Abstract
This study aimed to elicit the variability of appetite and food intake patterns in female college students during different menstrual phases. The craving for certain foods and physiological and psychological symptoms of menstrual phase (pre- and post-menstrual) were investigated by self-administered questionnaire. Three hundred and sixty six students who were 20.9 years old and had 19.8 kg/m2 of BMI volunteered to participate in this study. Most of the subjects (89.5%) experienced the premenstrual syndrome (PMS) such as irritation, bodily fatigue, nervosity. Symptoms such as tiredness, stomachache, changes in taste and increased appetite were pointed out to be experienced at the onset of the menstrual cycle. The variability of food intake in premenstrual phase, 11.0% of subjects had decreased food intake where as 68.8% had experienced increased intake. The postmenstrual phase, 20.1% had decreased food intake while 45.2% had experienced increased intake due to changes in the appetite. Before starting menstruation, most of the subjects craved for sweets. The group who had experienced abnormal appetite during menstrual phase was significantly high ratio in overweight and obese students (p < 0.05). We also observed an association between the PMS score and the variability of eating patterns during the menstrual phase. The students who experienced changing appetite and food intake had significantly high PMS score in the premenstrual phase (p < 0.01) and postmenstrual phase (p < 0.05). These results suggested a need for future study related to changes in the actual nutrient intake and activity level during the menstrual phase.
Figures and Tables
Fig. 1
The premenstrual syndrome (PMS) scores
1) Average score (0; points for strongly disagree, 1; points for disagree, 2; points for neutral, 3; points for agree, 4; points for strongly agree)
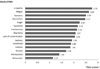
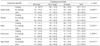
Table 3
Self-evaluated body image, menstrual regularity and the variability of food intake according to BMI

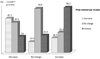
Table 4
Comparison of the sleeping time and premenstrual syndrome (PMS) score by the degree of dietary intakes in menstrual cycle

References
1. Fong AK, Kretsch MJ. Change in dietary intake, urinary nitrogen, and urinary volume across the menstrual cycle. Am J Clin Nutr. 1993; 57(1):43–46.
2. Blaustein JD, Wadi GN. Ovarian influences on the meal patterns of female rats. Physiol Behav. 1976; 17(2):201–208.
3. Buffenstein R, Poppitt SD, McDevitt RM, Prentice AM. Food intake and the menstrual cycle: A retrospective analysis, with implications for appetite research. Physiol Behav. 1995; 58(6):1067–1077.
4. Choi JW. Relationship among premenstrual syndrome, dietary behavior, stress, and depression of female adults. Sungsin University;2013. MS Thesis.
5. Chon MY, Jeon HW, Kim MH. Bone Mineral density and factors influencing bone mineral density in college women. Korean J Women Health Nurs. 2012; 18(3):190–199.
6. Cross GB, Marley J, Miles H, Willson K. Changes in nutrient intake during the menstrual cycle of overweight women with premenstrual syndrome. Brit J Nutr. 2001; 85:475–482.
7. Czaja JA, Goy RW. Ovarian hormones and food intake infemale guinea pigs and rhesus monkeys. Horm Behav. 1975; 6(4):329–349.
8. Dalvit-McPhillips SP. The effect of the human menstrual cycle on nutrient intake. Physiol Behav. 1983; 31(2):209–212.
9. Dalvit SP. The effect of the menstrual cycle on patterns of food intake. Am J Clin Nutr. 1981; 34(9):1811–1815.
10. Danker-Hopfe H, Roczen K, Löwenstein-Wagner U. Regulation of food intake during the menstrual cycle. Anthropol Anz. 1995; 53(3):231–238.
11. Davidsen L, Vistisen B, Astrup A. Impact of the menstrual cycle on determinants of energy balance : a putative role in weight loss attempts. Int J Obes (Lond). 2007; 31(12):1777–1785.
12. Dye L, Blundell JE. Menstrual cycle and appetite control:implications for weight regulation. Hum Reprod. 1997; 12(6):1142–1151.
13. Gentry RT, Wade GN, Roy EJ. Individual differences in estradiol-induced behaviors and in neuronal H-estradiol uptake in rats. Physiol Behav. 1976; 17(2):195–200.
14. Frye CA, Crystal S, Ward KD, Kanarek RB. Menstrual cycle and dietary restraint influence taste preferences in young women. Physiol Behav. 1994; 55(3):561–567.
15. Giannini AJ, Price WA, Loiselle RH, Giannini MC. Hyperphagia in premenstrual tension syndrome. J Clin Psychiatry. 1985; 46(10):436–437.
16. Ha KH. Perception and patterns for weight control of the female college students. Korean J Hum Ecol. 2005; 9(2):197–209.
17. Halbreich U, Endicott J, Schacht S, Nee J. The diversity of premenstrual changes as reflected in the premenstrual assessment form. Acta Psychiatr Scand. 1982; 65(1):46–65.
18. Hormes JM, Timko CA. All cravings are not created equal. Correlates of menstrual versus non-cyclic chocolate craving. Appetite. 2011; 57(1):1–5.
19. Jeong BS, Lee JH, Chang NS, Kang BN, Joe SH, Kim YC, Han OS. Treatment-seeking behaviors among Korean university women with premenstrual symptoms. Korean J Psychopharmacol. 2001; 12(3):201–210.
