Abstract
Background
Previous antibiotic exposure may inhibit the growth of microorganisms in blood culture bottles. The authors investigated the frequency of previous antibiotic usage and analyzed the relationships among antibiotic usage, microbiological culture results and mortality of sepsis patients.
Methods
From April to May 2011, all blood cultures requested from inpatients were analyzed according to the admitted ward and antibiotic prescription records. The BacT/Alert 3D system (bioMerieux Inc.) was used with a standard bottle (SA, SN) for blood culture.
Results
Of 900 inpatients, 48% had been receiving antimicrobial agents when blood cultures were ordered. This group had a significantly higher mortality rate (36.2%) compared to the patients who had not received antibiotics (11.1%). Gram-negative rod bacteremia (37.1%) and candidemia (100%) resulted in a significantly higher mortality rate compared to Gram-positive cocci bacteremia (16.4%). In the analysis of 21 cases resulting in death, 15 (71.4%) patients died before or on the date when blood culture results were reported.
Blood stream infections (BSIs) are common and often fatal. Blood culture is essential for isolating the etiological agents of sepsis and for improving the treatment outcomes of BSIs. There are several important guidelines for the optimal use of blood cultures, such as blood culture set numbers, blood collection timing, blood volume, and skin disinfection [1,2]. In addition, antibiotics should be delayed until blood is collected from patients with sepsis [1,3]. When patients are diagnosed with hematological malignancies or solid organ tumors, they are prone to developing sepsis due to prolonged neutropenia [4]. Other immunologically compromised hosts, such as patients who have undergone transplantation, steroid therapy, AIDS, multiple organ failures, trauma, burn, or surgery, may be susceptible to bacteremia or fungemia [5]. Antibiotics may be used prophylactically for these patients to prevent sepsis. Studies on the previous antibiotic usage on blood culture results are rare in Korea. We investigated the frequency of antibiotic usage before blood culture was performed in inpatients and the effect of this usage on blood culture results.
Gram-negative rod (GNR) bacteremia, especially bacteremia due to pseudomonas, is known to be more fatal than gram-positive cocci (GPC) bacteremia [4,6], although the latter is becoming more common because many medical devices inserted into the skin or mucous membranes have been more widely used [5,7-9]. We investigated mortality according to previous antibiotic prescriptions and microbiological results. Cases that resulted in death were reviewed to determine the risk factors for mortality.
During April-May, 2011, consecutive blood cultures requested from inpatients, except in the Department of Emergency, were retrospectively analyzed, because drug usage information was not available to obtain in most of the cases visiting the Department of Emergency. All blood cultures regardless of repeated request were included during the study period. Our institution is a university-affiliated teaching hospital with 850 hospital beds. Patients were divided into two groups: antibioticexposed vs. non-exposed. The proportion of antibiotics administered was analyzed by each ward. The types of antibiotics prescribed were retrieved using a drug information system.
For blood cultures, the BacT/Alert 3D system (bioMerieux Inc., Durham, NC) was used with standard bottle (SA, SN), which does not contain charcoal or resin. In general, a blood culture was performed for 2 sets with 10 mL of blood for each collection. Povidone iodine was mainly used for skin disinfection. Blood culture bottles were incubated for 5 days in the equipment. When there was a positive signal in the blood culture equipment, the bottle was subjected to Gram staining, and its result was reported as soon as possible (preferably within an hour) to the attending physician by short message service (SMS). A small aliquot was cultured on a blood agar plate and a MacConkey agar plate and then incubated overnight at 35℃. The colonies were used for identification and susceptibility testing using a Vitek system (bioMeriux Inc.). Microbiological data were analyzed according to the patient's history of antibiotic exposure.
During the study period, there were 21 cases that resulted in death. Mortality was compared according to antibiotic exposure history and the microbiological identification results. Underlying illnesses, neutrophil count, antibiotics administered, and blood culture isolates were reviewed for all death cases.
