Abstract
Purpose
To examine the details of lymphedema, upper limb morbidity, and its self management in women after breast cancer treatment.
Methods
Using a cross-sectional survey design, 81 women were recruited from a university hospital. Lymphedema was detected by a nurse as a 2-cm difference between arm circumferences at 6 different points on the arm. Degrees of pain, stiffness, and numbness were scored using a drawing of upper limb on a 0~10 point scale. Aggravating conditions and self-management for lymphedema were also recorded.
Results
The mean age of the participants was 52.5 years; the average time since breast surgery was 29.7 months. Histories of modified radical mastectomy (55%) and lymph node dissection (81%) were noted. Lymphedema was found in 59% of women, then pain and stiffness were prevalent most at upper arm while numbness was apparentat fingers, and the symptom distress scores ranged 3.9~6.7. Women experienced aggravated arm swelling after routine housework with greatly varied duration. Self-management was conservative with a wide range of times for the relief of symptoms.
Conclusion
Lymphedema education for women with breast cancer should be incorporated into the oncologic nursing care system to prevent its occurrence and arm morbidity. Risk reduction guidelines, individually tailored self-care strategies, and self-awareness for early detection need to be refined in clinical nursing practices.
Lymphedema is a common, debilitating complication of the surgical removal or radiation treatment of lymph nodes during breast cancer treatment. The occurrence of lymphedema after breast cancer treatment varies greatly, from 5% to 60% (Poage, Singer, Armer, Poundall, & Shellabarger, 2008), depending on the predisposing factors and on the diagnostic criteria. In 3-year prospective studies, 20.7% (Clark, Sitzia, & Harlow, 2005) and 32% (Paskett, Naughton, McCoy, Case, & Abbott, 2007) of the women studied were found to have lymphedema after breast cancer treatment. Of the 42% of women experiencing lymphedema, 80% of cases had occurred in the first 2 years after treatment (Norman et al., 2009). In Korea, cross-sectional studies have reported the prevalence of lymphedema to be 24.9% (Park, 2005) and 32.7% (Chun et al., 2005). Also, 45.5% of lymphedema cases were found to occur within 6 months of axillary dissection for breast cancer (Lee et al., 2006). Even using a conservative definition, the incidence is estimated to be from 20% to 25% (Armer, 2010; Erickson, Pearson, Ganz, Adams, & Kahn, 2001) and women may experience lymphedema at any time in their lives after breast cancer treatment.
Lymphedema after breast cancer treatment cannot be over looked since it causes not only symptoms of pain, numbness, stiffness, and limitations in the range of motion (Lee, 2006; Park, 2005) but has major effects on emotional and psychological health, social life and interpersonal relationships, functional status, and quality of life (Ahmed, Prizment, Lazovich, Schmitz, & Folsom, 2008; Fu, Chen, Haber, Guth, & Axelrod, 2010; Meneses & McNees, 2007; Moffatt et al., 2003). Lymphedema is incurablethus it requires lifelong management once detected. Education regarding early prevention and self-care cannot be overemphasized in clinical nursing practices.
Risk factors of lymphedema such as obesity, the extent of axillary node dissection, axillary radiation therapy, and others have been identified (Erickson et al., 2001). Lymphedema risk reduction practices (National Lymphedema Network, 2008) have been disseminated through standard patient education with breast cancer patients. However, the triggering or exacerbating conditions for lymphedema that women are exposed to in daily life, to what extent they are able to adhere to preventive guidelines, and their symptom management have not been studied. Nursing care for lymphedema would not be successful without the careful assessment of distress symptoms and related factors, as well as self-care education tailored to each individual. This study seeks to bridge the gap by taking into account aspects of women's daily reality in relation to current recommendations for preventive measures and self-care guidelines for lymphedema.
Especially in Korea, breast cancer is prevalent in women aged 30s and 40s and the survival of breast cancer patients consistently increases (National Cancer Information Center, 2010). Since after cancer treatment, maintaining optimal function is one of the quality of life goals in the treatment of cancer patients, lymphedema prevention and management is essential for long-term survival after breast cancer. In addition, women's workload, roles, and lifestyles differ by the sociocultural contexts to which they belong, and so identifying socioculturally-specific circumstances related to lymphedema manifestation would be useful. Research is needed on education to increase patient awareness of lymphedema, to determine the efficacy of self-care strategies, and to develop practical guidelines that women can apply in their daily lives. This study explores the incidence of lymphedema, upper limb morbidity, causal and aggravating factors of arm swelling, as well as patterns of self-management in women after breast cancer treatment.
