Abstract
Purpose
T-tube is a major procedure that prevents complication by biliary decompression, but which is accompanied by complications. Therefore, several procedures such as ENBD, PTBD, and antegrade biliary stent have been attempted, but with controversies as to which procedure is superior. Also, there are no standard procedures after laparoscopic CBD exploration. We performed this study to ascertain the most appropriate biliary drainage procedure after laparoscopic CBD exploration.
Methods
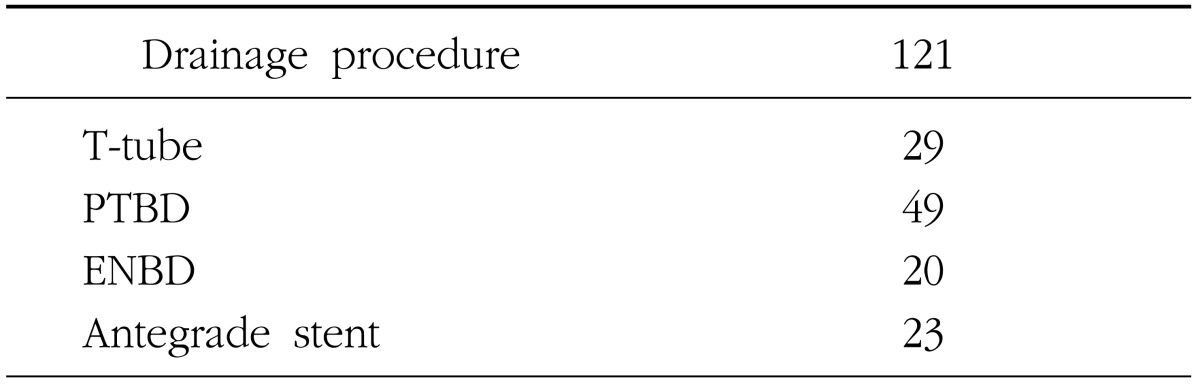
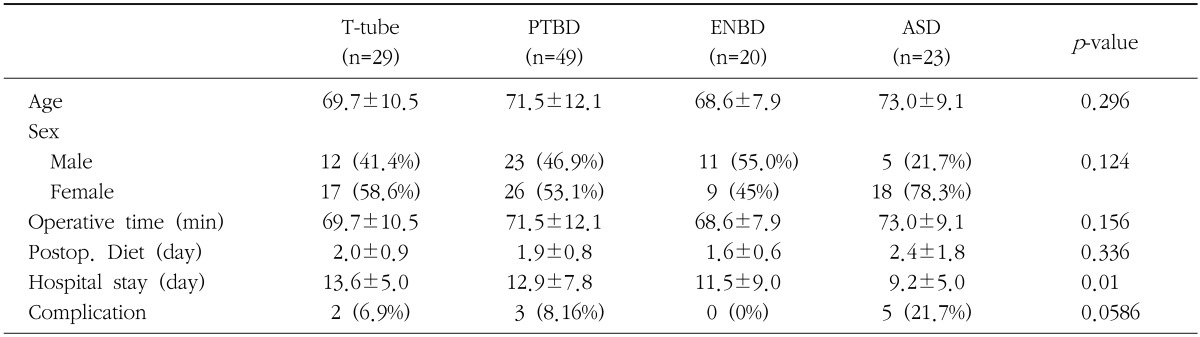
From March 2001 to December 2009, 121 patients who underwent Laparoscopic CBD exploration in Gunyang University were included for retrospective analysis. The patients were divided to 4 groups according to type of procedure, and we compared clinical parameters including age and gender, operation time, hospital stay, start of post-operative diet, and complications.
Results
There was no difference in age, gender, mean operation time, postoperative diet between the 4 groups. Hospital stay in the Stent group was shorter than T-tube group. There were 10 (7%) complications that occurred. Two 2 occurred in the T-tube, 3 in PTBD, and 5 in the Antegrade stent group. There were more complications in Stent group but no significant statistical difference. In 5 cases with remnant CBD stone, a total of 4 (3 PTBD, 1 Stent) was performed by endoscopic CBD stone removal. One T-tube case was removed easily by choledochoscopy through the T-tube. Three migrated and the impacted stents were removed by additional endoscopy. Perioperative biliary leakage (1) and peritonitis (1) post t-tube removal were resolved by conservative treatment.
