Abstract
Background
Catheter-related bloodstream infection (CRBSI) is one of the leading types of infection, with a significant morbidity and mortality rate. We evaluated the differential time to positivity (DTP) and semi-quantitative culture of catheter segments (SQCC) as a method for diagnosing CRBSI.
Methods
From January 2010 to August 2011, 155 positive paired blood cultures which had the same organism isolated from blood cultures drawn simultaneously through the central venous catheter (CVC) and the peripheral vein were included. Positive DTP represents a DTP of least 120 min earlier for the time to detection of CVC draw than that of a peripheral vein draw. We evaluated the clinical utility of DTP and SQCC for diagnosing CRBSIs, which were further divided into two groups: confirmed (either by DTP or SQCC) and non-confirmed CRBSIs (neither DTP nor SQCC positive).
Results
Sixty-five percent (100/155) of episodes were confirmed to CRBSIs. In CRBSIs, Gram-positive cocci accounted for 61% of cases, non-fermenting Gram-negative bacilli represented 10%, Enterobacteriaceae for 10%, yeasts for 15%, and others for 4%. Among the confirmed CRBSI cases, 22 were both positive with DTP and SQCC, 30 cases were positive with DTP only, 12 cases were positive with SQCC only, and 36 cases which did not undergo SQCC analysis were DTP positive. The sensitivities of the DTP and SQCC techniques were 88.0% (88/100) and 53.1% (34/64), respectively.
Figures and Tables
Table 1
Causative microorganisms distribution between confirmed and non-confirmed cathetcr-relwted blood stteam tufections episodes
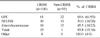
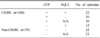
Table 2
Differential time to positivity according to microorganisms isolated from positive paired blood cultures

References
1. Chen WT, Liu TM, Wu SH, Tan TD, Tseng HC, Shih CC. Improving diagnosis of central venous catheter-related bloodstream infection by using differential time to positivity as a hospital-wide approach at a cancer hospital. J Infect. 2009. 59:317–323.
2. Shukrallah B, Hanna H, Hachem R, Ghannam D, Chatzinikolaou I, Raad I. Correlation between early clinical response after catheter removal and diagnosis of catheter-related bloodstream infection. Diagn Microbiol Infect Dis. 2007. 58:453–457.
3. Widmer AF, Nettleman M, Flint K, Wenzel RP. The clinical impact of culturing central venous catheters. A prospective study. Arch Intern Med. 1992. 152:1299–1302.
4. Capdevila JA, Planes AM, Palomar M, Gasser I, Almirante B, Pahissa A, et al. Value of differential quantitative blood cultures in the diagnosis of catheter-related sepsis. Eur J Clin Microbiol Infect Dis. 1992. 11:403–407.
5. Blot F, Nitenberg G, Chachaty E, Raynard B, Germann N, Antoun S, et al. Diagnosis of catheter-related bacteraemia: a prospective comparison of the time to positivity of hub-blood versus peripheral-blood cultures. Lancet. 1999. 354:1071–1077.
6. Blot F, Schmidt E, Nitenberg G, Tancréde C, Leclercq B, Laplanche A, et al. Earlier positivity of central-venous- versus peripheral-blood cultures is highly predictive of catheter-related sepsis. J Clin Microbiol. 1998. 36:105–109.
7. Raad I, Hanna HA, Alakech B, Chatzinikolaou I, Johnson MM, Tarrand J. Differential time to positivity: a useful method for diagnosing catheter-related bloodstream infections. Ann Intern Med. 2004. 140:18–25.
8. Khatib R, Riederer K, Saeed S, Johnson LB, Fakih MG, Sharma M, et al. Time to positivity in Staphylococcus aureus bacteremia: possible correlation with the source and outcome of infection. Clin Infect Dis. 2005. 41:594–598.
9. Marra AR, Edmond MB, Forbes BA, Wenzel RP, Bearman GM. Time to blood culture positivity as a predictor of clinical outcome of Staphylococcus aureus bloodstream infection. J Clin Microbiol. 2006. 44:1342–1346.
10. Martínez JA, Soto S, Fabrega A, Almela M, Mensa J, Soriano A, et al. Relationship of phylogenetic background, biofilm production, and time to detection of growth in blood culture vials with clinical variables and prognosis associated with Escherichia coli bacteremia. J Clin Microbiol. 2006. 44:1468–1474.
11. Martínez JA, Pozo L, Almela M, Marco F, Soriano A, López F, et al. Microbial and clinical determinants of time-to-positivity in patients with bacteraemia. Clin Microbiol Infect. 2007. 13:709–716.
12. Mermel LA, Farr BM, Sherertz RJ, Raad II, O'Grady N, Harris JS, et al. Guidelines for the management of intravascular catheter-related infections. Clin Infect Dis. 2001. 32:1249–1272.
13. Maki DG, Weise CE, Sarafin HW. A semiquantitative culture method for identifying intravenous-catheter-related infection. N Engl J Med. 1977. 296:1305–1309.
14. Raad I, Hanna H, Maki D. Intravascular catheter-related infections: advances in diagnosis, prevention, and management. Lancet Infect Dis. 2007. 7:645–657.
15. Park SH, Shim H, Yoon NS, Kim MN. Clinical relevance of time-to-positivity in BACTEC9240 blood culture system. Korean J Lab Med. 2010. 30:276–283.
16. Wilcox TA. Catheter-related bloodstream infections. Semin Intervent Radiol. 2009. 26:139–143.
17. O'Grady NP, Chertow DS. Managing bloodstream infections in patients who have short-term central venous catheters. Cleve Clin J Med. 2011. 78:10–17.
18. Maya ID, Carlton D, Estrada E, Allon M. Treatment of dialysis catheter-related Staphylococcus aureus bacteremia with an antibiotic lock: a quality improvement report. Am J Kidney Dis. 2007. 50:289–295.
19. Nguyen MH, Peacock JE Jr, Tanner DC, Morris AJ, Nguyen ML, Snydman DR, et al. Therapeutic approaches in patients with candidemia. Evaluation in a multicenter, prospective, observational study. Arch Intern Med. 1995. 155:2429–2435.
20. Raad I, Hanna H, Boktour M, Girgawy E, Danawi H, Mardani M, et al. Management of central venous catheters in patients with cancer and candidemia. Clin Infect Dis. 2004. 38:1119–1127.
21. James MT, Conley J, Tonelli M, Manns BJ, MacRae J, Hemmelgarn BR. Meta-analysis: antibiotics for prophylaxis against hemodialysis catheter-related infections. Ann Intern Med. 2008. 148:596–605.
22. Jaffer Y, Selby NM, Taal MW, Fluck RJ, McIntyre CW. A meta-analysis of hemodialysis catheter locking solutions in the prevention of catheter-related infection. Am J Kidney Dis. 2008. 51:233–241.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download