Women were recruited from a university-affiliated breast cancer clinic in Seoul during their follow-up visits. Inclusion criteria were if they were diagnosed with primary breast cancer, had breast surgery (with sentinel lymph node biopsy or lymph node dissection), had no neurologic disease or disability in physical functions before the breast surgery, and agreed to participate in the study. Women were excluded if they experienced a recurrence of breast cancer, had repeated breast surgery, or were diagnosed with cancer in both breasts. As lymphedema could occur at any time points after breast cancer treatments given accordance with the stage of cancer, types of surgery and adjuvant therapy as well as time since those treatments were not limited rather to include wide ranges of disease related characteristics. A total of 96 women participated in the study during the data collection period, of which 15 cases were excluded from the data analysis due to incomplete answers.
Sample size was not calculated based on power analysis since this study did not contain a statistical testing of hypotheses. Rather it aimed to explore current status of lymphedema for preliminary inquiry, thus all possible subjects were recruited from the clinic during the planned 3 months of data collection period.
Lymphedema was defined as present if a difference in circumference greater than 2 cm was measured by universal tape measurement between the affected and unaffected arms (Armer & Fu, 2005; Thomas-MacLean, Miedema, & Tatemichi, 2005). Measurements were taken by one nurse from six points most commonly used in clinical evaluation (Erickson et al., 2001; Park, 2005): the metacarpophalangeal joints, wrist, the lateral epicondyle of the humerus (noted hereafter as "the humerus"), 10 cm below, and 7 cm and 15 cm above the lateral epicondyle.
Upper limb symptoms
Upper limb morbidity was assessed by both symptoms and functioning. For upper limb symptoms, the degree and location of pain, numbness, and stiffness were assessed with a figure created by the authors. These symptoms are known to be the most common in relation to lymphedema and breast cancer treatment (Fu, Axelrod, & Haber, 2008; Lee, 2006). The degree of each symptom may differ by location in the upper limb depending on usage and the activities that women performed. Thus, the authors included an image of the upper body in the questionnaire and indicated 11 points, as a means of evaluating distress symptoms associated with each physical location. This novel method of eliciting symptom information from participants was thought to generate more detailed data than previous studies. The shoulder, remaining breast tissue, armpit, side of the chest wall, back, upper arm, elbow, forearm, wrist, hand, and fingers were the 11 locations marked in that figure, and participants were asked to score the degree of discomfort from 0 (none) to 10 (extremely severe) in three separate figures for pain, numbness, and stiffness. Higher scores indicated greater distress symptoms.
Upper limb functioning
In this study, overall upper limb functioning was evaluated with two questionscreated by the authors regarding the degree of usage and the strength of the arm on the affected side for simple and easy assessment in clinical settings.
To assess the degree of usage of the arm, participants were asked to indicate "To what extent do you use the affected arm in daily life?" using a score from 0 (rarely use) to 10 (use to the same extent as before treatment). A higher score meant better functioning affected arm.
The degree of strength was described on a scale ranging from 0 (noticeably much weaker) to 10 (same as before treatment) by asking "What do you think of the strength of the affected arm now compared to prior to treatment?" Thus a higher score meant more strength in the affected arm after cancer treatment.
From the Lymphedema Risk Reduction Practices of the National Lymphedema Network (2008), 15 possible risk conditions for causing lymphedema were listed in a structured questionnaire and participants were asked to check all conditions that seemed to cause or aggravate arm swelling, along with the approximate duration during which women were exposed to each condition. Women were also encouraged to describe, in a blank space next to each condition, further details regarding the indicated condition. For example, women could list specific activities, such as dishwashing, cooking, or doing laundry for the item 'when doing housework'.
In order to investigate women's self-management of arm swelling, participants were asked to describe how they relieved arm swelling when it occurred. This question was asked to gather data regarding existing common practices, since it is a topic that has not yet been explored in the literature.
The study was approved by the breast clinic and the institutional review board (2010-42) of the university with which the principal investigator is affiliated. Once women visited the clinic for follow-up care, they were invited to the study by a nurse at the clinic if they fulfilled the inclusion criteria, and written informed consent was obtained from each participant prior to data collection which was done from August 15, 2010 to November 15, 2010.
