Abstract
Backgrounds/Aims
Complete elimination of intrahepatic duct (IHD) stones is difficult and IHD stone disease is frequently associated with various complications, recurrence and sometimes cholangiocarcinoma. Therefore, we analyzed the long-term surgical results and evaluated the management currently considered appropriate.
Methods
Overall 110 patients who had been diagnosed with benign IHD stone disease and who underwent surgical treatment were enrolled in this study. The patients were categorized into three groups according to the type of surgery performed; liver resection (LR) group, intrahepatic duct exploration (IHDE) group and hepaticoenterostomy (HE) group. We compared and analyzed the results of these three groups.
Results
The number of cases in the LR group, IHDE group and HE group were 77, 25 and 8 respectively. The LR group required a longer operation time (p=0.000), more frequent transfusion (p=0.028) and had higher morbidity (p=0.049). However, the LR group had a higher clearance rate (90.9%) (p=0.000) than the other groups. In addition, there were a total of 22 cases of IHD stone recurrence during the follow-up, but there was no statistically significant difference among the three groups. The location of IHD stones was related to a risk factor for incomplete stone removal, but not for recurrence.
Conclusions
The fundamental principle for the treatment of IHD stone disease should be liver resection. However, it can lead to a longer operative time and higher rate of complications than the other procedures. There is also no difference in the IHD stone recurrence rate among the procedures. Therefore, these alternative and minor procedures could also be taken into account for patients with poor preoperative condition.
Go to : 
Intrahepatic duct (IHD) stone disease is considered when biliary stones exist within the bile ducts in the liver, especially at the proximal portion of the bifurcation of the right and left main hepatic ducts.12345678910111213 IHD stones can be classified according to their origin. Primary IHD stones develop in the IHD initially and are commonly accompanied by stricture of the bile ducts. Secondary IHD stones are formed within the common bile duct (CBD) or gallbladder and then move into the IHD.234
IHD stones are prevalent among patients between 40 to 50 years of age. This indicates that IHD stones are prevalent in a younger age group than that of patients with gallbladder stones.1234567 IHD stones develop more frequently in women and also have a tendency to occur in the left liver. Geographically, primary IHD stones are relatively common in East Asian countries including Korea, Japan, China and Taiwan. On the other hand, this disease is very rare in Western countries.123568
IHD stones are the common cause of recurrent cholangitis and liver abscess that sometimes can cause septic conditions and lead to fatal results, and IHD stones are the risk factor for biliary cirrhosis and cholangiocarcinoma.1345891011 Therefore the timing and method of treatment can affect the prognosis of patients with IHD stones. Additionally, cholangiocarcinoma can occur in 2.4-10.0% of patients with IHD stones.3121314 Hence, the probability of developing cholangiocarcinoma is always taken into account during the diagnosis and treatment of IHD stones and even during the follow-up examination in the clinical field.
In the recent years, the treatment for IHD stone disease has aimed to achieve complete stone removal using the surgical approach. But it is hard to choose the appropriate surgical modality due to the difficulty in removing the stones completely during operation, frequent complications after operation and higher recurrence rate. Therefore, there have been considerable changes in the treatment modality for the IHD stone disease and the debate regarding the appropriate surgical modality has continued till date.156715 It was reported that choledochoenterostomy was carried out more frequently than hepatectomy before the year 1985, but from the year 1986 onwards, hepatectomy has been performed more frequently than choledochoenterostomy.7
In this study, we tried to determine the most effective surgical modality for the IHD stone disease by analyzing the parameters such as clearance rate and recurrence rate, and the risk factors affecting these parameters in three types of surgical treatments.
Go to : 
From January 2000 to January 2010, 110 patients who had been diagnosed with IHD stone disease and who had undergone surgical treatment at our hospital were enrolled in this study. These patients had been diagnosed with benign disease only and had received adequate information on various surgical treatment options and findings. Adequate informed consent was obtained from the patients regarding surgical decision, risk and results.
According to the modality of surgical treatment, the patients were categorized into three groups, one group was of the patients who had undergone liver resection (LR group), another group was of the patients who had undergone choledochoscopic IHD exploration (IHDE group) only, and the last group was of the patients who had undergone only hepaticoenterostomy without liver resection (HE group). We reviewed the medical records of enrolled patients retrospectively and analyzed the demographic characteristics, clinical features, outcomes of treatment and follow-up results.
