, which were considered contraindications during the early reconciliation period. Although laparoscopic cholecystectomy is effective, it is sometime inevitable to convert from laparoscopy to laparotomy when encountering various circumstances, such as uncontrolled hemorrhage, severe inflammation and adhesion, or damage to biliary tract and adjacent organs.22 Thus, there has been deliberation on the option to undergo emergency laparoscopic cholecystectomy rather than preoperative percutaneous transhepatic gallbladder drainage for patients with moderate to severe acute cholecystitis, which may result in higher morbidity and mortality. Kim et al.23 reported that preoperative percutaneous transhepatic gallbladder drainage could reduce postoperative complications after laparoscopic cholecystectomy and conversion to laparotomy, but this only applied to high-risk patients who undergo an emergency operation. Application of early laparoscopic cholecystectomy to patients without high risk would bring about reduction in complications, shortening of hospital stay, or re-admission. Consequently, higher cost-effectiveness can be accomplished, which is in accord with other research data.2124 However, considering that elective laparoscopic surgery is only converted to laparotomy at a rate of 5%, emergency laparoscopic cholecystectomy reaches its conversion rate up to 30%. Therefore, early detection, prompt decision making, and an appropriate surgical plan will be critical to patients with gallbladder stones with a greater possibility of developing acute cholecystitis. This may have a positive influence on the prognosis.25
Yacoub et al.26 suggested that adapting a scoring system, based on age, pulse, sex, leukocytosis, and gallbladder wall thickening detected on ultrasound, could distinguish patients who require surgical treatment. After selecting patients, applying early surgical treatment might prevent disease progression to necrotizing cholecystitis or gallbladder empyema. Based on similar studies that were previously conducted, establishing risk factors in symptomatic patients with cholecystitis is necessary. Also, interdisciplinary work to standardize diagnostic and treatment methods will be fundamental to reduce morbidity and postoperative complications in patients with gallbladder stones with or without cholecystitis.
In conclusion, male gender and old age as risk factors for acute cholecystitis are statistically significant. The presence of fever or leukocytosis is significantly correlated with acute onset of cholecystitis. Moreover, patients with diabetes or hypertension are apt to develop acute cholecystitis, though further studies should be carried out to validate this conclusion. Therefore, patients who are male or old and patients with presence of fever or leukocytosis should be evaluated in detail. Early elective surgical treatment and early intervention would be critical to bring about an optimal prognosis and to prevent postoperative complications.
Go to : 
References
1. Kim IS, Myung SJ, Lee SS, Lee SK, Kim MH. Classification and nomenclature of gallstones revisited. Yonsei Med J. 2003; 44:561–570. PMID: 12950109.

2. Trowbridge RL, Rutkowski NK, Shojania KG. Does this patient have acute cholecystitis? JAMA. 2003; 289:80–86. PMID: 12503981.

3. Kim JY, Lee MK, Kang YJ, Kim CN, Cho BS, Park JS. Clinical analysis of acalculous cholecystitis. Korean J Hepatobiliary Pancreat Surg. 2005; 9:216–220.
4. Chari RS, Shah SA. Biliary system. In : Townsend CM, editor. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 2007. 18th ed. Philadelphia: WB Saunders;p. 1556–1560.
5. Lein HH, Huang CS. Male gender: risk factor for severe symptomatic cholelithiasis. World J Surg. 2002; 26:598–601. PMID: 12098053.

6. Hinchey EJ, Elias GL, Hampson LG. Acute cholecystitis. Surg Gynecol Obstet. 1965; 120:475–480. PMID: 14262043.
7. Glenn F, Dillon LD. Developing trends in acute cholecystitis and choledocholithiasis. Surg Gynecol Obstet. 1980; 151:528–532. PMID: 7414465.
8. Margiotta SJ Jr, Horwitz JR, Willis IH, Wallack MK. Cholecystectomy in the elderly. Am J Surg. 1988; 156:509–512. PMID: 3202263.