After common bile duct exploration and choledocholithotomy, insertion of a biliary drainage catheter has been applied as the standard procedure to prevent complications. Among them, T-tube insertion has been applied most widely because of the advantage of decompressing the bile duct efficiently, as well as assessing and removing remnant common bile duct stones.1
Nevertheless, it has shortcomings which include postsurgical infection and hemorrhage of the biliary system, risk for the development of choleperitonitis if the T-tubes migrate or during its removal, the t-tube placement period after surgery is long, and the placement for a long time is inconvenient to patients.1234
To reduce such complications and discomfort of the T-tube, primary repair without biliary drainage has been attempted.45 In addition, instead of the T-tube, several biliary drainage procedures such as retrograde biliary stent insertion, percutaneous transhepatic biliary drainage (PTBD), endoscopic naso-biliary drainage (ENBD), etc. have been devised and performed.6 Presently, common bile duct exploration has changed from open abdominal surgery to endoscopic surgery in many cases, and the trend is that it is on the rise.7 The biliary drainage procedure after endoscopic common bile duct exploration has not been standardized, and at present, bile juice drainage itself is under controversy. Studies that compared several biliary drainage procedures after endoscopic common biliary duct exploration have not been conducted sufficiently, and thus studies that report effective drainage procedures with a low incidence of complications are not few. In addition, the standard for the selection of drainage procedures according to the condition of patients has not been established. In this study, 4 types of drainage procedures that may be applied after endoscopic common biliary duct exploration were compared and analyzed in order to determine the appropriate drainage procedures according to the patient condition.
A retrospective study was performed on patients who received common bile duct exploration and choledocholithotomy for common bile duct stones at the Gunyang University Hospital from March 2001 to December 2009. For patients with a large number of bile duct stones or large biliary stones, patients who were associated with gall bladder stones (GB stones), or patients who were associated with cholecystitis, endoscopic surgery was performed initially. For patients with duodenal diverticulae, difficult cases that precluded an endoscopic approach because of past stomach surgery, or patients whose stones were not completely removed by endoscopic treatment, an endoscopic common bile duct exploration was performed. The subjects were 121 patients excluding 13 patients who simultaneously received hepatectomy, and 3 patients who were converted to open abdominal surgery during surgery. The subjects were divided according to 4 types of biliary drainage procedure maintained after surgery, and the clinical indices such as age and gender, operation time, hospitalization period, the time of the initiation of diet after surgery, and complications were compared.
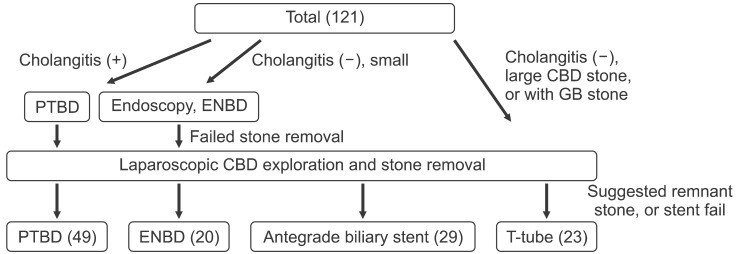
Of patients hospitalized for common bile duct stones, for patients who were suspected to have cholangitis prior to surgery, such as fever, increased leucocytes, or right abdominal pain, biliary drainage was performed by PTBD first, and surgery was performed after the improvement of inflammation. After surgery, PTBD was maintained continuously. For cases without symptoms of cholangitis, whose common bile duct stone diameter was less than 1 cm, and not associated with bile duct stones and cholecystitis, choledocholithotomy was attempted by sphincteropapillotomy. For cases in which choledocholithotomy failed, an EBND tube was inserted. This was followed by endoscopic common bile duct exploration and choledocholithotomy, and the EDNB tube was maintained instead of inserting a T-tube. Even if cholangitis symptoms were absent, if the size of common bile duct stone was large, or if cases were associated with cholecystitis and gall bladder stones, endoscopic surgery was performed as the initial procedure. After surgery, retrograde biliary stent insertion was performed first. When failed stent insertion or remnant stones in the common bile duct and the intrahepatic bile duct are anticipated, a T-tube was inserted (Fig. 1).