The basic test for diagnosing IHD stone disease was abdominal ultrasonography. In the cases which were accompanied by the complications of IHD stones such as liver atrophy or air bubbles within the bile ducts, abdominal computed tomography (CT) with contrast or magnetic resonance cholangiopancreatography (MRCP) were performed additionally.16
Liver resection was performed preferentially for multiple IHD stones in cases when the stones were localized in a unilateral lobe or several consecutive segments that could be resected entirely, especially when they were accompanied by complex parenchymal disease such as ductal stricture, atrophy or abscess. If there is an evidence of coexisting cholangiocarcinoma on radiologic or laboratory examination, liver resection should be performed.245891517 In our study, we had excluded the cases with malignancy or suspicious for malignancy on preoperative evaluation. But, if there were lesions suspicious for malignancy during operation, we performed liver resection although the patient had simple stones without complications. When IHD stones existed in the bilateral lobes, because of the impossibility to remove the affected liver parenchyma entirely, the unilateral lobe that had more severely complicated lesions was resected and then choledochoscopic IHD exploration was performed to eliminate the residual stones in the remnant lobe through the CBD or the exposed bile ducts on the resected surface. We carried out IHDE for simple cases in which complete elimination of stones was possible with only choledochoscopic lithotripsy followed by duct exploration. In cases of the patients who were anticipated to be having inoperable adhesions due to a previous operation of the hepatobiliary system or preoperative high-risk patients who had poor systemic conditions or patients who were expected to develop fatal complications, even death, we also chose to perform IHDE only or bypass procedure, such as HE. In cases of patients who refused to undergo liver resection due to their or their families' wishes, we again performed IHDE only or bypass procedure. When the patients with IHD stone disease had stricture and dilatation of the extrahepatic duct (EHD), we carried out liver resection with hepaticoenterostomy or only hepaticoenterostomy, considering the preoperative condition of the patients. Intraoperative choledochoscopy was performed in all the patients to confirm the existence of residual stones.713