Women were provided with a structured questionnaire to complete, requiring approximately10 to 15 minutes to complete, and a private, comfortable space was provided in the clinic for them for this purpose. The nurse then measured the arm circumferences of each participant, and additional disease-related data regarding cancer diagnosis and stage, type of surgery, and adjuvant treatment were taken from the medical records by the nurse. Each woman was encouraged to ask questions regarding their health or concerns after the completion of data collection.
Using SPSS/WIN 12.0 software, descriptive statistics analyzed demographic and disease-related characteristics as well as the incidence of lymphedema. Percentages and the mean scores of the upper limb symptoms and functioning were also obtained. Responses regarding the causes of the condition and self-management were categorized by their contents and analyzed for response frequencies.
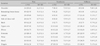
As shown in (Table 1), women in their 40s and 50s were about 69% of the sample, with an average age of 52.5 years. Most were diagnosed with infiltrating ductal carcinoma, and the most common stages of cancer were II (37.8%), III (35.1%), and I (21.7%). More than half of the women had had a modified radical mastectomy and 81% had undergone lymph node dissection, and had undergone adjuvant chemotherapy treatment (77.8%) or radiotherapy (53.1%). The time since breast surgery ranged widely (1~96 months), from 1 year (38.2%), 3 years (32.0%), 5 years (13.5%), through 7 years or more (16.3%) with an average of 29.7 months.
About 45.7% of the women had breast surgery on the right breast; 94% were the right-handed. One-third of the participants (34.6%) reported not having received lymphedema education because they hadmissed weekly education sessions, while more than one-third of those who had received education answered that they either forgot the contents of education or felt it had not been very helpful.
Based on measurements, 59.3% (n=48) of women were found to have lymphedema at one or more of the locations. The most frequent locations of lymphedema were 10 below the humerus and 7 above it, each of which was reported in 77% of the 48 women. The most extreme case of lymphedema was noted to be an 8-cm difference between arms at 10 cm below the humerus. The knuckles and wrist showed a relatively low percentage of lymphedema occurrence (Table 2).
The frequencies and mean symptom scores for pain, numbness, and stiffness at multiple locations of the upper limb of the affected side are presented in (Table 3). Overall, 85% (n=69) of the women complained of one or more of these symptoms in their affected limb.
Pain scores at each location ranged from a minimum of 5.0 to a maximum of 6.7 out of the 10-point scale. The upper arm, armpit, and shoulder were the locations that 30% or more of the women complained of pain. The side of the chest wall and shoulder were the locations that women complained of the most severe pain with scores over 6.0. Overall, pain seemed to be most prevalent in the upper part of the limb.
On the other hand, numbness was prevalent in the hand (23.5%) and fingers (33.3%), though the mean symptom scores for these locations were quite similar to those of all the other locations, ranging from 3.9 through 5.5. Stiffness was most frequently found in the upper arm (28.4%), then forearm, followed by the armpit, hand, and fingers, which were scored similarly for stiffness.
Meanwhile, the women answered that they used the affected arm less than before the surgery, with a mean score of 5.1±3.5, as indicated on a scale from 0 (rarely use) to 10 (use to the same extent as before surgery). Regarding the strength of the affected arm, women evaluated the strength of the affected arm compared to prior to surgery to be 6.1±3.7 on a scale of 0 (noticeably much weaker ) to 10 (same as before treatment).
Table 4 describes conditions that women felt aggravated arm swelling in daily life and the details of each condition, including their duration. Doing housework was the most common condition, listed by 43 women, including cooking, house cleaning, mopping, dish washing, and hand washing laundry. Notably, some women reported doing quite long and strenuous tasks, such as paring chestnuts for a couple of hours or making kimchi with 60 cabbages. The duration of each activity varied in range from a few minutes to 2~3 hours.
Exercise was also listed as one of the triggering factors in about 36% (n=29) of the women. Walking and climbing mountains are two of the most popular physical activities in Korea. However, after 90~180 minutes of climbing, the women's arms swelled. One woman answered that she had felt arm swelling after 2 minutes of arm stretching. Some participants played golf or did dumbbell lifting, then perceived their arm swelling soon thereafter. Heavy lifting was reported as one of the aggravating conditions in 24 women. They realized that their arms had swollen after about 30 minutes of activity, including handling water jars, books, dish piles, or stones in the garden.