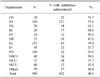
The rate of antibiotic prescriptions at the time of blood culture was 48.0% among 900 admitted patients during the study period. The prescription rate before blood culture was higher in the MICU (medical intensive care unit) (90.0%), SICU (surgical intensive care unit) (75.7%), Departments of Surgery (91.7%), Hematology (75.6%), and Neurosurgery (63.3%), whereas it was lower in the NICU (neonatal intensive care unit) (15.0%), Departments of Pediatrics (24.9%), Pulmonology (33.7%), and Gastroenterology (40.4%) (Table 1).
A total of 1,096 antibiotics were prescribed for 432 patients. The mean number of antibiotics per patient was 2.5. Cephalosporins (31.1%) were the most commonly prescribed followed by penicillins (16.2%), quinolones (14.1%), antifungal agents (8.5%), metronidazole (5.9%), and vancomycin (5.5%). Among 432 patients, 26.6% were prescribed ciprofloxacin, 23.8% piperacillin/tazobactam, 23.2% ceftriaxone, 15.7% fluconazole, and 13.9% vancomycin (data not shown).
Among 432 patients receiving antibiotics, 47 (10.9%) indicated bacteremia or candidemia. The most frequently isolated pathogens were S. aureus (9 episodes), Enterococcus faecium (8 episodes), Escherichia coli (8 episodes), Klebsiella pneumoniae (6 episodes), and Candida albicans (4 episodes) (Table 2). Among 468 patients not receiving antibiotics, 36 (7.7%) presented with bacteremia (P<0.05). S. aureus was predominantly isolated (8 episodes) in this group, followed by coagulase-negative staphylococci (CoNS, 6 episodes) and Staphylococcus epidermidis (5 episodes). Nine and 4 patients presented with polymicrobial infections in the group that received antibiotics and the group that did not receive antibiotics, respectively. The mortality of sepsis with GNR was 37.5% (9/24) compared to 26.9% (7/27) of sepsis with GPC in the group receiving antibiotics; the mortality of sepsis with GNR was 36.4% (4/11) and that with GPC was 7.1% (2/28) in the group that did not receive antibiotics. Taken together, the mortality rate with GNR (37.1%) was significantly higher than that with GPC (16.4%) (P<0.05). All five cases with candidemia died.
Seventeen (36.2%) of the 47 patients who had previous antibiotics before blood culture died compared to only 4 (11.1%) patients in the group that did not receive antibiotics (P<0.05, Table 2). Among 21 patients who died due to sepsis during the study period, 17 were over 50 years old (Table 3). There was no preponderance of gender (M=13). Ten had an underlying solid tumor, and 2 had acute leukemia. Eleven patients had neutrophil counts of >10,000/µL, whereas only 3 had counts of <500/µL. Among 5 patients with candidemia, 4 had neutrophil counts >10,000/µL. Multiple combination therapy had been prescribed except in 3 cases. Four patients presented with polymicrobial infections. From the 13 types of bacteria available for antibiotic susceptibility testing, 8 were resistant, and 5 were susceptible to currently used antibiotics (data not shown). Among 5 patients with candidemia, 4 had not used antifungal agents at the time of blood culture. Importantly, fifteen (71.4%) patients died either before or on the date that blood culture results were reported.