Residual or recurrent IHD stones were distinguished from each other based on the two-month time point of detection, so the stones which were detected at two months after operation were diagnosed as recurrent IHD stones.10 Abdominal ultrasonography or CT was performed annually after the operation for follow-up, but when the symptoms of cholangitis, such as discomfort or pain in the right upper quadrant of the abdomen, dyspepsia, fever or jaundice appeared after the operation, abdominal ultrasonography or CT was performed immediately after the hospital visit to confirm the relapse without considering the periodic examinations.110
Statistical analysis was done with SPSS ver. 18.0 (Chicago, Inc.). Continuous variables were analyzed by Student's t-test, recurrence and clearance rate was analyzed by Chi-square test and odds ratio was obtained by the logistic regression test. Two tailed p-value less than 0.05 was considered statistically significant.
Go to : 
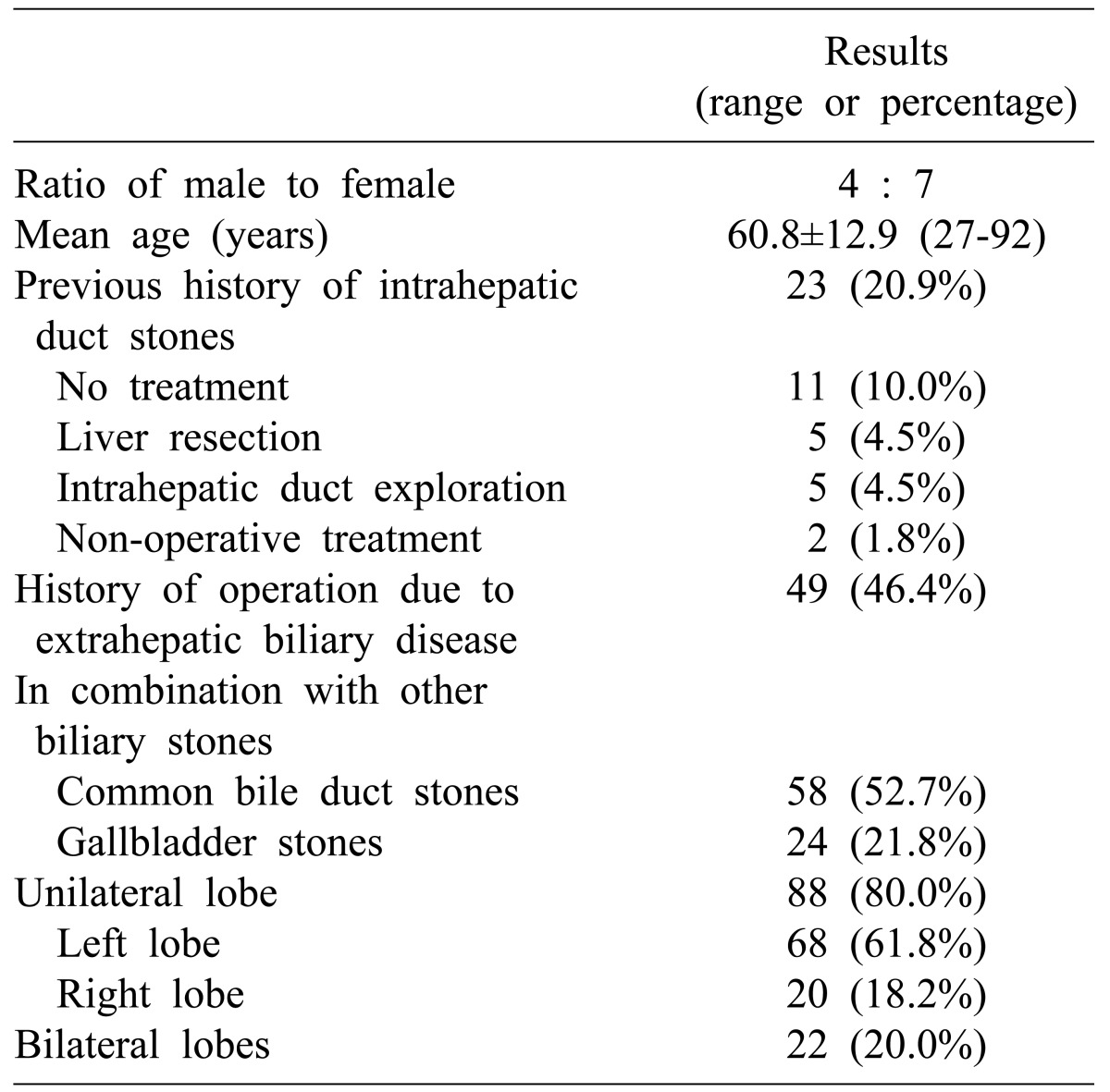
The average age of the 110 patients enrolled in the study was 60.8±12.9 years and 40 patients were males and 70 patients were females. 23 patients (20.9%) had a prior history of IHD stone disease and among them, 12 patients (10.9%) had received treatment, while the remaining 11 patients (10.0%) did not have any specific symptoms and hence had not been treated but had been kept under observation.
Of the 12 patients who had been treated, 10 patients (9.1%) had undergone surgical procedures and two patients (1.8%) had undergone non-surgical procedures, such as insertion of percutaneous drainage. Of the 10 patients who had undergone surgical procedures, 5 patients (4.5%) had undergone liver resection and 5 patients (4.5%) had undergone IHD exploration. 