In addition, women experienced arm swelling when they felt tired (n=16), when there was pressure on the arm during sleep (n=15), or due to repeated use of the arm (n=13) such as during employment activities, scrubbing the skin while bathing, and computer use. Each activity had a wide range of duration. Women reported being exposed to hot places in public bathhouses, including dry saunas or elvan stone saunas, which are popular in Korea. The time exposed to heat varied from a few minutes to 1 or 2 hours.
Meanwhile some women noticed that reduced use of the arm caused arm swelling, such as after sleep or sitting for long periods of time. When they felt high levels of stress, had an infection or insect bite, applied a compression stocking or bandage, or were exposed to changes in the weather, arm swelling was aggravated.
For relieving symptoms (Table 5), the most frequently used methods were elevating the arm (n=26), massaging (n=22), or resting (n=20). Fourteen women were able to use a compression pump with a stocking through clinic visits, and 12 women put a bandage on the swollen arm. Body stretching (n=13) and exercise such as swimming (n=4) were also tried. Similar to symptom-aggravating conditions, the time duration for these symptom-relieving methods also varied by participant and method.
Although the occurrence of lymphedema after breast cancer treatment is known to be 5% to 60% (Poage et al., 2008), the incidence in this study was found to be 59.3%, which was higher than previous results of 32.7% (Chun et al., 2005) when including 2 years or more follow ups and 42% (Norman et al., 2009) of 5-year cumulative incidence. This could be related to the self-selection of participants who had an interest in lymphedema issues as identified during follow-up care after cancer treatment. However, it could also be related to these women's known risk factors, undergoing lymph node dissection (81%) and radiation therapy (53%). It is important to take into account predisposing factors when comparing incidence rates; in the study of Chun et al. (2005) indicating a 33% lymphedema occurrence, 22% of the women had received a modified radical mastectomy with radiation therapy. Meanwhile, a 25% incidence was reported in a group of women of whom 46% had undergone radiation therapy and 88%, lymph node dissection (Park, 2005). Bani et al. (2007) found a 35% lymphedema occurrence from a group of women among whom 81% had undergone radiation therapy, while a sample with 77% lymph node dissection and 94% radiation therapy was reported to have a 12% rate of lymphedema within 12 months after breast cancer treatment. Since aggressive cancer treatment is inevitable, women are exposed to the risk of lymphedema. Because the treatment modality of breast cancer varied by study, it is critical to evaluate lymphedema incidences in light of the potential risk factors of each sample involved.
From this study, it should be noted that the locations of the humerus, 7 cm above it, as well as 10 cm below it were the parts most vulnerable to upper lymphedema, which was a pattern similar to Park's (2005) results. Particularly, the study revealed the severity of lymphedema at each location, and the difference between the two arms reached as high as 8 cm, which is quite large. This strongly suggests that the nurses predict possible lymphedema at prevalent locations and perform routine screening through careful and accurate assessment of the changes in the affected upper arm. However, according to Jeffs' study (2006), despite the fact that 59% of women experienced lymphedema after breast cancer treatment, only 32% of all participants sought professional help within 3 months another 17% delayed treatment more than 12 months. This meant that lymphedema after breast cancer is not well recognized as an important health issue among healthcare professionals. Since little is yet known on how serious the upper lymphedema is and how many women have sought help for it, future studies and clinical practice guidelines need to focus on both issues and strive for prevention and symptom management for women.
It has not yet been explored to what extent the impact of lymphedema could influence women's daily life. From the present study, the arm could function in just half of the full range, and the strength of the affected arm had also been reduced significantly relative to before the surgery and cancer treatment. These physical changes can have a major effect on performing daily activities (Bennett, Winters-Stone, & Nail, 2006) however, the patients' condition rarely seemed to have been identified by oncologic nurses or doctors after active cancer treatment. Therefore, empowering women to perform specific self-care strategies such as maintaining functional capacity or exercise prescriptions should be practical nursing interventions.