The main purposes of this study were to understand how many patients had received antibiotics before blood culture, and how mortality varied according to antibiotic usage and microbiological culture results. Demographics, diagnoses, neutrophil counts, previous antibiotic usage, and isolated pathogens were analyzed for the cases resulting in death. Approximately half of the inpatients had received antimicrobial therapy prior to blood culture, which was more common in the MICU, SICU, and surgical departments (Table 1). Ciprofloxacin, piperacillin/tazobactam, ceftriaxone, cefotaxime, fluconazole, and vancomycin were most commonly used. Approximately 40% of patients had recent antibiotic exposure, and cefepime (50%) and ciprofloxacin (33%) were the most common agents that patients were previously exposed to in the study of GNR severe sepsis [6]. Even in the patients receiving antibiotics, a blood culture using a standard bottle type gave a relatively favorable positive rate (10.9%), which was higher than that in the patients not receiving antibiotics (7.7%). This result went against expectation because antibiotics may suppress the growth of bacteria. The main reason for the higher prevalence of bacteremia in the group of patients receiving antibiotics may be due to the severity of disease. This group may have more severe illnesses than the group of patients not receiving antibiotics. In contrast, in a study on hematological malignancies and high-risk neutropenia, the positive rate of blood culture was 7% in patients receiving antibiotics compared to 14.3% in patients not receiving antibiotics [8]. Recently, GPC bacteremia has increased because central and peripheral catheters have been widely used in inpatients [5,10]. Our data showed a similar result: GNR bacteremia was present in 35 patients vs. GPC bacteremia in 55 patients (Table 2). Data on a higher mortality rate in patients recently exposed to antibiotics (51% vs. 34%) [6] were in accordance with our data (36.2% vs. 11.1%). GNR bacteremia, especially bacteremia due to pseudomonas, is known to be more fatal than GPC bacteremia [3,6]. GNR bacteremia showed a significantly higher mortality rate than GPC bacteremia (37.1% vs. 16.4%). All cases of GNR bacteremia should be regarded as true bacteremia, whereas it is difficult to interpret the cases of GPC bacteremia, especially when it comes to S. epidermidis, CoNS, or S. viridans [6,9-11].
Although we did not review all medical records, an underlying malignancy seemed to be the most important factor that determined the mortality of sepsis. This finding may be due to either the malignancy itself or an immunocompromised status, such as sustained neutropenia [4]. Among 21 death cases, twelve had either solid organ tumors or acute leukemia. Unexpectedly, absolute neutropenia (<500/µL) was observed only in 3 patients, whereas the majority of patients, including patients with candidemia, showed marked neutrophilia. Candidemia should be suspected even in cases of severe neutrophilia [3]. Eight patients had received antibiotics that were resistant to the etiological pathogen. Five patients died even though they had received antibiotics susceptible to the isolated pathogen. This phenomenon is called breakthrough bacteremia. An inadequate concentration of antibiotics, poor drainage of a focus of infection, or impairment of host defenses may play a role in breakthrough bacteremia [2]. One patient showed breakthrough candidemia. Breakthrough bacteremia was detected in 6% of episodes of bacteremia in Spain [6], whereas it was detected in 10.6% (5/47) of episodes of bacteremia in our study.
The presence of polymicrobial infections does not seem to be a major risk factor for mortality. Five (23.5%) of the 21 patients who died presented with polymicrobial infections. Another 8 cases with polymicrobial infections survived. Importantly, all patients with candidemia died, suggesting a very low immunological status in these patients. Physicians should be more alert when repored for GNR bacteremia or fungemia because mortalities are much higher in these cases [10]. Surprisingly, most (71.4%) of the patients died before or on the date of the blood culture results reported which suggests a very rapid progression of sepsis and requires a more accurate and rapid blood culture procedure. A more keen evaluation of the patients' conditions and standardized empirical therapeutic intervention are mandatory. Use of an automated continuous monitoring blood culture system will reveal bacteria in the blood culture bottle more rapidly than a manual method. More than 70% of the blood culture will give a positive result within a day when using an automated blood culture system [12]. Optimal procedures, such as sufficient blood volume collection or thorough skin decontamination, will improve the quality of the blood culture [2,11]. In a recent report, only 45% of cases had an adequate number of blood cultures, and an optimal volume of blood (≥10 mL per bottle) was inoculated in 13% of adult bottles [13]. The critical value of the Gram stain in a positive signal bottle should be reported to the attending medical personnel directly within an hour [1]. As it takes 2 more days to obtain the identification and susceptibility test results, the urgent reporting of Gram stain results cannot be overemphasized [1,2]. Patient categorization (e.g., community-acquired, nosocomial, or infections in hematological units) combined with Gram stain data could be useful for determining empirical therapy [14]. Resin- or charcoal-containing media are recommended for patients receiving antibiotics because they may inhibit the effect of antibiotics in the blood culture bottle and enhance the growth of microorganisms [1,2,15].
