A 59-year-old Japanese female patient presented with painless pigment deposition and diffuse enlargement of the left nipple. The nevus had grown slowly for approximately 3 years, at which time the patient was admitted to our institution. She had no history of breast trauma. The patient had contracted hepatitis type B at 30 years of age. She had no remarkable family history. A physical examination revealed a soft, elastic, pedunculated nodule located on the left nipple (
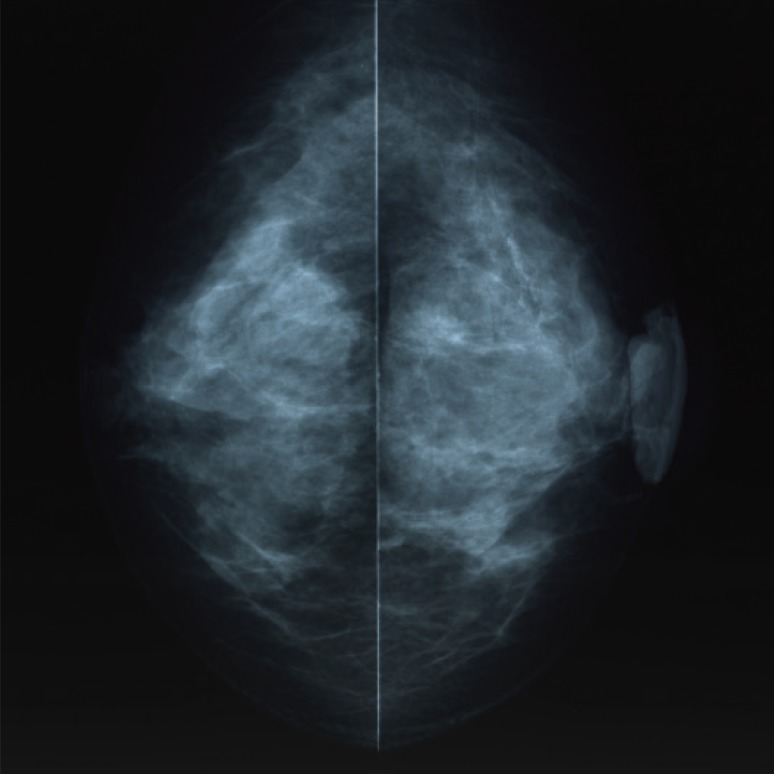
Figure 1). The tumor size was 4.0 cm×3.5 cm×1.5 cm. There were no palpable masses in the breast. The nipple discharge was bloody. There were no palpable axillary or supraclavicular lymph nodes. Dermoscopy revealed an asymmetrical, irregularly structured area accompanied by a 12-mm-thick ulceration, and a blue-whitish veil. The clinical course suggested malignant melanoma, rather than mammary Paget's disease. All laboratory data were unremarkable except for a slightly elevated lactate dehydrogenase level. Regarding tumor markers, the levels of carcinoembryonic antigen and cancer antigen 15-3 were within normal ranges, whereas those of neuron-specific enolase and 5-S-cysteinyldopa were elevated (13.7 ng/mL and 32.1 nmol/L, respectively). Mammography showed a lobulated mass with a well-circumscribed margin in the left nipple (
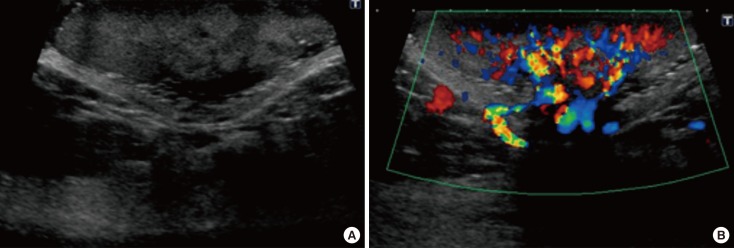
Figure 2). Ultrasonography showed a hypoechoic mass with a lobular shape that measured 4.0 cm×3.5 cm. Internally, the mass was heterogeneously echoic, and color Doppler ultrasound demonstrated a strong increase in blood flow within the lesion (
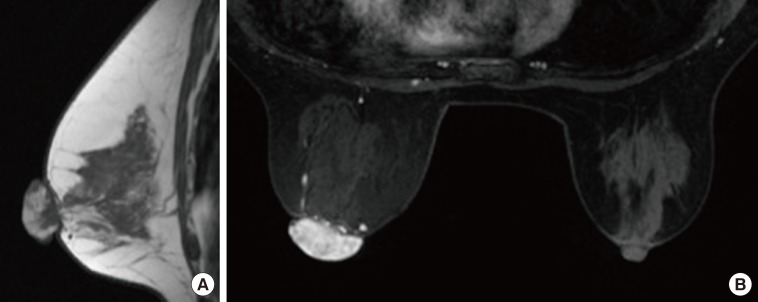
Figure 3). Magnetic resonance imaging showed a heterogeneously distributed lesion with high signal intensity in the left nipple on both T1-weighted and T2-weighted images (
Figure 4A). The mass in the nipple was rapidly enhanced following the injection of gadolinium diethylenetriaminepentaacetic acid, and the time-intensity curve showed a rapid plateau pattern (
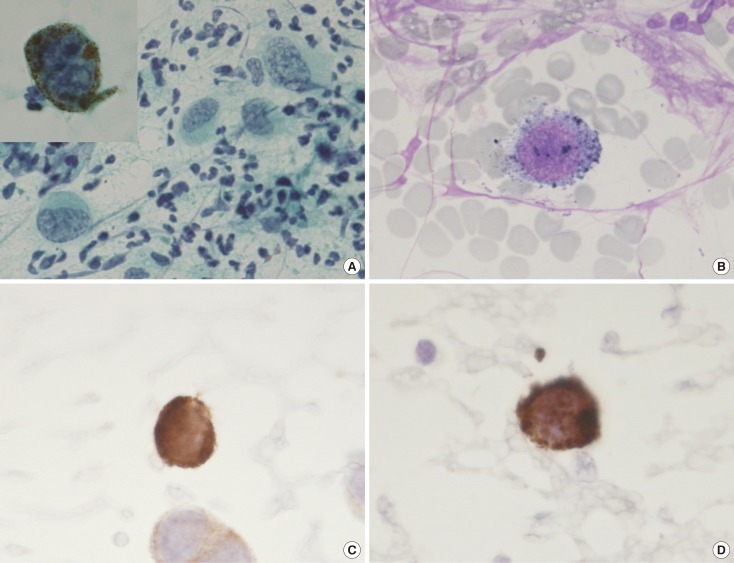
