Abstract
Purpose
The aim of this study was to compare the results of the lateral entry pin technique and the crossed pin technique in treatment of Gartland type III humerus supracondylar fracture.
Materials and Methods
Seventeen patients (group I) underwent surgery using the lateral entry pin technique, and 33 patients (group II) underwent surgery using the crossed pin technique for Gartland type III humerus supracondylar fracture in Hanyang University Seoul Hospital between January 2011 and January 2014. Maintenance of reduction was compared between the 2 surgical techniques by measuring changes in Baumann angle and lateral humerocapitellar angle after surgery and after pin removal in groups I and II. In addition, the final carrying angle and level of loss of functional movement were measured for comparison of clinical results between the 2 groups. Occurrence of ulnar nerve palsy in the 2 groups was also examined.
Results
The mean Baumann angle and lateral humerocapitellar angle changes were 3.3° and 3.7 in group I and 3.1° and 3.4° in group II, respectively. No statistically significant differences were found between the 2 groups. Clinical results showed that the changes in the final carrying angle and range of motion were 2.9° and 2.6° in group I and 2.6° and 3.0° in group II, respectively, indicating no significant differences between the 2 groups. In terms of nerve damage, 1 patient in group II had temporary iatrogenic ulnar nerve palsy.
Figures and Tables
 | Fig. 1(A) A 4-year-old boy fell outstretched and sustained an extension type III supracondylar humerus fracture, as determined by preoperative anteroposterior (AP) and lateral radiographs. (B) Closed reduction and 2 lateral pin fixation was performed. The Baumann angle and lateral humerocapitellar angle were measured using postoperative AP and lateral radiographs. (C) The Baumann angle and lateral humerocapitellar angle were re-measured using AP and lateral radiographs obtained after pin removal. Difference was calculated using the changes in Baumann angle and lateral humercapitellar angle from after the operation to after pin removal. |
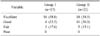
Table 1
Flynn's Criteria for Grading

Data from the article of Flynn et al. (J Bone Joint Surg Am 1974;56:263-272).14)
References
1. Cheng JC, Shen WY. Limb fracture pattern in different pediatric age groups: a study of 3,350 children. J Orthop Trauma. 1993; 7:15–22.
2. de las Heras J, Durán D, de la Cerda J, Romanillos O, Martínez-Miranda J, Rodríguez-Merchán EC. Supracondylar fractures of the humerus in children. Clin Orthop Relat Res. 2005; (432):57–64.
3. Farnsworth CL, Silva PD, Mubarak SJ. Etiology of supracondylar humerus fractures. J Pediatr Orthop. 1998; 18:38–42.

4. Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959; 109:145–154.
5. Kocher MS, Kasser JR, Waters PM, et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J Bone Joint Surg Am. 2007; 89:706–712.

6. Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am. 2008; 90:1121–1132.

7. Shoaib M, Sultan S, Sahibzada SA, Ali A. Percutaneous pinning in displaced supracondylar fracture of humerus in children. J Ayub Med Coll Abbottabad. 2004; 16:48–50.
8. Lee SS, Mahar AT, Miesen D, Newton PO. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. 2002; 22:440–443.

9. Zionts LE, McKellop HA, Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1994; 76:253–256.

10. Royce RO, Dutkowsky JP, Kasser JR, Rand FR. Neurologic complications after K-wire fixation of supracondylar humerus fractures in children. J Pediatr Orthop. 1991; 11:191–194.

11. Skaggs DL, Hale JM, Bassett J, Kaminsky C, Kay RM, Tolo VT. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J Bone Joint Surg Am. 2001; 83:735–740.

12. Lee YH, Lee SK, Kim BS, et al. Three lateral divergent or parallel pin fixations for the treatment of displaced supracondylar humerus fractures in children. J Pediatr Orthop. 2008; 28:417–422.

13. Topping RE, Blanco JS, Davis TJ. Clinical evaluation of crossed-pin versus lateral-pin fixation in displaced supracondylar humerus fractures. J Pediatr Orthop. 1995; 15:435–439.

14. Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children Sixteen years' experience with long-term follow-up. J Bone Joint Surg Am. 1974; 56:263–272.

15. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979; 86:420–428.

16. Celiker O, Pestilci FI, Tuzuner M. Supracondylar fractures of the humerus in children: analysis of the results in 142 patients. J Orthop Trauma. 1990; 4:265–269.

17. Mazda K, Boggione C, Fitoussi F, Penneçot GF. Systematic pinning of displaced extension-type supracondylar fractures of the humerus in children. A prospective study of 116 consecutive patients. J Bone Joint Surg Br. 2001; 83:888–893.
18. Oh CW, Park BC, Kim PT, Park IH, Kyung HS, Ihn JC. Completely displaced supracondylar humerus fractures in children: results of open reduction versus closed reduction. J Orthop Sci. 2003; 8:137–141.

19. Shim JS, Lee YS. Treatment of completely displaced supracondylar fracture of the humerus in children by crossfixation with three Kirschner wires. J Pediatr Orthop. 2002; 22:12–16.

20. Skaggs DL, Cluck MW, Mostofi A, Flynn JM, Kay RM. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg Am. 2004; 86:702–707.

21. Maity A, Saha D, Roy DS. A prospective randomised, controlled clinical trial comparing medial and lateral entry pinning with lateral entry pinning for percutaneous fixation of displaced extension type supracondylar fractures of the humerus in children. J Orthop Surg Res. 2012; 7:6.

22. Shamsuddin SA, Penafort R, Sharaf I. Crossed-pin versus lateral-pin fixation in pediatric supracondylar fractures. Med J Malaysia. 56:Suppl D. 2001; 38–44.
23. Brauer CA, Lee BM, Bae DS, Waters PM, Kocher MS. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. 2007; 27:181–186.

24. Zaltz I, Waters PM, Kasser JR. Ulnar nerve instability in children. J Pediatr Orthop. 1996; 16:567–569.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download