Abstract
Purpose
Skin-sparing mastectomy with immediate reconstruction provides psychological satisfaction and a good cosmetic effect for patients with breast cancer. However, this procedure takes longer operation time than mastectomy, and the risk of pulmonary thromboembolism (PTE) and deep vein thrombosis may be increased. The purpose of this study was to evaluate the incidence of PTE.
Methods
Between January and May in 2005, 54 breast cancer patients who underwent skin-sparing mastectomy with immediate transverse rectus abdominalis myocutaneous flap (TRAM) at Asan Medical Center were prospectively investigated according to the clinicopathologic data. Patients were placed in compression stockings on the day of operation, and lung perfusion, inhalation scans,and serum D-dimer assays were performed on the first three postoperative days. If findings were suspicious, we performed embolism computed tomography. We compared patient age, body mass index (BMI), clinical risk factors, operative findings, pathologic results, and the clinical course between PTE patients and non-PTE patients.
Results
There were 9 cases of intermediate probability and 6 cases of high probability for PTE according to lung perfusion and inhalation scans, and they underwent embolism CT. Eleven patients (20.4%) were diagnosed with embolism CT or with lung perfusion and inhalation scans;2 patients were symptomatic and 9 patients were asymptomatic. There was significant difference between PTE and non-PTE patients for age, but none for BMI, clinical risk factors, operation time, serum D-dimer, or stage.
Conclusion
The incidence of PTE after mastectomy with immediate TRAM is relatively high, and a strategy for the prevention and treatment of PTE is required. Although age is a risk factor for PTE on this study, future studies are needed to determine the risk factors for and to confirm proper treatment and prevention of PTE.
Figures and Tables
Fig 1
Study Design. USG= Ultrasonography; LMMH= low molecular weight heparin; CT= Pulmonary Embolism Computerized Tomography.

Fig 2
Lung perfusion and inhalation scan of high-probability pulmonary embolism patients: a)Large sized V/Q mismatched perfusion defect in medial segment of right middle lobe and posterior segment of right upper lobe in perfusion scan. b)Computerized-Tomgraphy finding of pulmonary embolism: pulmonary thromboembolism involving right upper pulmonary artery.

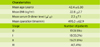
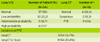
Table 3
Clinicopathologic charateristics of pulmonary thromboembolism patients .

BMI= Body Mass Index; Risk Factor= Diabetes Mellitus, Hypertension, Smoking, Alcohol, Hormone Replacement Therapy; OP=operation, LVI= Lymphovascular invasion; PTE= Pulmoanry Thromboembolism; LMWH= Low Molecular Weight Heparin; NC= Not Checked DVT= Deep Vein Thrombosis; Tx= treatment; Intermediate= Intermediate Probability; High= High probability.
References
1. Grazer FM, Goldwyn RM. Abdominoplasty assessed by survery with emphasis on complications. Plast Reconstr Surg. 1977. 59:513–517.
2. Rosendaal FR. Venous thrombosis: multicausal disease. Lancet. 1999. 353:1167–1173.
3. Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003. 107:I9–I16.

4. Heit JA, Silverstein MD, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ 3rd. Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med. 2000. 160:809–815.

5. White RH, Zhou H, Romano PS. Incidence of symptomatic venous thromboembolism after different elective or urgent surgical procedures. Thromb Haemost. 2003. 90:446–455.

6. Luzzatto G, Schafer AI. The prethrombotic state in cancer. Semin Oncol. 1990. 17:147–159.
7. Levine MN. Prevention of thrombotic disorders in cancer patients undergoing chemotherapy. Thromb Haemost. 1997. 78:133–136.

8. Lee AY, Levine MN. The thrombophilic state induced by therapeutic agents in the cancer patient. Semin Thromb Hemost. 1999. 25:137–145.

9. ENOXACAN study group. Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep vein thrombosis in elective cancer surgery: a double-blind randomized multicentre trial with venographic assessment. Br J Surg. 1997. 84:1099–1103.
10. Weiss RB, Tormey DC, Holland JF, Weinberg VE. Venous thrombosis during multimodal treatment of primary breast carcinoma. Cancer Treat Rep. 1981. 65:677–679.
11. Levine MN, Gent M, Hirsch J, Arnold A, Goodyear MD, Hryniuk W, et al. The thrombogenic effect of anticancer drug therapy in women with stage II breast cancer. N Eng J Med. 1988. 318:404–407.