9. Chang WT, Lee KT, Huang MC, et al. The impact of body mass index on laparoscopic cholecystectomy in Taiwan: an oriental experience. J Hepatobiliary Pancreat Surg. 2009; 16:648–654. PMID: 19387531.

10. Lee HK, Han HS, Min SK. The association between body mass index and the severity of cholecystitis. Am J Surg. 2009; 197:455–458. PMID: 18760398.

11. Huber DF, Martin EW Jr, Cooperman M. Cholecystectomy in elderly patients. Am J Surg. 1983; 146:719–722. PMID: 6650754.

12. Fried GM, Clas D, Meakins JL. Minimally invasive surgery in the elderly patient. Surg Clin North Am. 1994; 74:375–387. PMID: 8165473.

13. Cho JY, Kim JY, Chang SK, Kim SG, Hwang YJ, Yun YK. Is laparoscopic cholecystectomy safe in octogenarians? J Korean Surg Soc. 2009; 76:231–235.

14. Cho JY, Han HS, Yoon YS, Ahn KS. Risk factors for acute cholecystitis and a complicated clinical course in patients with symptomatic cholelithiasis. Arch Surg. 2010; 145:329–333. PMID: 20404281.

15. Cher DJ. Myocardial infarction and acute cholecystitis: an application of sequence symmetry analysis. Epidemiology. 2000; 11:446–449. PMID: 10874553.

16. Diehl AK, Haffner SM, Hazuda HP, Stern MP. Coronary risk factors and clinical gallbladder disease: an approach to the prevention of gallstones? Am J Public Health. 1987; 77:841–845. PMID: 3496013.

17. Lieber MM. The incidence of gallstones and their correlation with other diseases. Ann Surg. 1952; 135:394–405. PMID: 14903868.

18. McSherry CK, Ferstenberg H, Calhoun WF, Lahman E, Virshup M. The natural history of diagnosed gallstone disease in symptomatic and asymptomatic patients. Ann Surg. 1985; 202:59–63. PMID: 4015212.
19. Aucott JN, Cooper GS, Bloom AD, Aron DC. Management of gallstones in diabetic patients. Arch Intern Med. 1993; 153:1053–1058. PMID: 8481073.

20. Shpitz B, Sigal A, Kaufman Z, Dinbar A. Acute cholecystitis in diabetic patients. Am Surg. 1995; 61:964–967. PMID: 7486428.
21. Simopoulos C, Botaitis S, Polychronidis A, Tripsianis G, Karayiannakis AJ. Risk factors for conversion of laparoscopic cholecystectomy to open cholecystectomy. Surg Endosc. 2005; 19:905–909. PMID: 15868267.

22. Bang JS, Choi YS, Kim BG, et al. Comparative clinical analysis of 111 laparoscopic cholecystectomy cases converted to open procedures. Korean J Hepatobiliary Pancreat Surg. 2008; 12:168–172.
23. Kim SW, Kim SY, Hong SK, et al. Clinical benefits of preoperative percutaneous transhepatic gallbladder drainage in patients older than sixty with acute cholecystitis. Korean J Hepatobiliary Pancreat Surg. 2010; 14:184–190.
24. Borzellino G, Sauerland S, Minicozzi AM, et al. Laparoscopic cholecystectomy for severe acute cholecystitis. A meta-analysis of results. Surg Endosc. 2008; 22:8–15. PMID: 17704863.

25. Ibrahim S, Hean TK, Ho LS, Ravintharan T, Chye TN, Chee CH. Risk factors for conversion to open surgery in patients undergoing laparoscopic cholecystectomy. World J Surg. 2006; 30:1698–1704. PMID: 16927065.

26. Yacoub WN, Petrosyan M, Sehgal I, Ma Y, Chandrasoma P, Mason RJ. Prediction of patients with acute cholecystitis requiring emergent cholecystectomy: a simple score. Gastroenterol Res Pract. 2010; 2010:901739. PMID: 20631896.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download