Abstract
In order to investigate the feasibility of a modified tension band combined with anti-gliding loop augmentation technique for the treatment of comminuted patellar fracture, 21 patients with comminuted patellar fracture were enrolled in this study. After the modified tension band wiring of patellar fracture, a cerclage wire was passed around the patella. Anti-gliding loops were made on the bending sites of Kirshner-wires. A knot was tied using both ends of the anti-gliding loops, and the cerclage wire was tightened using proximal knots. Bone union was achieved at 4.5±1.5 months postoperatively without nonunion. The Lysholm score was 87.1±2.8, and the range of motion of the knee was 2.1°±3.4° to 132.2°±6.5° at the last follow-up. The modified tension band combined with anti-gliding loop augmentation technique might be considered an alternative modification of modified tension band wiring for the treatment of comminuted patellar fracture.
Fracture of the patella accounts for approximately 0.5% to 1.5% of all skeletal injuries1). Surgical correction of patellar fracture is indicated when the integrity of the extension mechanism is affected or the fracture fragments are displaced due to traction of the quadriceps muscles3). Several surgical techniques for the treatment of patellar fracture have been used8), and the most popular fixation method is the AO modified tension band wiring technique involving the use of a tension band and two intramedullary Kirschner (K)-wires7). However, Smith et al.6) reported 20% of patellar fractures treated with the AO modified tension band technique were significantly displaced (2 mm) in the perioperative period. In addition, there have been reports on the postoperative complications related to migration of the K-wires leading to loss of rigid internal fixation4). Recently, various modifications of the technique have been suggested to overcome these complications2,9,10). We developed a novel modification method, 'anti-gliding loop augmentation technique', to improve the surgical outcome and avoid the complications of the modified tension band wiring used especially for the treatment of comminuted patellar fracture. The purpose of this study was to present the technical procedures and investigate the feasibility of this technique through clinical and radiographic evaluation.
This was a retrospective study of patients who underwent open reduction with internal fixation of patella using AO modified tension band combined with anti-gliding loop augmentation technique. The study population comprised 21 consecutive patients with comminuted patellar fracture from January 2007 to April 2011. Exclusion criteria included any history of surgery around knee joint on the affected limb, severe osteoporosis and concomitant other fracture around knee joint. The patients consisted of 16 men and 5 women. The mean age was 45 years (range, 25-57 years), mean body mass index was 27.4 (range, 20.9-32.2) and mean follow-up period was 18 months (range, 12-24 months). Radiographic and clinical parameters were evaluated at 6 weeks, 3, 6, 12 months postoperatively, and the last follow-up. Average union time was evaluated using clinical assessment and plain radiographs. Clinical parameters included time to 120° flexion of the knee joint, and the Lysholm score and range of motion at the last follow-up. The postoperative complications including slippage of K-wires were assessed. Implants were routinely removed on confirmation of adequate bony union with patients' consent in all cases at 12 months after surgery.
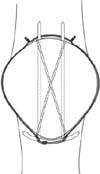
The patients were placed in a supine position on an operating table under spinal anesthesia if possible. A pneumatic tourniquet was routinely used. A standard midline longitudinal incision was made in the skin above the knee and the soft tissue was gently dissected. The fracture surface was exposed subperiosteally and the patellar fragments were reduced using a clamp. Fixation was achieved with longitudinal insertion of two K-wires in a parallel pattern and a steel wire (18 Fr. gauge) was wound around the proximal and distal ends of the K-wires in a figure-of-eight manner. After the modified tension band fixation was completed, a cerclage wire (19 Fr. gauge) for the anti-gliding loops was prepared with two proximal knots like a Mickey Mouse hat (Fig. 1). The cerclage wire was then passed around the soft tissue of the patella using a spinal needle (Fig. 2). Antigliding loops were made on the bending sites of K-wires at the lower pole of the patella (Fig. 3). After a knot was tied between both ends of the anti-gliding loops, the cerclage wire was tightened using the proximal knots while the knee was placed in full extension (Figs. 4, 5, 6, 7). Before the wound closure, full passive range of motion without any reduction loss or loosening of the fixation was confirmed. Postoperatively, the patients began active and passive knee range of motion exercises as early as possible. On postoperative day 3, protected partial weight-bearing was allowed. Protected crutch ambulation was recommended until the fracture healed. Bone union was defined based on the clinical and radiographic conditions as follows: spontaneous ability to walk without pain or tenderness and trabeculi evidently connecting both major fragments on plain radiographs9).