In conclusion, approximately half of the inpatients had already been receiving antimicrobial agents when the blood cultures were ordered. Notably, the patients that had received antibiotics gave a higher positive rate compared to the patients that had not received antibiotics. GNR bacteremia and candidemia were more fatal than GPC bacteremia. As many patients died before blood culture results were reported, adequate blood culture procedure and direct reporting of Gram stain results should be emphasized.
Figures and Tables
Table 1
Frequency of antibiotic administration by each department before blood culture was performed
ACKNOWLEDGMENTS
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2011-0008757).
References
1. CLSI. Principles and procedures for blood cultures; approved guideline. CLSI document M47-A. 2007. 2007. Wayne, PA: Clinical and Laboratory Standards Institute.
2. Baron EJ, Weinstein MP, Dunne WM Jr, Yagupsky P, Welch DF, Wilson DM. Baron EJ, editor. Cumitech 1C, blood cultures IV. 2005. Washington, D.C: ASM Press.
3. Anatoliotaki M, Valatas V, Mantadakis E, Apostolakou H, Mavroudis D, Georgoulias V, et al. Bloodstream infections in patients with solid tumors: associated factors, microbial spectrum and outcome. Infection. 2004. 32:65–71.
4. Rolston KV. The Infectious Diseases Society of America 2002 guidelines for the use of antimicrobial agents in patients with cancer and neutropenia: salient features and comments. Clin Infect Dis. 2004. 39:Suppl 1. S44–S48.
5. López Dupla M, Martinez JA, Vidal F, Almela M, López J, Marco F, et al. Clinical characterization of breakthrough bacteraemia: a survey of 392 episodes. J Intern Med. 2005. 258:172–180.
6. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003. 348:1546–1554.
7. Gaynes R, Edwards JR. National Nosocomial Infections Surveillance System. Overview of nosocomial infections caused by gram-negative bacilli. Clin Infect Dis. 2005. 41:848–854.
8. Hummel M, Warga C, Hof H, Hehlmann R, Buchheidt D. Diagnostic yield of blood cultures from antibiotic-na�ve and antibiotically treated patients with haematological malignancies and high-risk neutropenia. Scand J Infect Dis. 2009. 41:650–655.
9. Johnson MT, Reichley R, Hoppe-Bauer J, Dunne WM, Micek S, Kollef M. Impact of previous antibiotic therapy on outcome of Gram-negative severe sepsis. Crit Care Med. 2011. 39:1859–1865.
10. Sepkowitz KA. Treatment of patients with hematologic neoplasm, fever, and neutropenia. Clin Infect Dis. 2005. 40:Suppl 4. S253–S256.
11. Hall KK, Lyman JA. Updated review of blood culture contamination. Clin Microbiol Rev. 2006. 19:788–802.
12. Park SH, Shim H, Yoon NS, Kim MN. Clinical relevance of time-to-positivity in BACTEC9240 blood culture system. Korean J Lab Med. 2010. 30:276–283.
13. Vitrat-Hincky V, François P, Labarère J, Recule C, Stahl JP, Pavese P. Appropriateness of blood culture testing parameters in routine practice. Results from a cross-sectional study. Eur J Clin Microbiol Infect Dis. 2011. 30:533–539.
14. Hautala T, Syrjälä H, Lehtinen V, Kauma H, Kauppila J, Kujala P, et al. Blood culture Gram stain and clinical categorization based empirical antimicrobial therapy of bloodstream infection. Int J Antimicrob Agents. 2005. 25:329–333.
15. McDonald LC, Fune J, Gaido LB, Weinstein MP, Reimer LG, Flynn TM, et al. Clinical importance of increased sensitivity of BacT/Alert FAN aerobic and anaerobic blood culture bottles. J Clin Microbiol. 1996. 34:2180–2184.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download