Abstract
Purpose
To evaluate the anatomic and functional outcome of retrograde intramedullary single wire fixation for metacarpal shaft fractures of the little finger.
Materials and Methods
hirty one consecutive patients with closed metacarpal shaft fractures of the little finger who have been treated with retrograde intramedullary single wire fixation were evaluated. Fracture union and angulation were analyzed radiologically, and clinical evaluations were performed including range of motion, DASH score and complications.
Results
Fracture union was achieved in all cases and callus formation was obvious at postoperative 41 days. Average angulation of fracture site was 3° in the coronal plane and 1.2° in the sagittal plane at the last follow up and no measurable metacarpal shortening was observed. Mean TAM was 253° and DASH score was 2.6. There were two cases of pin migration as intermediate complications.
Conclusion
Closed reduction with subsequent percutaneous retrograde K-wire fixation produced good radiological and functional results. We recommend this minimally invasive technique which provides adequate fixation of displaced little finger metacarpal shaft fractures with good functional results and low morbidity.
Metacarpal fracture of the little finger is one of the common fractures of hand and vast majority of these fractures are stable and treated conservatively. The hand tolerates these injury well and serious residual functional deficits are rare1), therefore these injuries are often considered trivial and treated lightly. On the other hand, this fracture can sometimes cause significant morbidity and patient dissatisfaction. Rotational malalignment and stiffness will produce a serious functional deficit and angular malunion can result in a cosmetic defect poorly tolerated by some patients. Displaced metacarpal shaft fracture can be treated with a variety of techniques, ranging from closed reduction and early mobilization within the splint to open reduction and internal fixation. All possible treatment options have advantages and disadvantages, but there is no one treatment that is always the best.
Surgical treatment is justified in certain cases like unstable, displaced fractures. When surgical intervention is necessary, intramedullary fixation using small flexible rod or wire can be an option that provides stable internal fixation while minimizing the extent of soft tissue trauma among many different operative procedures4,5,8,10,11,14). We chose retrograde closed intramedullary pinning with a single Kirschner wire (K-wire) and early mobilization. This is almost the same procedure which was described by Flatt5) except bending of the proximal tip and removal of the pin after fracture union. In spite of long history and good results of retrograde intramedullary single wire fixation, there have been few recent reports about this simple treatment method. We applied this technique mostly to the little finger metacarpals because other metacarpals have higher risk of carpometacarpal joint or tendons injuries. We reviewed a series of 31 patients who were managed by this procedure and report anatomic and functional outcome.
Thirty one consecutive patients, 25 men and 6 women with closed metacarpal shaft fractures of the little finger who have been treated with closed reduction and percutaneous retrograde intramedullay K-wire fixation, were analyzed retrospectively. We excluded the comminuted fractures in this study. Preoperative evaluation of hand function showed that none of the patients had any pre-existing functional deficits regarding flexion, extension and rotation. The indications for this surgical procedure were transverse or short oblique closed shaft fractures with less than 50 percent apposition of bone ends, more than 30 degrees angulation, more than 4 mm shortening or any degree of malrotation which were not manually reduced nor maintained.
The average age at the time of surgery was 26 years old (range, 15~47 years). Twenty three patients had transverse fractures of the metacarpal mid shaft, and eight patients had short oblique fractures. This procedure was not applied to long oblique or spiral fracture, multiple fractures, and fractures in association with severe soft-tissue crush injuries, because we believe that other fixation methods could provide better stability.
Radiological evaluation of anterior-posterior and lateral radiographs assessed healing, displacement, angulation and shortening. Cortical margin of shaft was marked on radiographs and it was assessed by comparing with neighboring metacarpals. Clinical evaluation included assessment of total active motion (TAM), the range of motion (ROM) of fifth metacarpophalangeal (MP) joint, postoperative complications. The aesthetic outcome was also assessed and each subject completed the Disabilities of the Arm, Shoulder and Hand (DASH) outcome questionnaire after instruction. The score were evaluated in the standard manner such that the possible score range was between 0 (no disability) and 100 (complete disability)9). For the evaluation of aesthetic results, subject's opinion on appearance was used (1=normal, 2=virtually normal, 3=disfigured, 4=mildly unsightly, 5=very unsightly)15).
This study was approved by the Committee on Clinical Investigation of our Institutional Review Board.
The surgery was performed under general or regional anesthesia with image intensification, preferably with a tourniquet on the upper arm. Under the fluoroscopy, closed reduction of the metacarpal fracture was achieved by manipulation, and 1.6 mm K-wire was inserted from metacarpal head with MP joint flexion for easy access to the medullary canal (Fig. 1). When the wire tip passed fracture site and reach to metacarpal base, wrist was bent maximum and further penetration was performed to proximal area (Fig. 2). The distal end of K-wire was pulled up until its tip end lay within the metacarpal head (Fig. 3). Penetrated proximal part of wire was bent over, cut and buried under the skin (Fig. 4). During this procedure, any rotation of fracture was carefully checked with passive flexion and extension motion of the finger. Ulnar gutter splint was applied for rotational stability and pain relief. It was changed to extension block splint and encouraged motion exercise from postoperatively 1 week. After fracture healing, the wire was removed with local anesthesia in the outpatient department in all cases. We make small skin incision at proximal bended wire and pull out that with local anesthesia.
The average follow-up period was one year nine months, with a range of 12~42 months. Average operation time was 18 minutes (range, 12~27 min) and no immediate complication was seen. Rotational malalignments were detected in 4 cases preoperatively and they were corrected by manual reduction without any further invasive procedure. Distal migrations of K-wire tip to the MP joint were seen in two patients during the follow up. One patient showed migration in postoperative 3 weeks and the other in 4 weeks (Fig. 5). Migrated pins were removed immediately at the time of detection and gentle ROM exercise was recommended within the splint.