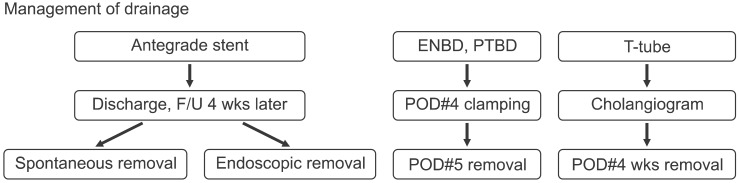
Patients with stent insertion were followed up for 4 weeks after surgery. For patients in whom spontaneous removal of the stent failed, it was removed endoscopically. ENBD and PTBD were closed on day 4 after surgery. Patients without fever and pain and not elevated bilirubin levels, the tubes were removed on the day 5 after surgery. Remnant stones were assessed by postsurgical cholangiography through the T-tube, and the T-tube was removed at 4 weeks at our outpatient clinic after discharge (Fig. 2).
Statistical analysis was performed by the Anova test, Kruskal-wallis test, Mann-Whitney test and Bonferoni correction. p-values less than 0.05 were considered to be significant.
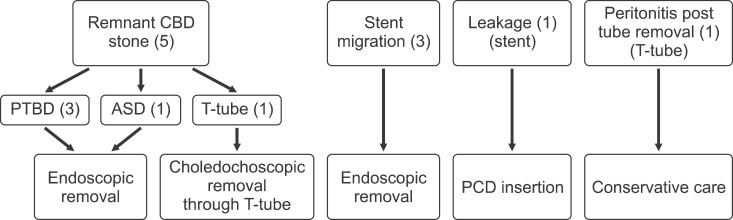
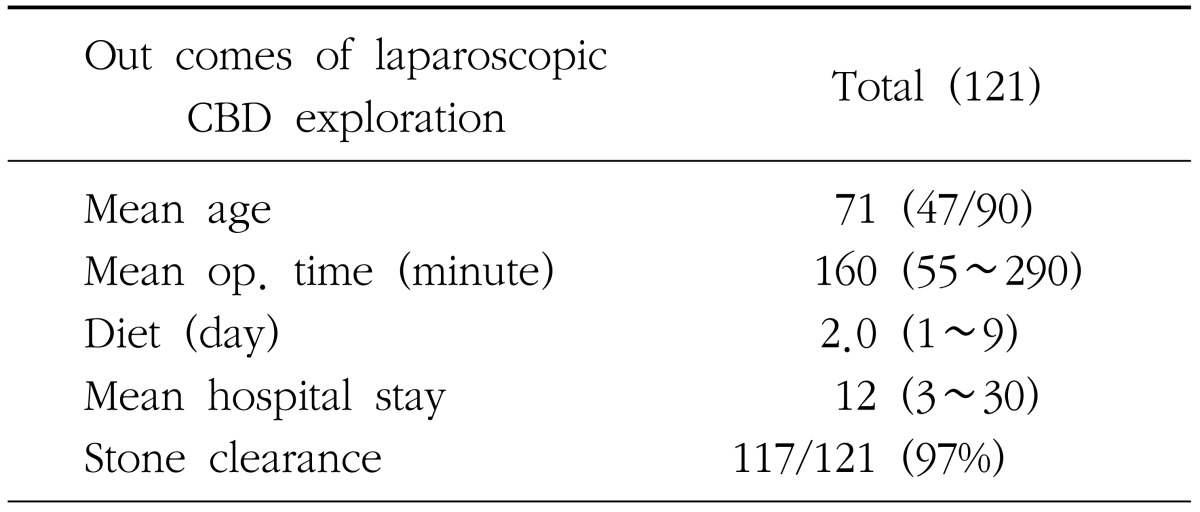
The mean age was 71 years. There were 51 male patients (41%) and 70 female patients (59%). The average operation time was 160 minutes. The average time of the initiation of food intake after surgery was 2 days. The average hospitalization period was 12 days, and the rate of biliary stone removal was 97% (Table 1). Of the total of 121 patients, T-tube was performed on 29 cases (24%), percutaneous transhepatic biliary drainage in 49 cases (40%), endoscopic naso-biliary drainage in 20 cases (16.5%), and retrograde stent insertion in 23 cases (19%) (Table 2). Group age and gender were not significantly different. Operation time was not different, and the initial food intake of the ENBD group was 1.6 days, which was shorter than other groups but not statistically significant. The hospitalization period of the T-tube insertion group was 13.6 days, the stent insertion group 9.2 days, and a significant difference between the two groups was shown (p<0.01). None of patients died after surgery. Ten patients developed complications, which represented 7% of the entire patients. These were bile juice leakage which occurred in 1 case, remnant bile duct stones in 5 cases, stent migration in 3 cases, and bile juice peritonitis developed after T-tube removal in 1 case. Development of complications according to drainage tube procedures comprised of T-tube in 2 cases (6.9%), percutaneous transhepatic biliary drainage in 3 cases (8.16%), endoscopic naso-biliary drainage in 0 case (0%), and the stent insertion in 5 cases (21.7%) (Table 3). Bile juice leakage developed in the stent insertion group, and after percutaneous drainage, it was treated by conservative management. There were remnant stones present after surgery in 1 case of the T-tube insertion group, 3 cases in the percutaneous transhepatic biliary drainage group, and 1 case in the stent insertion group. For the T-tube insertion group, remnant stones were removed easily biliary endoscopy through the T-tube and washing. In the remaining patients, remnant stones were removed by additional endoscopic sphincterotomy and lithotomy. In the Stent insertion group, stent migration occurred in 3 cases, and the stent was also removed by additional endoscopy. After removal of T-tube, 1 patient developed bile leakage, but the volume was small and it was thus treated with conservative management only (Fig. 3).