Another meaningful finding of this study related to the results above was to identify what conditions aggravated the arm swelling and lymphedema women experienced. More than half of the participants were experiencing arm swelling after doing housework. Mostly women were back to regular life after the series of cancer treatments; however, the type and duration of tasks each reported performing everyday varied widely, such as doing 60 minutes of cooking, washing, or laundry. A few individuals related stories of occasionally doing tasks such as 3 hours of chestnut paring or making 60 heads of kimchi, which caused arm swelling. Although exercise is usually recommended for women, walking and mountain climbing between 90 minutes and 3 hours seemed to cause symptoms. There was a wide range of duration between arm stretching and the onset of arm swelling in different participants, with one woman able to play 36 holes of golf before having symptoms. Women's roles and responsibilities can differ by culture and family; thus the extent of upper lymphedema can vary. Specific standards or evidence-based guidelines are required for women to follow for managing their physical activities.
In addition, it was apparent that women were still exposing themselves to risks such as spending time in hot places such as saunas and public baths, sudden weather changes, and doing housework for long periods of time, despite general precautions against doing so (Ridner, 2002). The result requires healthcare professionals evaluate the effects of routine education that they had provided besides, there has been no report on how well the women adhere to these guidelines. Since providing information about upper lymphedema has shown significant effects on reducing symptoms (Fu et al., 2010), women's awareness and implementation of self-care should be stressed in nursing education for lymphedema prevention.
Women practiced conservative self-management by elevating, resting, or massaging the affected arm for symptom relief and the variation in the duration of this self-care was notably wide. As McNeely et al. (2010) concluded from a meta-analysis of exercise interventions for women with breast cancer, there seemed to be no structured instruction or supervision. Further investigation of the type and intensity of, and adherence to exercise is needed to determine lymphedema management guidelines.
Despite the impact of lymphedema on women's life after breast cancer treatment, until now, details of symptoms, aggravating conditions of arm swelling in daily life, and self management methods have not been adequately explored in Korea. This study collected descriptive data on those questions, investigating degrees of pain, stiffness, and numbness at 11 points of the upper limb, as well as in identifying complaints associated with each point. The current practice of gathering general information on women's complaints, such as "pain in the arm" or "stiffness of the upper limb", is too vague. Data gathering needs to be modified to collect more specific information on each part of the limb for identifying symptom occurrence accurately, to facilitate effective management based on patient reports, and to identify practical outcomes of applied interventions.
One other valuable finding was to explore actual conditions and circumstances that women reported to aggravate arm swelling. The study results indicated that women faced the risk factors during daily life and role performance, therefore, in the future, nurses should take better precautions against lymphedema by providing customized patient education based on each woman's awareness level and potential vulnerability. Moreover, lymphedema can be diagnosed by a nurse using arm circumferences the actual measurement should be performed by nurses, and the data should be incorporated into the document to follow up on quality nursing care outcomes. Along with that, concrete and standard guidelines should be provided for women to prevent risk behaviors and promote efficient self-management strategies.
Recently, the benefits of exercise for this population have drawn interest. However, standardized or evidenced-based interventions are not yet available, which requires further intervention research on exercise prescription, women's adherence, and effects of exercise on lymphedema and physical functioning in women with different characteristics.
Although this study had strong evidence of lymphedema occurrence, as a cross-sectional study, it was limited in not having access to initial arm circumference data to compare to post-cancer treatment data. Longitudinal nursing assessment of lymphedema would provide useful descriptive data to reveal symptom patterns and the effects of nursing interventions. Relatively small sample size was one of the limits of the study. A wide range of data distribution, such as time since diagnosis, was not controlled for in this study design due to the aim of achieving an initial exploration of the lymphedema picture in Korea. This prevented us from finding the period of time of lymphedema occurrence as well as aggravating or changing patterns of the symptoms. These limitations could be overcomein future prospective research and intervention studies with larger sample sizes to identify evidence needed to develop systematic and valid nursing care strategies.
References
1. Ahmed R.L., Prizment A., Lazovich D., Schmitz K.H., Folsom A.R. Lymphedema and quality of life in breast cancer survivors: The Iowa women's health study. Journal of Clinical Oncology. 2008. 26:5689–5696.
2. Armer J. Research on risk assessment for secondary lymphedema following breast cancer treatment. Cancer Epidemiology, Biomarkers and Prevention. 2010. 19:2715–2717.
3. Armer J., Fu M.R. Age differences in post-breast cancer lymphedema signs and symptoms. Cancer Nursing. 2005. 28:200–207.
4. Bani H.A., Fasching P.A., Lux M.M., Rauh C., Willner M., Eder I., et al. Lymphedema in breast cancer survivors: Assessment and information provision in a specialized breast unit. Patient Education and Counseling. 2007. 66:311–318.