Radiological evaluation revealed evidence of callus formation in all fractures at 41 days in average (range, 34~58 days) such that splints and wires were removed at the same time in out-patient clinic. All the fractures had united and mean angular deformity were 3° (0~7°) in the coronal plane and 1.2° (0~5°) in the sagittal plane. Previous penetrated metacarpal heads by K-wire were healed completely without any residual change on the last follow up x-ray and there was no measurable shortening. At the final follow up, all patients had regained little finger MP joint motion of average extension 9°, flexion 87°. None of the patients had other joints stiffness at the final follow up. By TAM grading system, it ranged from 225° to 260°, mean was 253°. All patients stated subjectively that the function at the MP joint of little finger had returned to normal including the patient who had pin migration. DASH score was average 2.6 at the last follow up, ranging from 0 to 8. None of the patient had a clinically detectable rotational deformity and they reported satisfaction with their resulting appearance. Even though small skin incision was made during pin removal, it did not make any remarkable scar. Mean cosmesis score was 1.6 and it indicated the appearance was better than virtually normal. All continued with their previous occupations.
The deformity from metacarpal shaft fracture causes loss of hand function and unpleasant cosmetic appearance. Most cases can be managed by conservative means after closed reduction, but surgical intervention is indicated when unacceptable reduction persists. Metacarpal fracture of the little finger is more common, and acceptable range is wider than any other metacarpal bones because mobile carpometacarpal joint can compensate some degree of deformity.
Acceptable limits have been quoted as greater than 50 percent apposition of bone ends, no rotational deformity, and angulation of less than 30°7). In any case, angulation of more than 30°, shortening of more than 4 mm, or a combination of these findings interferes with normal intrinsic muscle tension dynamics and may cause weakness, loss of endurance, cramping and clawing, each of which should be prevented by correction of deformity10,12). Author's surgical indication was based on these criteria.
When the fracture is displaced and unstable, the main purpose of the treatment is to minimize any deformities and restore anatomical relations between the metacarpal bones. The ideal method of metacarpal fracture treatment should obtain stable fixation and allow early recovery of function while minimizing the risk of soft tissue damage and scar formation. It should also be reliable, simple, and easy to perform. Although plate fixation can provide rigid fixation in anatomical alignment, it can cause extensor tendon adhesion and the plate and surrounding new bone formation on the back of the metacarpal can cause an appreciable cosmetic deformity. Intramedullary K-wire fixation is one option which a hand surgeon could offer patients who have unstable metacarpal shaft fractures with advantages of minimal scar formation and soft tissue trauma. Some surgeons use single large wire whereas others use multiple small intramedullary wires. Specially designed implants were applied by several surgeons although most use Kirschiner wires5,8,14). We performed closed intramedullary pinning with a single large, 1.6 mm K-wire and encouraged joint mobilization at early period. This procedure is suitable for the little finger metacarpal shaft fractures because mobile carpometacarpal joint could prevent transfix the carpus, and relatively radial location of extensor tendons to the 5th metacarpal base could lower the risk of those tendon injuries. Our method is similar to Flatt's procedure5) but we bent proximal wire tip, buried under the skin and removed the pin after fracture union instead of burying and leaving within the medullary canal. It is also different from the previously described multiple-pin technique used by Foucher6), Gonzalez8) and Faraj4). Authors did not make any skin incision during the procedure because all pins just penetrated percutaneously. Diminishing extensor tendon adhesion by minimal soft-tissue dissection and no exposure of the fracture site makes this method of fixation attractive. The fracture hematoma is not disturbed with obvious advantages in regard to fracture healing and burying the wires reduces the risk of pin site infection. Any late complication from remained pin was not seen because no wires are left permanently within the medullary canal.
Potential deleterious effects on tendon or joint capsule scarring from the MP joint can be avoided because joint movement is possible during the early treatment phase, and no MP joint implant is present by withdrawing the K-wire. We encouraged continuous active motion exercise from one week after surgery and it could prevent any extensor mechanism complications. We also noticed that 1.6 mm sized K-wire penetration to the articular surface of metacarpal head could be healed without any complications in the joint from no abnormal change of metacarpal head in the last follow up x-ray and good range of motion.
Good results have been reported for the other intramedullary technique with excellent fracture healing, good cosmetic results and few complications4,13), and our series adds merit to this method of fixation. But authors realized that pin migration could make serious complication to the joint unless it is not managed appropriately. Bent proximal wire tip should be located close to the metacarpal base during the procedure for prevention of this problem. Author's all pin migrated patients had longer proximal tip and even small motion of wrist could make the pins migrate.
Theoretically, fixation with a single K-wire would allow rotational instability at the fracture site and some surgeons recommended supplemental wire fixation like transfixation to adjacent intact metacarpals3). But by placing the finger in position of 70 to 90 degrees MP joint flexion, rotational control can be achieved through the immobilization even with single intramedullary wire fixation2). We corrected any rotational malalignment during the operative procedure, and it was immobilized temporary and carefully managed while motion exercise was performed.
We applied this procedure only to short oblique or transverse fracture because it was hard to control the length and rotation in oblique and spiral fracture which are usually the result of torsional forces. Even though this procedure has some limitation like this, the findings of this study support that retrograde intramedullary pin fixation could provide adequate fixation of displaced or angulated metacarpal shaft fractures with good functional results and low morbidity when the indication is appropriate. We recommend this minimally invasive technique for the transverse or short oblique metacarpal fractures of the little finger which is technically easy to perform, saves operating time, produces an insignificant scar and demands no specific instrument.
Figures and Tables
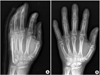
 | Fig. 11.6 mm K-wire is inserted from metacarpal head with metacarpophalangeal joint flexion for easy access to the medullary canal. |
References
1. Choi JY, Shin HK, Son KM, Ko CS. Operative treatment in fracture-dislocations of carpometacarpal joints. J Korean Fract Soc. 2005. 18:443–451.