It has been reported that after endoscopic common bile duct exploration, primary repair of the bile duct without bile juice drainage was not significantly different from T-tube insertion.145 However, until now, the drainage of bile juice by T-tube insertion has been applied widely after endoscopic common bile duct exploration.48 The T-tube has advantages in that it prevents intrahepatic abscess and bile leakage from the repair area by decompression of the bile duct system, and remnant stones may be assessed by cholangiography through the T-tube after surgery and be removed by biliary endoscopy via the T-tubes with washing. However, problems are associated with T-tubes such as risk for postsurgical infection, hemorrhage, early T-tube migration, and bile peritonitis that may develop after removal, and inconvenience of having to be maintained for a long time.1234910 Because of such problems, several alternative biliary drainage procedures that may replace the T-tube have been performed, such as percutaneous transhepatic biliary drainage, endoscopic naso-biliary drainage, and retrograde stent insertion.
Advantages of percutaneous bile duct drainage tubes are that it may prevent several postsurgical complications similar to T-tubes. However, different advantages from T-tubes are that maintenance of the tube is less inconvenient, the maintenance period is short, there is less biliary leakage after removal of the drainage tube, and inflammation may be improved in patients associated with presurgical cholangitis. On the other hand, shortcomings are inconvenience of a procedure that has to be performed one more time prior to surgery, risks for complications caused by percutaneous transhepatic drainage tube insertion, and the difficulty or removing remnant stones after surgery. Endoscopic naso-biliary drainage tube also has advantages including prevention of postsurgical complications by decompression of the bile duct system, shorter maintenance period which is different from the T-tube, and prevention of peritonitis and intraabdominal abscess caused by the migration of the T-tube or percutaneous transhepatic biliary drainage. However, associated shortcomings are that although remnant stones may be assessed after surgery, additional endoscopic procedures have to be performed for removal of remnant stones. Finally, with regard to retrograde stent insertion, it may prevent biliary leakage by significantly decreasing the biliary duct pressure. In addition, several recent studies have observed that the procedure that inserts a retrograde stent after endoscopic choledocotomy and performs simple repair is an effective procedure which may replace T-tube.6
In addition, significant advantages are that the inconvenience due to the maintenance of drainage tubes can be avoided, and the patients can return early to their normal life. Nevertheless, it also has shortcomings. If the stent is removed spontaneously, it has to be removed by endoscopic procedures, and it has risks for biliary atresia and cholangitis caused of the migration of stent, and remnant stones after surgery may not be removed readily. In our study, an additional endoscopic procedure was performed in 3 cases because of the migration of the stent to the bile duct. In addition, it was not removed spontaneously and thus an additional endoscopic procedure was performed in 3 cases. Also, other studies have revealed that in cases with intestinal adhesion or intestinal diverticulum, intestinal perforation occurs due to stent migration has been reported.1112
In our study, the operating time of the groups, the time of the initiation of food intake after surgery, the incidence of major complications were not significantly different. T-tubes were useful for the removal of remnant common bile duct stones, the maintenance period of T-tube was long (4 weeks), and the maintenance of the tube was inconvenient to patients. The hospitalization period of the stent group was short, and thus the patients experienced less discomfort. Nonetheless, if the stent migrated or spontaneous removal of stent failed, additional endoscopic procedures were required.
