Abstract
Purpose
The purpose of this study is to evaluate the clinical and radiologic results of plate fixation in the Vancouver B1 and C periprosthetic femoral fracture (PFF).
Materials and Methods
Twenty patients who had sustained a Vancouver type B1 and C periprosthetic fracture after hip arthroplasty (years 2002-2012) were identified. The mean age was 66.0 years (range, 43-85 years) and the mean follow-up duration of the group was 38 months (range, 12-102 months). The dynamic compression plate (DCP) group included 12 patients and the locking compression plate (LCP) group included eight patients. Harris hip score (HHS) and walking ability, knee joint range of motion (ROM) were compared before injury and last follow-up. Fracture union rate and period were compared.
Results
The mean HHS score was 90.7 (64-96). There was no statistical difference between the two groups. At the last follow-up, knee joint ROM was 103.3° (105°-140°) in the DCP group and 118.4° (110°-140°) in the LCP group, showing good results in the LCP group (p=0.043). No significant difference in the fracture union rate and union periods was observed between the two groups.
Figures and Tables
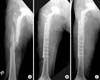 | Fig. 1A 46-year-old male patient with a Vancouver type B1 periprosthetic fracture treated with open reduction and internal fixation dynamic compression plate and screws. (A) Preoperative radiograph. (B) Immediate postoperative radiograph. (C) Postoperative 3-year plain radiograph. |
 | Fig. 2A 72-year-old male patient with a Vancouver type C periprosthetic fracture treated with open reduction and internal fixation locking compression plate and screws. (A) Preoperative radiograph. (B) Immediate postoperative radiograph. (C) Postoperative 1-year plain radiograph. |
Table 1
Demographic Data of the Two Groups

Table 2
Clinical Outcomes of the Two Groups

References
1. Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005; 20:857–865.
2. Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999; 30:183–190.
3. Garbuz DS, Masri BA, Duncan CP. Periprosthetic fractures of the femur: principles of prevention and management. Instr Course Lect. 1998; 47:237–242.
4. Pike J, Davidson D, Garbuz D, Duncan CP, O'Brien PJ, Masri BA. Principles of treatment for periprosthetic femoral shaft fractures around well-fixed total hip arthroplasty. J Am Acad Orthop Surg. 2009; 17:677–688.

5. Giannoudis PV, Kanakaris NK, Tsiridis E. Principles of internal fixation and selection of implants for periprosthetic femoral fractures. Injury. 2007; 38:669–687.

6. Brady OH, Garbuz DS, Masri BA, Duncan CP. Classification of the hip. Orthop Clin North Am. 1999; 30:215–220.

7. Brady OH, Garbuz DS, Masri BA, Duncan CP. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000; 15:59–62.

8. Masri BA, Meek RM, Duncan CP. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res. 2004; (420):80–95.

9. Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003; 34:Suppl 2. B63–B76.

10. Plecko M, Kraus A. Internal fixation of proximal humerus fractures using the locking proximal humerus plate. Oper Orthop Traumatol. 2005; 17:25–50.
11. Ricci WM, Bolhofner BR, Loftus T, Cox C, Mitchell S, Borrelli J Jr. Indirect reduction and plate fixation, without grafting, for periprosthetic femoral shaft fractures about a stable intramedullary implant. J Bone Joint Surg Am. 2005; 87:2240–2245.

12. McElfresh EC, Coventry MB. Femoral and pelvic fractures after total hip arthroplasty. J Bone Joint Surg Am. 1974; 56:483–492.

13. Nilsdotter A, Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res (Hoboken). 2011; 63:Suppl 11. S200–S2007.
14. Ogden WS, Rendall J. Fractures beneath hip prosthesis: a special indication for parham bands and plating. Orthop Trans. 1978; 2:70.
15. Kim KS, Chung YY, Ryu SW, Choi CH, Jung HG. Management of ipsilateral femoral fracture after hip arthroplasty. J Korean Orthop Assoc. 1997; 32:1575–1583.

16. Lindahl H, Oden A, Garellick G, Malchau H. The excess mortality due to periprosthetic femur fracture. A study from the Swedish National Hip Arthroplasty Register. Bone. 2007; 40:1294–1298.

17. Johansson JE, McBroom R, Barrington TW, Hunter GA. Fracture of the ipsilateral femur in patients wih total hip replacement. J Bone Joint Surg Am. 1981; 63:1435–1442.

18. Chakravarthy J, Bansal R, Cooper J. Locking plate osteosynthesis for Vancouver type B1 and type C periprosthetic fractures of femur: a report on 12 patients. Injury. 2007; 38:725–733.

19. Muller ME, Allgower M, Schneider R, Willenegger H. Manual of internal fixation techniques recommended by the AO group. 2nd ed. New York: Springer-Verlag;1986.
20. Rüedi TP, Lüscher JN. Results after internal fixation of comminuted fractures of the femoral shaft with DC plates. Clin Orthop Relat Res. 1979; (138):74–76.
22. Ring D, Jupiter JB. Internal fixation of the humerus with locking compression plates. Tech Shoulder Elbow Surg. 2003; 4:169–174.

23. Ring D, Perey BH, Jupiter JB. The functional outcome of operative treatment of ununited fractures of the humeral diaphysis in older patients. J Bone Joint Surg Am. 1999; 81:177–190.

24. Cho TJ, Lee K, Oh CW, Park MS, Yoo WJ, Choi IH. Locking plate placement with unicortical screw fixation adjunctive to intramedullary rodding in long bones of patients with osteogenesis imperfecta. J Bone Joint Surg Am. 2015; 97:733–737.

25. Fulkerson E, Koval K, Preston CF, Iesaka K, Kummer FJ, Egol KA. Fixation of periprosthetic femoral shaft fractures associated with cemented femoral stems: a biomechanical comparison of locked plating and conventional cable plates. J Orthop Trauma. 2006; 20:89–93.

26. Graham SM, Moazen M, Leonidou A, Tsiridis E. Locking plate fixation for Vancouver B1 periprosthetic femoral fractures: a critical analysis of 135 cases. J Orthop Sci. 2013; 18:426–436.

27. Buttaro MA, Farfalli G, Paredes Núñez M, Comba F, Piccaluga F. Locking compression plate fixation of Vancouver type-B1 periprosthetic femoral fractures. J Bone Joint Surg Am. 2007; 89:1964–1969.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download