49 patients (44.5%) had received surgical treatments for biliary system diseases other than IHD stone disease. Among them, 2 patients had been diagnosed as having choledocholithiasis and had undergone choledochojejunostomy with cholecystectomy and the remaining 47 patients had been diagnosed as having cholecystitis with or without gallbladder stones and had undergone cholecystectomy. 58 patients (52.7%) had CBD stones and 24 patients (21.8%) had gallbladder stones at the time of diagnosis of IHD stone disease (Table 1).
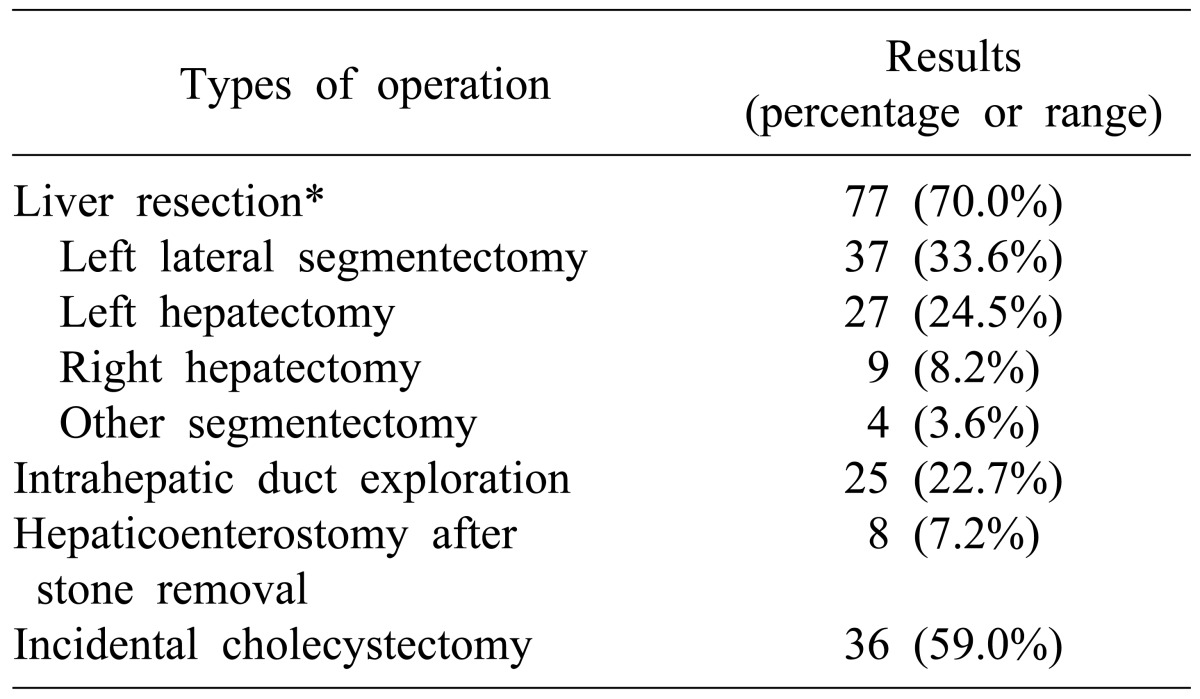
Among the patients diagnosed with IHD stones, 77 patients (70.0%) underwent liver resection, 25 patients (22.7%) underwent IHD duct exploration only and the other 8 patients (7.3%) underwent only hepaticoenterostomy without liver resection. Cholecystectomy was performed in 36 patients (59.0%) while the patients who had a prior history of cholecystectomy were excluded (Table 2).
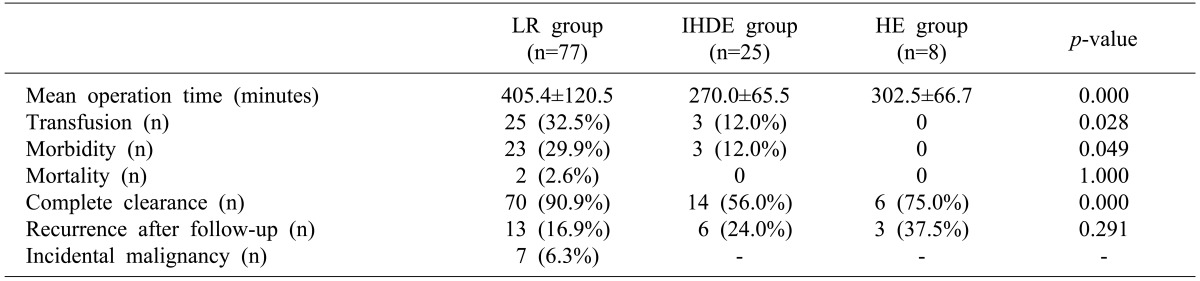
The mean operation time was 366.6±123.7 minutes in the total patients. The mean operation time in the LR group, HE group and IHDE group was 405.4±120.5 minutes, 302.5±66.7 minutes and 270.0±65.5 minutes respectively, and a statistically significant difference was seen among the three groups (p=0.000) (Table 3).
Postoperative complications occurred in 26 (23.6%) of the 110 patients. 23 complications occurred in the LR group with an incidence of 29.9% and 3 complications occurred in the IHDE group with an incidence of 12.0%. The difference in the incidence between the two groups was statistically significant (p=0.049). Of the 110 patients, 28 patients (25.4%) received transfusion postoperatively. In the LR group, postoperative transfusion was given to 25 patients (32.5%) and to 3 patients (12.0%) in the IHDE group. This result was also statistically significant (p=0.028).
During the perioperative period, 7 cases (6.3%) of malignancy were identified. All of them had histological cholangiocarcinoma of an early stage and liver resection with cholecystectomy was carried out in these cases. There was no recurrence during the follow-up period (Table 3).
There were two postoperative deaths in the LR group only, one was due to septic shock and the other was due to uncontrolled postoperative bleeding (Table 3). Both cases had poor preoperative conditions and complications.
