Abstract
To report the unusual failure of proximal femoral nail antirotation (PFNA) at the level of lag screw hole and introduce a simple technique for removal of a broken intramedullary nail with a narrow hollow using a bulb-tipped guide wire and Kirschner wire.
As the indications and popularity for intramedullary (IM) nailing have expanded to the metaphyseal fractures of femur and tibia, the incidence of nail breakage has also increased. For such complication, exchange nailing is a simple, less invasive and effective procedure for selected patients for nonunion after IM nailing6). However, the removal of the broken nail is an inevitable and cumbersome procedure for exchange nailing1~7). The surgeon must be prepared to face this complication and needs to be familiar with as many methods as possible2). A broken distal part of the nail is sometimes very difficult to be removed from the medullary canal via the entry hole. It becomes even more difficult if the distal part is tightly fitted in the medullary canal and has a narrow hollow. Herein we report the details of the technique that we had tried with the literature review.
A seventy-five year old woman sustained subtrochanteric fracture of left femur after a fall accident. She took alendronate for 5 years for the treatment of osteopenia. The initial preoperative hip radiographs showed hypertrophy of the lateral cortex and transverse fracture with the medial beak. She underwent closed reduction and internal fixation with a long proximal femoral nail-antirotation (PFNA, Synthes, Paoli) at a local hospital. However, the reduction of the proximal fragment was not good enough and showed flexion deformity at the fracture site (Fig. 1). Nonunion and hardware failure developed at seven months after the operation (Fig. 2). Then, she was referred to our department for further treatment. Removal of the broken nail, exchange cephalomedullary nailing and bone graft was planned. The patient was placed on the operating table in supine position under the general anesthesia. A proximal part of the broken nail, a blade and distal interlocking screws were removed through the previous incision. The nail size was confirmed as PFNA 10 mm. A bulb-tipped guide wire was passed to the distal fragment of the nail through the entry point and medullary canal (Fig. 3). Once the bulb-tipped wire passed the distal fragment, we tried to put another straight guide wire into the distal fragment but failed due to its narrow hallow. As an alternative strategy, we introduced a 10 mm-long no. 3 Kirschiner wire (K-wire) into the distal interlocking hole of the nail through the pre-existing distal interlocking hole at the distal femur using a straight hemostatic forceps. The length of the K-wire matched with the size of the nail imprinted on the proximal part of the removed nail. A wire was pushed further into the interlocking hole using a blunt no 3. Steinmann pin (Fig. 4). Then, bulb-tipped guide wire was gently pulled out until the bulb abutted and locked with the K-wire at the distal interlocking hole. The guide wire was held using a holder, and it was tapped with a slotted hammer (Fig. 5). After removing the distal fragment, a new cephalomedullary nail (11 mm, Short ITST nail-Asian version, Zimmer, Warsaw) was inserted after reaming. A guide pin for the lag screw was inserted into the femoral head and neck through the targeting guide. The guide pin position was confirmed using the image intensifier. One lag screw (85 mm) and an anti-rotation screw (75 mm) were inserted into the femoral head. Then, two distal locking screws were inserted. Additionally, the nonunion site was exposed and the autogenous iliac bone was grafted in the usual orthopedic manner.
Removal of a broken nail with a narrow hollow is always challenging. Surgeons seek for a solid method using a simple instrument to resolve this problem1~8). Previously, we reported a method which uses a modified smooth guide wire6). However, the method can only be applied for a loosely fitted distal nail fragment in the canal because the holding power of the hook is not strong enough to overcome the tightly fixed fragment in the medullary canal. In our case, as described above, the broken nail fragment was very long and was tightly fixed at the isthmus. Regardless of the outer diameter of nail (range: ∅9, ∅10, ∅12, ∅14 mm) all of the PFNA has same inner diameter which is 4.5 mm. Considering the narrow hollow (∅4.5 mm), we couldn't insert a thin bulb-tipped wire and straight guide wire together at the distal fragment8). Because average diameter of guide wire range from 2.8 mm to 3.5 mm. Next we might try inserting the large bulb tipped guide wire from the femoral condyle reversely5). The large bulb can be locked at the distal entry of the nail, providing enough strength to remove the nail tightly fitted at the isthmus. Concerning the articular damage and positioning the patient on the fracture table precluded this method. The special removal instrument can be screwed into the proximal end of the distal nail. However, the hollow was too small, and the nail was located too far from the entry site. We finally tried K-wire locking technique as described above. The bulb-tipped guide wire was jammed at the distal interlocking hole due to the K-wire at the hole and provided enough holding power. It is important that the bulb-tipped guide wire must be pulled at all time. Special attention should be paid when the broken nail is toggling at the wide distal femoral canal. Otherwise, the K-wire in the distal interlocking hole may dislodge and fall into the wide intramedullary canal. The semi-lateral position of the patient will increase the risk of the K-wire dislodging. We recommend external rotation of the limb and make it as neutral as possible when the patient is positioned in semi-lateral position. If the lateral position is preferred, a small cortical screw may be used instead of K-wire3). The screw head may prevent dislodging of a screw to the wide medullary canal. Once the K-wire reaches the isthmus, it can be removed without dislodging. We trimmed the edge of the K-wire carefully to prevent it from scratching and bumping the inner cortex of the medullary canal. The limitation of this method is that it is not applicable if the nail breaks at the most distal hole of the nail. Fortunately, such a case is rare, and breakage usually happens at more proximal hole of the distal interlocking holes. Considering the convenient preparation of a distal interlocking hole after removal of the screw and universal availability of a bulb-tipped guide wire and K-wire, we expect this method can be used to remove any kind of broken nails with a narrow hollow. If the distal interlocking hole is filled up with the bone and fibrous tissue due to previous dynamization, the hole may be opened using the free hand technique.
Figures and Tables
Fig. 1
(A) Preoperative radiograph shows subtrochanteric fracture of left femur: Hypertrophy of the lateral cortex and transverse fracture with medial beak were noticed.
(B) Postoperative radiograph after the initial operation: inadequate reduction status with flexion deformity at the fracture site.

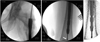
Fig. 3
Intraoperative radiographs from image intensifier; after removing of the proximal portion of broken nail, bulb-tipped guide wire was introduced (arrow).
References
1. Brewster NT, Ashcroft GP, Scotland TR. Extraction of broken intramedullary nails--an improvement in technique. Injury. 1995. 26:286.

2. Georgilas I, Mouzopoulos G, Neila C, Morakis E, Tzurbakis M. Removal of broken distal intramedullary nail with a simple method: a case report. Arch Orthop Trauma Surg. 2009. 129:203–205.

3. Karladani AH. Removal of a broken nail using a guide wire and a screw. Acta Orthop. 2006. 77:986–988.

4. Levine JW, Georgiadis GM. Removal of a broken cannulated tibial nail: a simple intramedullary technique. J Orthop Trauma. 2004. 18:247–249.
5. Magu NK, Sharma AK, Singh R. Extraction of the broken intramedullary femoral nail--an innovative technique. Injury. 2004. 35:1322–1323.

6. Park SY, Yang KH, Yoo JH. Removal of a broken intramedullary nail with a narrow hollow. J Orthop Trauma. 2006. 20:492–494.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download