12. Saphner T, Tormey DC, Gray R. Venous and arterial thrombosis in patients who received adjuvant therapy for breast cancer. J Clin Oncol. 1991. 9:286–294.

13. Goodnough LT, Saito H, Manni A, Jones PK, Pearson OH. Increased incidence of thromboembolism in stage IV breast cancer patients treated with a five-drug chemotherapy regimen. A study of 159 patients. Cancer. 1984. 54:1264–1268.

14. Dismuke SE, Wagner EH. Pulmonary embolism as a cause of death: The changing mortality in hospitalized patients. JAMA. 1986. 255:2039–2042.

15. Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW, et al. Prevention of venous thromboembolism. Chest. 2004. 126:338S–400S.

16. Caine GJ, Stonelake PS, Rea D, Lip GY. Coagulopathic complication in breast cancer. Cancer. 2003. 98:1578–1586.
17. Clahsen PC, van de Velde CJ, Julien JP, Floiras JL, Mignolet FY. Thromboembolic complication after perioperative chemotherapy in women with early breast cancer: a European Organization for Reseach and Treatment of Cancer Breast Cancer Cooperative Group Study. J Clin Oncol. 1994. 12:1266–1271.

18. Yap KP, McCready DR. Deep Vein Thrombosis and maliganancy: A Surgical Oncologist\'s Perspective. Asian J Surg. 2004. 27:249–254.
19. Scientific committee for national survey of acute pulmonary thromboembolism. Korean academy of tuberculosis and respiratory Disease. The national survey of acute pulmonary thromboembolism in Korea. Tuberc Respir Dis. 2003. 54:5–14.
20. Khushal A, Quinlan D, Alikhan R, Gardner J, Bailey C, Cohen A. Thromboembolic disease in surgery for malignancy-rationale for prologed thromboprophylaxis. Seminars in Thrombosis and Hemostasis. 2002. 28:569–576.

21. Olsson EH, Tukiainen E. Three-years evaluation of late breast reconstruction with a free transverse rectus abdominalis musculocutaneous flap in a county hospital in Sweden: A retrospective study. Scand J Plast Reconstr Surg Hand Surg. 2005. 39:33–38.

22. Erdmann D, Sundin BM, Moquin KJ, Young H, Georgiade GS. Delay in unipedicled TRAM flap reconstruction of the breast: a review of 76 consecutive cases. Plast Reconstr Surg. 2002. 110:762–767.

23. Sullivan SD, Kahn SR, Davidson BL. Borris L, Bossuyt P, Raskob G. Measuring the outcomes and pharmacoeconomic consequences of venous thromboembolism prophylaxis in major orthopaedic surgery. Pharmacoeconomics. 2003. 21:477–496.

24. Egermayer P, Town GI. The clinical significance of pulmonary embolism: uncertainties and implication for treatment-a dabate. J Intern Med. 1997. 241:5–10.

25. Kaper DL, Harrison TR. Harrison's principles of internal medicine. Pulmonary Thromboembolism. 2005. 16th ed. New York: McGraw-Hill, Medical Pub. Division;1561–1565.
26. Tetalman MR, Hoffer PB, Heck LL, Kunzmann A, Gottschalk A. Perfusion lung scans in normal volunteers. Radiology. 1973. 106:593–594.
27. Bergqvist D, Agnelli G, Cohen AT, Eldor A, Nilsson PE, Le Moigne-Amiani A, et al. Duration of prophylaxis against venous thromboembolism with enoxaparin after surgery for cancer. N Engl J Med. 2002. 346:975–980.

28. van Rossum AB, Pattynama PM, Ton ER, Treurniet FE, Arndt JW, van Erk B. Pulmonary embolism: validation of spiral CT angiography in 149 patients. Radiology. 1996. 201:467–470.

29. Hyers TM, Agnelli G, Hull RD, Morris TA, Samama M, Tapson V, et al. Antithrombotic therapy for venous thromboembolitic disease. Chest. 2001. 119:176S–193S.
30. Korea central cancer registry. 2002 annual report of the korean central cancer registry. 2003. Gwacheon: Ministry of Health and Welfare;Republic of Korea.
31. Korean Breast. Nationwide breast cancer data of 2002 in Korea. J Kor Breast Cancer Soc. 2004. 7:72–83.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download