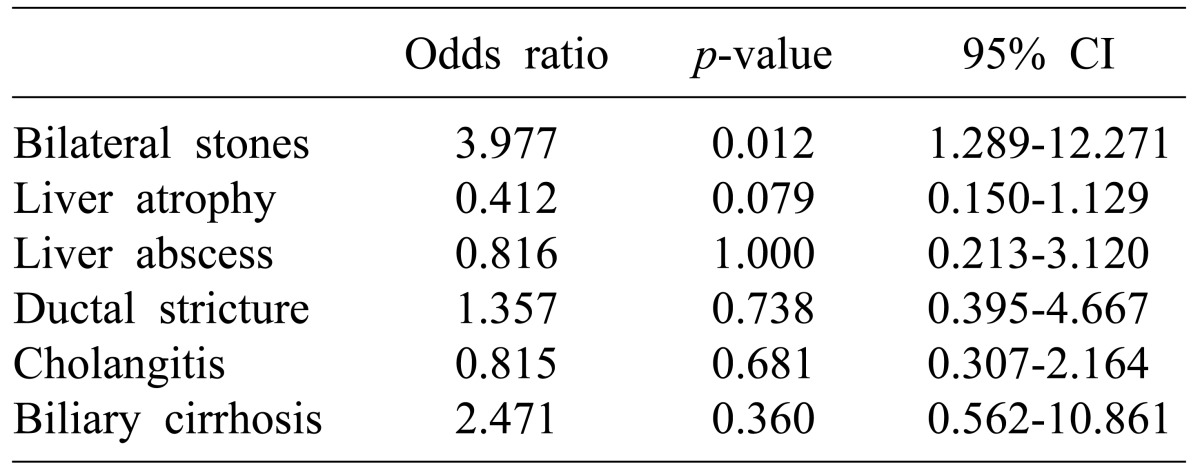
Residual stones were identified in 21 patients immediately after the operation and additional residual stones were detected in three patients within 2 months during the short-term follow-up examination. Meanwhile, of the 21 patients in whom residual stones were detected immediately after the operation, 4 patients did not have residual IHD stones on postoperative radiologic examination. We think that the residual stones could have been excreted naturally in these patients. Thus finally, the total number of patients with residual stones was 20 and the stone clearance rate in our study was 82.0%. Difference in the stone clearance rate among the three groups was statistically significant, the stone clearance rate was 90.9% in the LR group, 75.0% in the HE group and 56.0% in the IHDE group, respectively (p=0.000) (Table 3). Comparing the risk of residual stones based on the distribution of stones in the liver, the occurrence rate of residual stones was 13.6% when the stone was located in a unilateral lobe, whereas when the stone was located in the bilateral lobes, the occurrence rate was 63.2%. The risk of residual stones in the patients with bilateral IHD stone disease was four times higher than that in those with unilateral IHD stone disease and it was statistically significant (OR 3.977; 95% CI 1.289-12.271; p=0.012). Meanwhile, the existence of complex hepatic lesions, namely liver atrophy, abscess, ductal stricture, cholangitis and biliary cirrhosis did not affect the incidence of residual IHD stones in this study (Table 4).
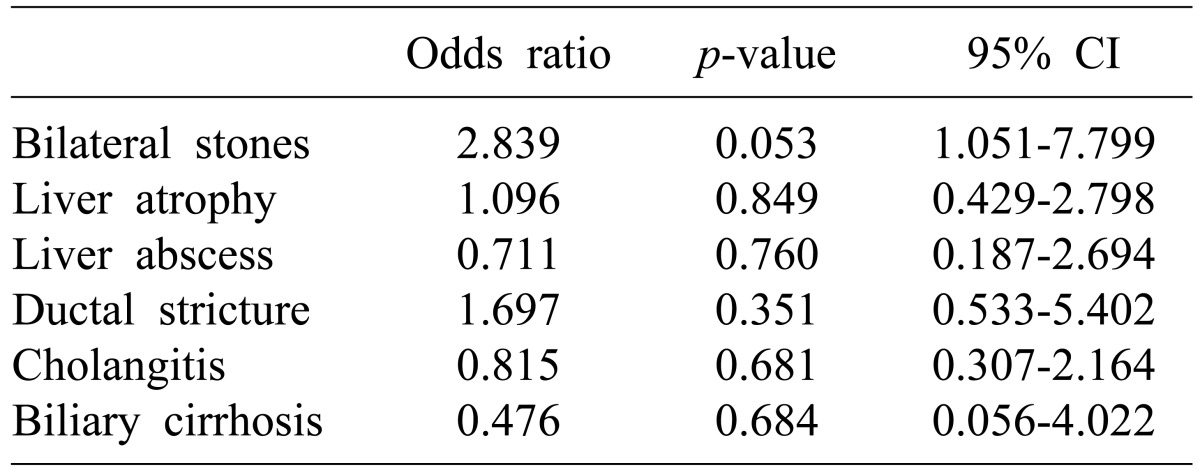
The mean follow-up period for this study was 30.9 months and it was not different among the three groups. During the follow-up period, relapse of IHD stone disease occurred in 22 patients and the recurrence rate was 20.0%. Comparing the stone recurrence rate in each group, the number of stone recurrences was 13 in the LR group, 3 in the HE group and 6 in the IHDE group, and the recurrence rate was 16.9%, 37.5%, and 24.0% respectively, which was not a statistically significant difference (p=0.291) (Table 3). Measuring the stone recurrence rate according to the distribution of IHD stones, the stone recurrence rate was 68.2% when the IHD stones were localized in a unilateral lobe, whereas when the IHD stones existed in the bilateral lobes the stone recurrence rate was 31.8% and there was only crude correlation between the stone recurrence rate and the distribution of IHD stones (OR 2.839; 95% CI 1.051-7.799; p=0.053). The complex lesions, such as liver atrophy, abscess, ductal stricture, cholangitis and biliary cirrhosis did not affect the IHD stone recurrence rate either (Table 5).