Figure 4B). No other enhanced lesion was detected in the breast area. Positron emission tomography/computed tomography (PET/CT) revealed a lesion with high 18F-fluorodeoxyglucose only in the left nipple. Exfoliative cytology of the left nipple and using Papanicolaou and Giemsa staining revealed anaplastic cells (melanocytes) with intranuclear cytoplasmic invaginations and prominent nucleoli (
Figure 5A and 5B). These melanocytes also exhibited strong mmunohistochemical reactions to Melan-A and HMB45, which are highly specific for melanoma cells (
Figure 5C and 5D). These findings suggested a very thick nodular malignant melanoma. The patient underwent a mastectomy resection of the left breast. A left-sided sentinel lymph node biopsy revealed an axillary lymph node metastasis, and an axillary lymph node dissection was performed. Macroscopically, the resected specimen revealed a pigmented tumor measuring approximately 4.5 cm×3.2 cm×2.0 cm (
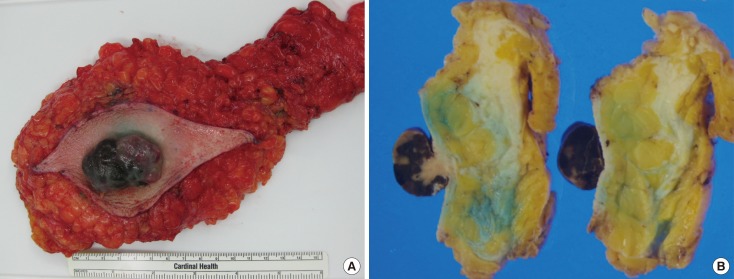
Figure 6). A histological analysis revealed high cellularity, with plump cells containing prominent and pleomorphic nucleoli. The cytoplasm was filled with compact melanosomes. Numerous atypical melanocytes were also observed in the connective tissue (
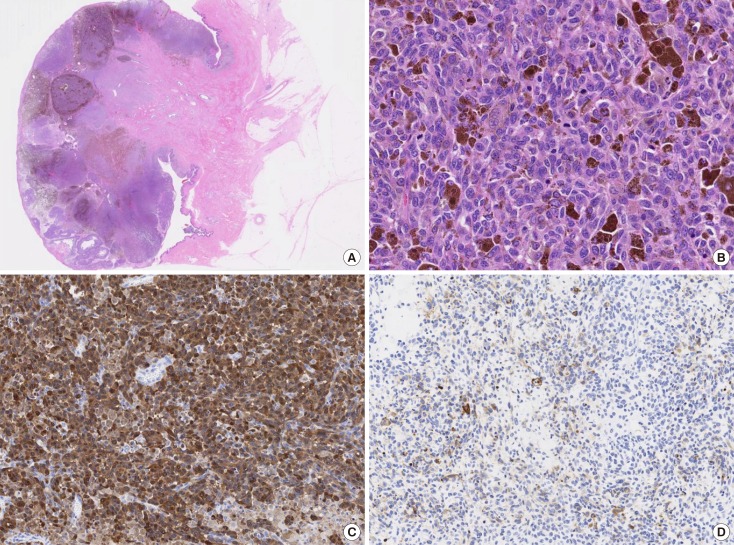
Figure 7A and 7B). Breslow's tumor thickness was 12 mm, which suggested Level IV according to the Clark level of invasion. Strong immunohistochemical reactions for S100 protein and HMB45, a marker of melanocytic neoplasms, confirmed the diagnosis (
Figure 7C and 7D). Based on these features, a pathological diagnosis of nodular malignant melanoma was made. Metastasis was identified in the left axillary lymph nodes, and a AJCC/UICC stage of IIIC, T4bN1bM0 was confirmed. The surgical margin was pathologically negative. The patient was given postoperative chemotherapy (DAV-Feron [dacarbazine, nimustine, vincristine, and interferon-β] and subsequent interferon). A lung nodule detected by computed tomography 2 years after surgery was subjected to careful follow-up. The size of the lung nodule did not change for 5 years, and was deemed benign. There has been no evidence of recurrence after 7 years of surgery.