20. Jung HM, Kim YS. Factors affecting dysmenorrhea among adolescents. Korean J Child Health Nurs. 2004; 10(2):196–204.
21. Jung JH. Dietary behaviors and life style in high school female students with premenstrual syndrome. Sungsin University;2009. MS Thesis.
22. Piehowski KE, Preston AG, Miller DL, Nickols-Richardson SM. A reduced-calorie dietary pattern including a daily sweet smack promotes body weight reduction and body composition improvements in premenopausal women who are overweight and obese: a piot study. J Am Diet Assoc. 2011; 111(8):1198–1203.
23. Kim BS, Lee YE. The relationship of food behaviors with body Image and BMI of female college students in Jeonbuk province. Korean J Hum Ecol. 2000; 9(2):231–243.
24. Kim EH, Kim SJ. Pre-menstruation discomforts experienced by women. Korean J Women Health Nurs. 2001; 7(4):631–641.
25. Kim JW. Sleep pattern across the menstrual cycle phase in healthy women. Korea University;2003. Ph.D thesis.
26. Kim JY, Ahn HS. A Study of nutritional intakes, food preference and blood composition in female college students with premenstural syndrome. Korean J community Nutr. 2008; 13(4):565–572.
27. Kim YM, Jung MH. A Survey on premenstrual syndrom of female workers. J Korea Community Health Nurs Acad Soc. 1994; 8(1):53–56.
28. Lee IS. A study on the menstrual patterns and menstrual discomforts in women university students. J Korea Community Health Nurs Acad Soc. 1998; 12(1):116–131.
29. Lim HS, Park YS. Differences in dietary intake and life-style of female college students in Seoul with and without premenstrual syndrome. J Korean Soc Menopause. 2010; 16(3):153–161.
30. Lovejoy JC, Champagne CM, Donge LD, Xie H, Smith SR. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes (Lond). 2008; 32(6):949–958.
31. McNair DM, Frankenthaler ML, Czerlinsky T, White TW, Sasson S, Fisher S. Simulated public speaking as a model of clinical anxiety. Psychopharmacology (Berl). 1982; 77(1):7–10.
32. Manocha S, Choudhuri G, Tandon BN. A study of dietary intake in pre-and post-menstrual period. Hum Nutr Appl Nutr. 1986; 40(3):213–216.
33. Martini MC, Lampe JW, Slavin JL, Kurzer MS. Effect of the menstrual cycle on energy and nutrient intake. Am J Clin Nutr. 1994; 60(6):895–899.
34. McNeil J, Doucet E. Possible factors for altered energy balance across the menstrual cycle: a closer look at the severity of PMS, reward driven behaviors and leptin variations. Eur J Obstet Gynecol Reprod Biol. 2012; 163(1):5–10.
35. Steiner M. Premenstural syndrome and premenstrual dysphoric disorder: Guidlines for management. J Psychiatry Neurosci. 2000; 25(5):459–468.
36. Moon HJ. A Study on dietary attitudes and body composition by menstrual cycle in female college students of Yeosu area. Yeosu University;2005. MS Thesis.
37. Park JY. The BMI, body image recognition, and weight control behavior of female college students. J Korean Acad Fundam Nurs. 2011; 18(4):444–451.
38. Park KE, Lee SE. A study on premenstrual syndrome and menstrual attitude. Korean J Women Health Nurs. 2001; 7(3):359–372.
39. Sung MJ, Chang KJ. Correlations among life stress, dietary behaviors and food choice of college students. J East Asian Soc Diet Life. 2006; 16(6):655–662.
40. Seo IJ, Doo KJ. A study on the relationship between study and leisure time according to the sleeping time of university students. In : Proceedings of 2010 Symposium of the Korean Home Management Association; 2010. p. 329.
41. The Korean Nutrition Society. Dietary reference intakes for Koreans. Seoul: 2010.
42. Tarasuk V, Beaton GH. Menstrual-cycle patterns in energy and macronutrient intake. Am J Clin Nutr. 1991; 53(2):442–447.
43. Wade GN. Gonadal hormones and behavioral regulation of body weight. Physiol Behav. 1972; 8(3):523–534.
44. Yang HY, Byun YS. Weight control behavior in women college students and factors influencing behavior. J Korean Acad Fundam Nurs. 2012; 19(2):190–200.
45. Yen JY, Chang SJ, Ko CH, Yen CF, Chen CS, Yeh YC, Chen CC. The high-sweet-fat food craving among women with premenstrual dysphoric disorder:Emotional response, implicit attitude and rewards sensitivity. Psychoneuroendocrinology. 2010; 35(8):1203–1212.
46. Yom YH, Lee KE. Factors affecting eating attitude of female undergraduates in regard to BMI. J Korean Acad Nurs. 2010; 40(5):676–685.
47. Yonkers KA. Premenstrual syndrome. Lancet. 2008; 371:1200–1210.
48. Ziomkiewicz A, Pawlowski B, Ellison PT, Lipson SF, Thune I, Jasienska G. Higher luteal progesterone is associated with low levels of premenstrual aggressive behavior and fatigue. Biol Psychol. 2012; 91(3):376–382.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download