3. Downing ND, Davis TR. Intramedullary fixation of unstable metacarpal fractures. Hand Clin. 2006. 22:269–277.

4. Faraj AA, Davis TR. Percutaneous intramedullary fixation of metacarpal shaft fractures. J Hand Surg Br. 1999. 24:76–79.

5. Flatt AE. Closed and open fractures of the hand. Fundamentals of management. Postgrad Med. 1966. 39:17–26.
6. Foucher G. "Bouquet" osteosynthesis in metacarpal neck fractures: a series of 66 patients. J Hand Surg Am. 1995. 20:S86–S90.

7. Galanakis I, Aligizakis A, Katonis P, Papadokostakis G, Stergiopoulos K, Hadjipavlou A. Treatment of closed unstable metacarpal fractures using percutaneous transverse fixation with Kirschner wires. J Trauma. 2003. 55:509–513.

8. Gonzalez MH, Igram CM, Hall RF Jr. Flexible intramedullary nailing for metacarpal fractures. J Hand Surg Am. 1995. 20:382–387.

9. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996. 29:602–608.

10. Kelsch G, Ulrich C. Intramedullary k-wire fixation of metacarpal fractures. Arch Orthop Trauma Surg. 2004. 124:523–526.

11. Kim MH, Yoo MJ, Kim JP, Lee JH, Lee JW. Bouquet pin intramedullary nail technique of the 5th metacarpal neck fractures. J Korean Fract Soc. 2007. 20:64–69.

12. Low CK, Wong HC, Low YP, Wong HP. A cadaver study of the effects of dorsal angulation and shortening of the metacarpal shaft on the extension and flexion force ratios of the index and little fingers. J Hand Surg Br. 1995. 20:609–613.

13. Mockford BJ, Thompson NS, Nolan PC, Calderwood JW. Antegrade intramedullary fixation of displaced metacarpal fractures: a new technique. Plast Reconstr Surg. 2003. 111:351–354.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download