 | Figure 1Gross finding. An elastic soft pedunculated nodule located on the left nipple.
|
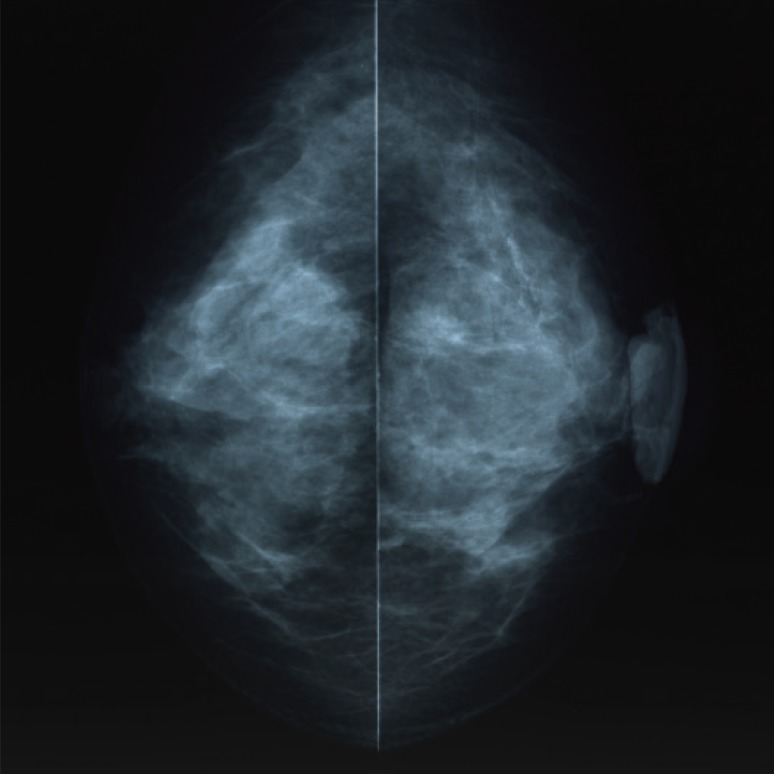 | Figure 2Mammography examination of the left breast. The craniocaudal view mammogram showed a lobulated mass in the left nipple.
|
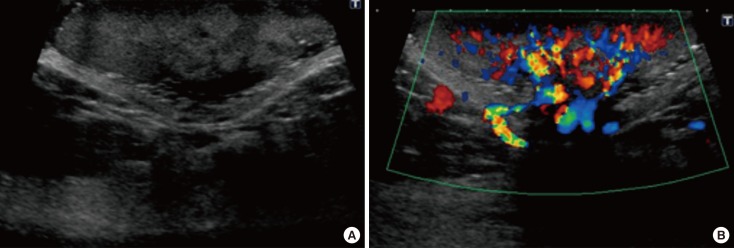 | Figure 3Ultrasonography (US) examination. (A) US showed a hypoechoic mass with a lobular shape. (B) The color Doppler ultrasound demonstrated highly increased blood flow within the lesion.
|
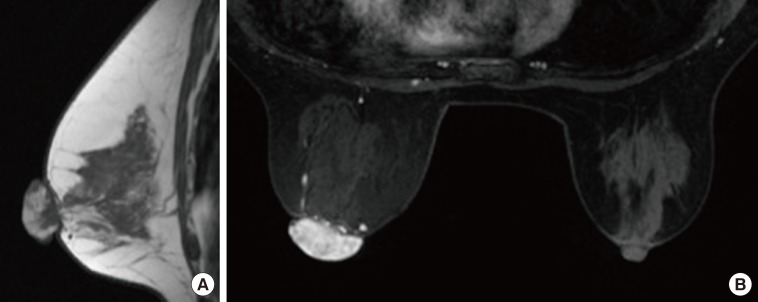 | Figure 4Magnetic resonance imaging (MRI). (A) MRI showed the heterogeneously distributed lesion of the high signal intensity in the left nipple on T1-weighted images. (B) The mass of the nipple was enhanced quickly following the injection of gadolinium diethylenetriamine-pentaacetic acid at early phase (2 minutes after A B agent injection).