T-tube was advantageous for patients who were suspected to have remnant common biliary stones as biliary stones may be removed without additional endoscopic procedures. In addition, for cases who maintained an endoscopic naso-biliary drainage tube, to use T-tube may be an adequate method for the prevention of complications caused by the T-tube if remnant biliary stones are not anticipated. It is thought that the application of drainage procedures suitable to each patient is the best drainage procedure, for example, for patients with suspected cholangitis, the procedure that consists of percutaneous transhepatic biliary drainage first and maintenance after surgery. In addition, recent efforts to reduce complications and discomfort caused by the drainage tubes, studies on primary repair without the insertion of drainage tubes are ongoing, and it is thought that more studies are required.
References
1. Zhu QD, Tao CL, Zhou MT, Yu ZP, Shi HQ, Zhang QY. Primary closure versus T-tube drainage after common bile duct exploration for choledocholithiasis. Langenbecks Arch Surg. 2011; 396:53–62. PMID: 20582601.

2. Keighley MR, Graham NG. Infective complications of choledochotomy with T-tube drainage. Br J Surg. 1971; 58:764–768. PMID: 4329041.

3. Park YK, Kim JC, Cho CK, Kim HJ. Bile peritonitis associated with biliary leakage after removal of T-tube from common bile duct. Korean J Hepatobiliary Pancreat Surg. 2000; 4:131–137.
4. Zhang WJ, Xu GF, Wu GZ, Li JM, Dong ZT, Mo XD. Laparoscopic exploration of common bile duct with primary closure versus T-tube drainage: a randomized clinical trial. J Surg Res. 2009; 157:e1–e5. PMID: 19577251.

5. Jameel M, Darmas B, Baker AL. Trend towards primary closure following laparoscopic exploration of the common bile duct. Ann R Coll Surg Engl. 2008; 90:29–35. PMID: 18201497.

6. Park IY, Sung GY, Song MH, Lee DS, Kim W, Won JM. Primary common bile duct closure and antegrade stent insertion in choledocholithiasis patients. Korean J Hepatobiliary Pancreat Surg. 2001; 5:65–71.
7. Tan KK, Shelat VG, Liau KH, Chan CY, Ho CK. Laparoscopic common bile duct exploration: our first 50 cases. Ann Acad Med Singapore. 2010; 39:136–142. PMID: 20237736.
8. Ambreen M, Shaikh AR, Jamal A, Qureshi JN, Dalwani AG, Memon MM. Primary closure versus T-tube drainage after open choledochotomy. Asian J Surg. 2009; 32:21–25. PMID: 19321398.

9. Seale AK, Ledet WP Jr. Primary common bile duct closure. Arch Surg. 1999; 134:22–24. PMID: 9927125.

10. So BJ, Chae KM, Ann HS. Primary colosure of T-tube drainage after choledochotomy. J Korean Surg Soc. 1994; 46:107–113.
11. Humar A, Barron PT, Sekar AS, Lum A. Pancreatitis and duodenal perforation as complications of an endoscopically placed biliary stent. Gastrointest Endosc. 1994; 40:365–366. PMID: 8056245.

12. Lenzo NP, Garas G. Biliary stent migration with colonic diverticular perforation. Gastrointest Endosc. 1998; 47:543–544. PMID: 9647386.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download