5. Bennett J.A., Winters-Stone K., Nail L. Conceptualizing and measuring physical functioning in cancer survivorship studies. Oncology Nursing Forum. 2006. 33:41–49.
6. Chun M.S., Moon S.M., Lee H.J., Lee E.H., Song Y.S., Chung Y.S., et al. Arm morbidity after breast cancer treatments and analysis of related factors. The Journal of the Korean Society for Therapeutic Radiology and Oncology. 2005. 23:32–42.
7. Clark B., Sitzia J., Harlow W. Incidence and risk of arm oedema following treatment for breast cancer: A threeyear follow-up study. Monthly Journal of the Association of Physicians. 2005. 98:343–348.
8. Erickson V.S., Pearson M.L., Ganz P.A., Adams J., Kahn K.L. Arm edema in breast cancer patients. Journal of the National Cancer Institute. 2001. 93:96–111.
9. Fu M.R., Axelrod D., Haber J. Breast-cancer-related lymphedema: Information, symptoms, and risk-reduction behaviors. Journal of Nursing Scholarship. 2008. 40:341–348.
10. Fu M.R., Chen C.M., Haber J., Guth A.A., Axelrod D. The effect of providing information about lymphedema on the cognitive and symptom outcomes of breast cancer survivors. Annals of Surgical Oncology. 2010. 17:1847–1853.
11. Jeffs E. Treating breast cancer-related lymphoedema at the London Haven: Clinical audit results. European Journal of Oncology Nursing. 2006. 10:71–79.
12. Lee K.H. Post-operative morbidity, menopause symptoms and quality of life in patients with breast cancer. 2006. Seoul: Yonsei University;Unpublished master's thesis.
13. Lee K.W., Kim S.B., Yoon K.S., Kwak H., Cho S.H., Park J.M., et al. The risk factors associated with lymphedema after axillary dissection for breast cancer. Journal of the Korean Surgical Society. 2006. 71:85–90.
14. McNeely M.L., Campbell K., Ospina M., Rowe B.H., Dabbs K., Klassen T.P., et al. Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Database of Systematic Reviews (Online). 2010. 16(6):CD005211.
15. Meneses K.D., McNees M.P. Upper extremity lymphedema after treatment for breast cancer: A review of the literature. Ostomy/Wound Management. 2007. 53:16–29.
16. Moffatt C.J., Franks P.J., Doherty D.C., Williams A.F., Badger C., Jeffs E., et al. Lymphoedema: An underestimated health problem. Monthly Journal of the Association of Physicians. 2003. 96:731–738.
17. National Cancer Information Center. The occurrence of cancer incidence trends 1999-2007. 2010. Retrieved December 5, 2010. from http://www.cancer.go.kr/cms/statics/incidence/index.html.
18. Position statement of the National Lymphedema Network. Topic: Lymphedema risk reduction practices. National Lymphedema Network. 2008. Retrieved April 30, 2009. from http://www.lymphnet.org.
19. Norman S.A., Localio A.R., Potashnik S.L., Simoes Torpey H.A., Kallan M.J., Weber A.L, et al. Lymphedema in breast cancer survivors: Incidence, degree, time course, treatment, and symptoms. Journal of Clinical Oncology. 2009. 27:390–397.
20. Paskett E.D., Naughton M.J., McCoy T.P., Case L.D., Abbott J.M. The epidemiology of arm and hand swelling in premenopausal breast cancer survivors. Cancer Epidemiology, Biomarkers and Prevention. 2007. 16:775–782.
21. Park J.H. Predictors of breast cancer lymphedema. 2005. Seoul: Yonsei University;Unpublished master's thesis.
22. Poage E., Singer M., Armer J., Poundall M., Shellabarger J. Demystifying lymphedema: Developing of the lymphedema Putting Evidence Into Practice®Card. Clinical Journal of Oncology Nursing. 2008. 12:951–964.
23. Ridner S.H. Breast cancer lymphedema: Pathophysiology and risk reduction guidelines. Oncology Nursing Forum. 2002. 29:1285–1293.
24. Thomas-MacLean R., Miedema B., Tatemichi S.R. Breast cancer-related lymphedema: Women's experiences with an underestimated condition. Canadian Family Physician Médecin de Famille Canadien. 2005. 51:206–208.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download