Go to : 
IHD stone disease has been considered clinically as a malignancy due to the less likelihood of complete recovery, high incidence of recurrence and complications. Moreover, it may lead to the development of cholangiocarcinoma even after complete elimination of all the stones is achieved. Hence, it is accompanied by the difficulties and torments of making a decision regarding the modality of the treatment to be used.156715 In fact, surgeons sometimes encounter patients with complex IHD stone disease who have poor general conditions. The patients are mostly older in age having systemic diseases, such as cardiovascular, pulmonary disease and/or diabetes mellitus, or they allow the disease to progress and visit the hospital very late. In these cases, surgeons have to agonize over selection of the best treatment for these patients although they are aware of the traditional surgical treatment modalities. Therefore, clinical trials are needed to determine the most effective surgical modality for the treatment of IHD stone disease, and an analysis of the risk factors that affect the outcomes of the operation such as stone clearance rate, recurrence rate and complications after the operation is very important.
According to the previous studies, the incidence of postoperative complications was 12.0-38.5% after LR, 24.3-38.0% after HE and 2.1-40.0% after IHDE.57810181920212223 In this study, the incidence of postoperative complications was 29.9% after LR, 12.0% after IHDE and there were no cases of postoperative complications after HE. The incidence of complications in patients who underwent LR and IHDE was in concordance with the results of prior studies, but the patients who underwent HE showed a highly lower incidence of complications.581821 This was probably due to the bias as a result of the small number of patients in the HE group than in the other groups. But, the difference in the postoperative complication rate between the LR group and HE group was statistically significant and it could be an important consideration while selecting the surgical treatment modality in patients with IHD stone disease.
IHD stones are the well known risk factors for cholangiocarcinoma and cholangiocarcinoma has been shown to occur in 2.4-10% of patients with IHD stones.3121314 In this study, although the cases suspicious for malignancy on preoperative evaluation were excluded, 7 patients (6.3%) were diagnosed with incidental cholangiocarcinoma during the operation or postoperative period.
The clearance rate of the IHD stones in this study was 90.9% in the LR group, 56.0% in the IHDE group and 75.0% in the HE group. This difference was statistically significant. The clearance rate after LR was 88.0% in the study by Uenishi et al.5 and was 83.3% in the study by Cheon et al.,21 and these results coincided with the result of our study. On the other hand, it was reported that the clearance rate after IHDE was 63.9-78.2%.52123 And, the clearance rate after HE was 51.4% in the study by Uenishi et al.5 These results of the prior studies showed a marked distinction from the results of our study. This can be explained by the fact that the trials performed for the IHD stone removal with choledochoscopy failed because of the accompanying complex hepatic parenchymal lesions in many patients who underwent IHDE. The success rate of IHD stone removal with IHDE is dependent on the possible approach to the stone lesion with a choledochoscope. So, if there is a complex parenchymal lesion, such as ductal stricture or liver abscess, it becomes difficult to approach the stone lesion with a choledochoscope and the clearance rate of IHD stones decreased. In our study, complex parenchymal lesions were relatively more commonly identified. IHD stones were accompanied by ductal stricture and liver abscess in 32.0% and 24.0% of the patients in the IHDE group respectively. Furthermore, the population of the HE group was too small to estimate the appropriate statistical results, so there could be large differences from the results of the previous studies. But, the result of higher stone removal rate in the LR group of our study and prior studies can support the suggestion that liver resection, namely segmentectomy or hepatectomy, should be the principle for treatment of IHD stones, with an additional advantage of the possibility to eliminate not only the IHD stones but also the complex hepatic parenchymal lesions.181118
The recurrence rate of IHD stones after treatment has been reported to be about 6.0-22.0% in prior studies. In view of each surgical treatment modalities, the stone recurrence rate after LR was 10.0-18.0% and that after IHDE was 21.0-56.1%, and to conclude LR showed better results.5891011151718192123 In our study, the stone recurrence rate after LR, IHDE and HE were 16.9%, 24.0% and 37.5%, respectively. These results are similar to the results of prior study although statistical significance was not reached. This fact can support the hypothesis that the principle for the treatment of IHD stones should be LR only.