|
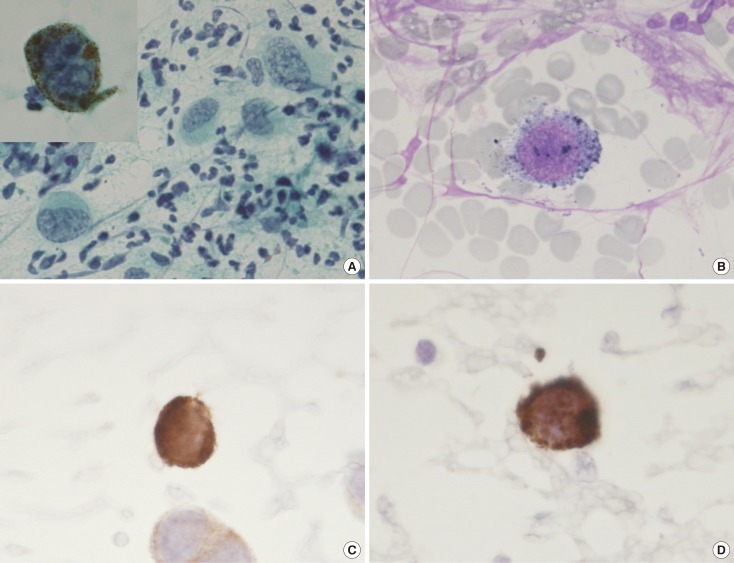 | Figure 5Exfoliative cytology of the left nipple. The anaplastic cells with intranuclear cytoplasmic invaginations, and the prominent nucleoli can be seen using (A) Papanicolaou stain (×400; inset, ×1,000) and (B) Giemsa stain (×1,000). These melanocytes also revealed strong immunohistochemical reactions for (C) Melan-A (×1,000) and (D) HMB45 (×1,000).
|
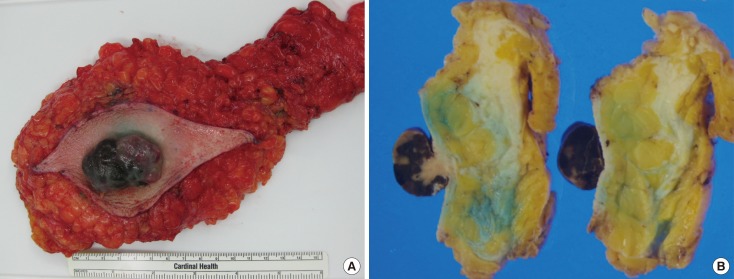 | Figure 6Gross appearance of the mastectomy specimen. (A) The resected specimen revealed a black color tumor. (B) The cut slice through the nipple of the mastectomy specimen.
|
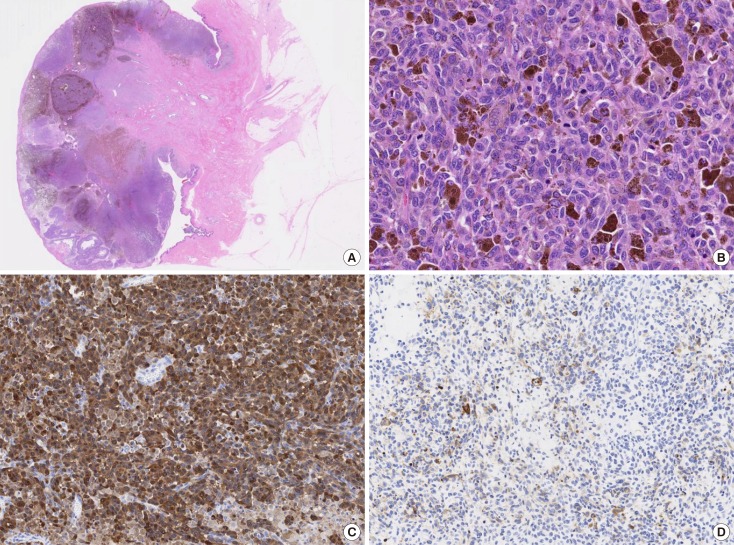 | Figure 7Histopathologic findings. (A) Microscopic findings revealed numerous atypical melanocytes in the connective tissue (H&E stain, low magnification view). (B) The cytoplasm was filled with compact melanosomes (H&E stain, ×200). The immunohistochemistry image for (C) S100 protein (×100) and (D) HMB45 (×100) were strongly positive.
|




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download