Bone union was achieved at 4.5±1.5 (mean±standard deviation) months postoperatively (range, 3-6 months). Postoperative complications including nonunion or migration of K-wires was not observed in any case. The time to 120° flexion of the knee joint was 12.3±3.1 postoperative days (range, 7-14 days). At the last follow-up, the Lysholm score was 87.1±2.8 (range, 82-92) and the range of motion of the knee joint was from 2.1°±3.4° to 132.2°±6.5°. The patients returned sports and recreational activities at 6 months after surgery without any limitation of activity afterwards.
The modified AO tension-band technique is a very effective and widely used technique for stabilizing patellar fracture. It is well known that the major advantage of the tension-band wiring is enhancement of early range of motion of the joint. Accordingly, a long period of immobilization is unnecessary and the functional outcome is usually satisfactory after the surgical treatment. However, there have been many reports on the postoperative complications related to this technique6). The common complications include migration of inserted K-wires, irritation symptoms due to a subcutaneous knot or bending sites of K-wires, and disruption of the fracture site. Among these complications, loosening and migration of K-wires can lead to loss of reduction and surprisingly many reports have pointed out this complication4,5).
There have been various modifications of the technique to avoid loosening and migration of K-wires2,9,10). Kinik et al.2) reported the self-locking tension band technique: the proximal ends of the K-wires are bent to form the loops that a cerclage wire can pass through. With this self-locking effect, the cerclage wire can lock the K-wires and prevent proximal migration of the K-wires. However, the main disadvantages of their method are difficulty in bending K-wires and the bulky loops of K-wires. In our early experience, we found that K-wires (0.062 inches) were too stiff to form the proximal loops effectively. In case of comminuted fracture, the fracture reduction sites were displaced during the bending procedure. In addition, the proximal loops were so prominent on the quadriceps mechanism that they caused subcutaneous irritation during range of motion exercise. Wu et al.9) reported a revised technique of the tension band wiring: K-wires are bent at the both poles of the patella and the ends of K-wires are reversed to face downward. With regard to the complication of this revised technique, they commented that skin may be irritated by the reversed ends of the K-wires. Yotsumoto et al.10) recommended their method using two metal ring pins and two braided polyblend sutures as an alternative to stainless steel wire for fixation of patellar fracture. This technique may be an ideal version of the tension band wiring. However, the cost effectiveness should be considered.
Compared with the recent modifications of tension band wiring technique reported in the literature, our method has several advantages: This method is relatively easy and cost effective. There are no bulky loops that may induce subcutaneous irritation or pain. The anti-gliding loops can hold K-wires and provide an additional force to maintain the fracture reduction as well.
The limitation of this study is the small number of cases. More clinical experience using our technique will be necessary to confirm the advantageous effect on prevention of the complications of the tension band wiring fixation. The modified tension band combined with anti-gliding loop augmentation technique might be an alternative modification of modified tension band wiring for the surgical treatment of comminuted patellar fracture.
Figures and Tables
 | Fig. 1A cerclage wire is prepared for the anti-gliding loops with proximal two knots like a Mickey Mouse hat. |
 | Fig. 4A knot is tied between both ends of the anti-gliding loops, and the cerclage wire is tightened using the proximal knots. |
 | Fig. 5Fluoroscopic image of modified tension band fixation and the tightened cerclage wire with anti-gliding loops. |
 | Fig. 6Intraoperative picture demonstrating modified tension band fixation and the tightened cerclage wire with anti-gliding loops. Dotted rectangular area demonstrating anti-gliding loops. |
 | Fig. 7Magnified picture of the dotted rectangular area of Fig. 6 demonstrating anti-gliding loops. |
References
1. Boström A. Fracture of the patella. A study of 422 patellar fractures. Acta Orthop Scand Suppl. 1972; 143:1–80.

2. Kinik H, Us AK, Mergen E. Self-locking tension band technique. A new perspective in tension band wiring. Arch Orthop Trauma Surg. 1999; 119:432–434.
3. Lotke PA, Ecker ML. Transverse fractures of the patella. Clin Orthop Relat Res. 1981; (158):180–184.

4. Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am. 1985; 67:1396–1401.

5. Murphy DF, Greene WB, Dameron TB Jr. Displaced olecranon fractures in adults. Clinical evaluation. Clin Orthop Relat Res. 1987; (224):215–223.

6. Smith ST, Cramer KE, Karges DE, Watson JT, Moed BR. Early complications in the operative treatment of patella fractures. J Orthop Trauma. 1997; 11:183–187.

7. Weber MJ, Janecki CJ, McLeod P, Nelson CL, Thompson JA. Efficacy of various forms of fixation of transverse fractures of the patella. J Bone Joint Surg Am. 1980; 62:215–220.

8. Wild M, Windolf J, Flohé S. Fractures of the patella. Unfallchirurg. 2010; 113:401–411.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download