Abstract
Purpose
To evaluate the clinical and radiological results of minimally invasive plate, osteosynthesis, using either a locking compression plate-distal tibia (LCP-DT) or Zimmer periarticular locking plate (ZPLP) for distal tibia fractures.
Materials and Methods
Fifty one patients (51 cases), who underwent minimally invasive osteosynthesis using locking compression plate for distal tibia fractures between October 2008 and August 2011, were followed for more than six months. Eighteen patients were treated with LCP-DT and 33 patients with ZPLP. Time to bony union and anatomic alignment were evaluated radiologically. Clinically, American Orthopedic Foot & Ankle Society ankle-hindfoot scales (AOFAS score) and range of ankle motion were assessed and compared between two groups.
Results
All patients achieved bony union at an average of 18 weeks on LCP-DT group and 16weeks on ZPLP group. The average American Orthopedic Foot & Ankle Society ankle-hindfoot scales was 83.3 points on the LCP-DT group, 84.6 points on the ZPLP group, and range of ankle motion averaged at 45 degrees, 48 degrees, respectively.
Figures and Tables
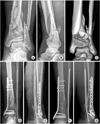
 | Fig. 1
(A-C) Preoperative radiographs and 3-dimensional computed tomography of a 53 year-old man shows a distal tibia and fibular fractures classified as the AO/OTA type 43-B1.
(D, E) The distal tibia fracture was stabilized with the Zimmer periarticular locking plate using a minimal invasive technique.
(F, G) Postoperative radiographs shows complete bone union with good alignment at 12 months after surgery.
|
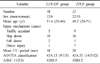
 | Fig. 2
(A-C) Preoperative radiographs and 3-dimensional computed tomography of a 61 year-old man shows distal tibia and fibular fractures classified as the AO/OTA type 43-A3.
(D) The distal tibia fracture was stabilized with the locking compression plate-distal tibia plate using a minimal invasive technique. Immediate postoperative anteroposterior radiograph shows 6 degrees of valgus malalignment.
(E) Immediate postoperative lateral radiograph shows 12 degrees of posterior angulation.
(F, G) Postoperative radiographs shows complete bone union at 18 months after surgery. patient had good functional outcome without further progression of malalignment.
|
References
1. Anderson LD, Hutchins WC, Wright PE, Disney JM. Fractures of the tibia and fibula treated by casts and transfixing pins. Clin Orthop Relat Res. 1974. (105):179–191.

2. Asche G. Results of the treatment of femoral and tibial fractures following interlocking nailing and plate osteosynthesis. A comparative retrospective study. Zentralbl Chir. 1989. 114:1146–1154.
3. Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001. 15:153–160.

4. Bone LB, Johnson KD. Treatment of tibial fractures by reaming and intramedullary nailing. J Bone Joint Surg Am. 1986. 68:877–887.

5. Borrelli J Jr, Prickett W, Song E, Becker D, Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma. 2002. 16:691–695.

6. Collinge C, Protzman R. Outcomes of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. J Orthop Trauma. 2010. 24:24–29.

7. Dickson KF, Montgomery S, Field J. High energy plafond fractures treated by a spanning external fixator initially and followed by a second stage open reduction internal fixation of the articular surface--preliminary report. Injury. 2001. 32:Suppl 4. SD92–SD98.

8. Edge AJ, Denham RA. External fixation for complicated tibial fractures. J Bone Joint Surg Br. 1981. 63:92–97.

9. Fisher WD, Hamblen DL. Problems and pitfalls of compression fixation of long bone fractures: a review of results and complications. Injury. 1978. 10:99–107.

10. Hahn D, Bradbury N, Hartley R, Radford PJ. Intramedullary nail breakage in distal fractures of the tibia. Injury. 1996. 27:323–327.

11. Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007. 38:365–370.

12. Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia--results in 20 patients. Injury. 2006. 37:877–887.

13. Helfet DL, Shonnard PY, Levine D, Borrelli J Jr. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997. 28:Suppl 1. A42–A47.

14. Karlström G, Olerud S. Fractures of the tibial shaft; a critical evaluation of treatment alternatives. Clin Orthop Relat Res. 1974. (105):82–115.
15. Khoury A, Liebergall M, London E, Mosheiff R. Percutaneous plating of distal tibial fractures. Foot Ankle Int. 2002. 23:818–824.

16. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994. 15:349–353.

17. Krackhardt T, Dilger J, Flesch I, Höntzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg. 2005. 125:87–94.

18. Lee KB, Song SY, Kwon DJ, Lee YB, Rhee NK, Choi JH. A comparison between minimally invasive plate osteosynthesis & interlocking intramedullary nailing in distal tibia fractures. J Korean Fract Soc. 2008. 21:286–291.

19. Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop. 2004. 28:159–162.

20. Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res. 2003. (408):286–291.

21. Olerud C, Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984. 103:190–194.

22. Park KC, Park YS. Minimally invasive plate osteosynthesis for distal tibial metaphyseal fracture. J Korean Fract Soc. 2005. 18:264–268.

23. Pugh KJ, Wolinsky PR, McAndrew MP, Johnson KD. Tibial pilon fractures: a comparison of treatment methods. J Trauma. 1999. 47:937–941.

24. Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury. 2004. 35:615–620.

25. Ristiniemi J, Flinkkilä T, Hyvönen P, et al. Two-ring hybrid external fixation of distal tibial fractures: a review of 47 cases. J Trauma. 2007. 62:174–183.

26. Ronga M, Longo UG, Maffulli N. Minimally invasive locked plating of distal tibia fractures is safe and effective. Clin Orthop Relat Res. 2010. 468:975–982.

27. Streicher G, Reilmann H. Distal tibial fractures. Unfallchirurg. 2008. 111:905–918.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download