Hepatic parenchymal pathologic lesions that were identified preoperatively on radiologic examinations may affect the decision regarding the selection of the surgical treatment modality. Liver atrophy, liver abscess, ductal stricture, cholangitis and biliary cirrhosis did not affect the stone clearance rate and recurrence in our study. But, these pathologic lesions, especially biliary ductal stricture, have been considered to be the important risk factors for the relapse of IHD stones.14578910111517192123242526 According to the report by Uenishi et al.,5 the incidence of residual stones and the recurrence rate had been reported to be increased to up to 5.0 times and 40.5 times respectively when IHD stones were accompanied by ductal stricture than when IHD stones were not accompanied by ductal stricture. However, there was no significant relationship between the existence of ductal stricture and the stone clearance rate or the stone recurrence rate in our study. This result could be due to several reasons. First, we performed LR extensively to eliminate not only the stones but also the source of stones including the hepatic parenchymal pathologic lesions. Second, there might be limitations to collecting the information of patients using the method of retrospective review of the medical records, such as the official readings of radiologic examinations.
Comparing the patients with IHD stones localized in a unilateral hepatic lobe and bilateral lobes, the latter showed a 4.0 times higher incidence of residual stones after the treatments, although there was no definite significant difference in the recurrence rate of IHD stones. The report by Yang et al.,24 which was about the comparison and analysis of unilateral hepatectomy and bilateral hepatectomy in the surgical treatments of bilateral IHD stone disease, showed significant differences as the postoperative recurrence rate was 34.1% and 11.8%, respectively. However, 5.7% of patients undergoing bilateral hepatectomy expired due to postoperative complications. On the other hand, there was no mortality after unilateral lobectomy. These results suggest that although extensive liver resection exhibits favorable outcomes with respect to recurrence of IHD stones, a combination of various surgical treatments should be considered for the patients' recovery after the operation even in the cases with bilateral IHD stone disease.
In conclusion, LR facilitates IHD stone removal along with complete removal of the affected liver parenchyma and improves the stone clearance rate. Thus, it can definitely relieve the symptoms of IHD stone disease in the short term and decrease the incidence of cholangiocarcinoma in the long term by eliminating the pathologic hepatic lesions and resolving the bile stasis. However, LR also has the limitations of higher rate of postoperative complications and risk of fatal results in spite of the decreased recurrence rate compared with the other surgical modalities. Therefore, we recommend that the principle for the treatment of IHD stone disease should be liver resection. However, it can impose the burdens of a longer operative time, higher rate of complications and risk of fatal results. Thus, IHDE or HE could be an alternate choice in some patients who may not seem to endure liver resection based on the preoperative condition or age, if multiple combined modalities such as percutaneous choledochoscopic lithotripsy or endoscopic lithotripsy can be applied for the elimination of remnant stones after the operation.
Go to : 
References
1. Lim CS, Jang JY, Lee SE, Kang MJ, Kim SW. Recent treatment modalities for hepatolithiasis and long-term outcomes. Korean J Hepatobiliary Pancreat Surg. 2010; 14:37–45.
2. Kim MH, Sekijima J, Lee SP. Primary intrahepatic stones. Am J Gastroenterol. 1995; 90:540–548. PMID: 7717308.
3. Kim GH, Ok CM, Kim BJ, et al. A clinical review of gallstone diseases in Koreans. Korean J Gastroenterol. 1997; 29:352–361.
4. Ramia JM, Palomeque A, Muffak K, Villar J, Garrote D, Ferrón JA. Indications and therapeutical options in hepatolithiasis. Rev Esp Enferm Dig. 2006; 98:597–604. PMID: 17048996.

5. Uenishi T, Hamba H, Takemura S, et al. Outcomes of hepatic resection for hepatolithiasis. Am J Surg. 2009; 198:199–202. PMID: 19249730.

6. Huang MH, Chen CH, Yang JC, et al. Long-term outcome of percutaneous transhepatic cholangioscopic lithotomy for hepatolithiasis. Am J Gastroenterol. 2003; 98:2655–2662. PMID: 14687812.
7. Uchiyama K, Onishi H, Tani M, Kinoshita H, Ueno M, Yamaue H. Indication and procedure for treatment of hepatolithiasis. Arch Surg. 2002; 137:149–153. PMID: 11822950.

8. Otani K, Shimizu S, Chijiiwa K, et al. Comparison of treatments for hepatolithiasis: hepatic resection versus cholangioscopic lithotomy. J Am Coll Surg. 1999; 189:177–182. PMID: 10437840.
9. Marín C, Robles R, Pastor P, Parrilla P. Liver resection in the treatment of intrahepatic lithiasis. Immediate and long-term results in a single-center series. Rev Esp Enferm Dig. 2008; 100:225–229. PMID: 18563980.
10. Uchiyama K, Kawai M, Ueno M, Ozawa S, Tani M, Yamaue H. Reducing residual and recurrent stones by hepatectomy for hepatolithiasis. J Gastrointest Surg. 2007; 11:626–630. PMID: 17468921.

11. Kim YT, Byun JS, Kim J, et al. Factors predicting concurrent cholangiocarcinomas associated with hepatolithiasis. Hepatogastroenterology. 2003; 50:8–12. PMID: 12629979.
12. Kubo S, Kinoshita H, Hirohashi K, Hamba H. Hepatolithiasis associated with cholangiocarcinoma. World J Surg. 1995; 19:637–641. PMID: 7676713.

13. Su CH, Shyr YM, Lui WY, P'Eng FK. Hepatolithiasis associated with cholangiocarcinoma. Br J Surg. 1997; 84:969–973. PMID: 9240138.

14. Khan SA, Davidson BR, Goldin R, et al. British Society of Gastroenterology. Guidelines for the diagnosis and treatment of cholangiocarcinoma: consensus document. Gut. 2002; 51(Suppl 6):VI1–VI9. PMID: 12376491.

15. Chijiiwa K, Yamashita H, Yoshida J, Kuroki S, Tanaka M. Current management and long-term prognosis of hepatolithiasis. Arch Surg. 1995; 130:194–197. PMID: 7848091.

16. Park SW, Song SY, Kang JK, et al. The role of ultrasonography, computed tomography and magnetic resonance imaging in prediction of gallstone composition. Korean J Gastroenterol. 1995; 27:213–227.
17. Lee TY, Chen YL, Chang HC, Chan CP, Kuo SJ. Outcomes of hepatectomy for hepatolithiasis. World J Surg. 2007; 31:479–482. PMID: 17334864.

18. Kusano T, Isa TT, Muto Y, Otsubo M, Yasaka T, Furukawa M. Long-term results of hepaticojejunostomy for hepatolithiasis. Am Surg. 2001; 67:442–446. PMID: 11379645.
19. Chijiiwa K, Kameoka N, Komura M, Yamasaki T, Noshiro H, Nakano K. Hepatic resection for hepatolithiasis and long-term results. J Am Coll Surg. 1995; 180:43–48. PMID: 8000654.
20. Takada T, Uchiyama K, Yasuda H, Hasegawa H. Indications for the choledochoscopic removal of intrahepatic stones based on the biliary anatomy. Am J Surg. 1996; 171:558–561. PMID: 8678199.

21. Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS. Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery. 2009; 146:843–853. PMID: 19744434.

22. Chen MF, Jan YY, Hwang TL, Jeng LB, Yeh TS. Impact of concomitant hepatolithiasis on patients with peripheral cholangiocarcinoma. Dig Dis Sci. 2000; 45:312–316. PMID: 10711444.
23. Cheung MT, Kwok PC. Liver resection for intrahepatic stones. Arch Surg. 2005; 140:993–997. PMID: 16230551.

24. Yang T, Lau WY, Lai EC, et al. Hepatectomy for bilateral primary hepatolithiasis: a cohort study. Ann Surg. 2010; 251:84–90. PMID: 20032719.
25. Chen MF, Jan YY, Wang CS, et al. Role of hepatic resection in surgery for bilateral intrahepatic stones. Br J Surg. 1997; 84:1229–1232. PMID: 9313699.

26. Hwang JH, Yoon YB, Kim YT, Cheon JH, Jeong JB. Risk factors for recurrent cholangitis after initial hepatolithiasis treatment. J Clin Gastroenterol. 2004; 38:364–367. PMID: 15087697.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download