Abstract
Purpose
Breast volume assessment is one of the most important steps during implant-based breast reconstruction because it is critical in selecting implant size. According to previous studies, there is a close relationship between the mastectomy specimen weight and resected breast volume. The aim of this study was to evaluate long-term patient satisfaction with implant-based breast reconstruction guided by the ratio of implant volume to mastectomy specimen weight. In doing so, we describe the ideal ratio for patient satisfaction.
Methods
A total of 84 patients who underwent implant-based breast reconstruction for breast cancer were included in this study. The patients were grouped by the ratio of implant size to mastectomy specimen weight (group 1, <65%; group 2, 65%–75%; and group 3, >75%). Outcome analysis was performed using a questionnaire of patient satisfaction and the desired implant size.
Results
Patient satisfaction scores concerning the postoperative body image, size, and position of the reconstructed breast were significantly higher in group 2. The average ratio of the ideal implant volume to mastectomy specimen weight for each group was 71.9% (range, 54.5%–96.7%), with the differences across the three groups being not significant (p=0.244).
Conclusion
Since there is an increase in breast reconstruction, selecting the appropriate breast implant is undoubtedly important. Our novel technique using the ratio of implant volume to mastectomy specimen weight provides physicians a firm guide to intraoperative selection of the proper implant in reconstructive breast surgery.
The demand for postmastectomy reconstruction of breast tissue following cancer is increasing worldwide [1]. Approximately 18% to 25% of patients who receive a mastectomy undergo breast reconstruction [23]. The breast reconstruction methods vary, including the use of autologous tissue, prosthetic material, or a combination of the two [4]. Deciding which method to use involves multiple factors, such as patient preference, risk factors, and physical characteristics [2]. While autologous tissue reconstruction using a transverse rectus abdominis musculocutaneous flap is one of the gold standards for breast reconstruction, the increasing use of a tissue expander or implant-based reconstruction represent additional reasonable methods [5]. A two-stage procedure that involves tissue expansion with a temporary expander, followed by replacement with a permanent implant, is a safe and popular method of reconstruction [6]. Today, immediate implant reconstruction is also a well-accepted reconstruction method. Approximately 15% to 20% of breast reconstructions are performed with this technique [7]. The ideal candidate for implant-based reconstruction is a slim patient who requires bilateral reconstruction or a slim patient with small, minimally ptotic breasts and sufficient soft tissue who requires unilateral reconstruction [58]. The physician must consider sufficiency and quality of soft tissue coverage, symmetry of inframammary folds, and implant position and size to achieve suitable aesthetic result of implant-based breast reconstruction. Among these factors, proper implant size selection is undoubtedly crucial in achieving satisfactory aesthetic result of reconstruction [9]. Preoperative breast volume measurement is a determining factor for selecting implant size that closely matches the contralateral breast [1011]. Furthermore, mastectomy specimen weight is proportionate to the volume required to fill the residual defect [11]. This weight measurement enables the reconstructive surgeon to select the appropriate implant. Spear and Spittler [5] have reported that mastectomy specimen weight in grams correlates with the volume of the selected implant in cubic centimeters and should serve as important information. We assumed that the selected implant volume is closely associated with mastectomy specimen weight and hypothesized that there is an ideal ratio of implant volume to mastectomy specimen weight. The aim of this study was to evaluate long-term patient satisfaction with implant breast reconstruction associated with the ratio of implant volume to mastectomy specimen weight.
Between 2004 and 2012, 84 patients who were treated with postmastectomy breast reconstruction using an implant at a single institution were surveyed retrospectively. The reconstructions included a two-stage procedure that involved the insertion of a tissue expander followed by an implant after a few months (n=69) and a one-stage method of immediate insertion of the implant at the time of mastectomy (n=15). The two-stage reconstructions were performed on patients who underwent total mastectomy, while the immediate implant reconstructions were performed on those who underwent nipple or skin sparing mastectomy. In tissue expander cases, the permanent implants were inserted about three months after the initial operation. Tissue expanders or permanent silicone implants were placed with the assistance of an acellular dermal matrix (ADM). The ADM was fixed on the lower margin of the origin of the dissected pectoralis major muscle on the superior side and connected to the serratus anterior muscle on the lateral side, as well as to the chest wall on the medial and inferior side. This created a supportive pocket for expander or implant placement against the chest wall. The ADMs used in this study were AlloDerm® (LifeCell Corp., Branchburg, USA) and CGDerm® (CGBio Corp., Seoul, Korea).
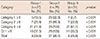
Patients who underwent immediate and unilateral reconstructions were included in this study, while those who underwent delayed or bilateral reconstructions were not. We also excluded patients who underwent simultaneous contralateral breast reduction, mastopexy, and augmentation because we planned to analyze patient satisfaction with the reconstructed breast compared to the contralateral (intact) breast. The independent clinical variables obtained by review of medical records included patient age, weight, height, stage of breast cancer, and history of radiation or chemotherapy (Table 1).
Patients were either contacted by telephone or interviewed in person at our outpatient clinic. We developed a new questionnaire for this study. The questionnaire contained 11 rating scale questions (0–10 scale) and one subjective question, and required approximately 10 minutes to complete. The rating scale contained three categories to determine patient satisfaction with (1) postoperative body image, (2) size and position of the reconstructed breast compared to the intact one, and (3) the breast reconstruction procedure itself (Supplementary Table 1, available online). All procedures were performed by three other plastic surgeons who did not participate in the reconstruction (response rate, 75.0% [84/112]).
The patients were grouped based on their ratio of implant volume to mastectomy specimen weight (group 1, <65%; group 2, 65%–75%; and group 3, >75%) and type of reconstruction (expander+implant vs. immediate implant). Data analysis was performed using SAS version 9.2 (SAS Institute Inc., Cary, USA). Patient satisfaction in each group was compared using a one-way analysis of variance. Values were expressed as the mean±standard deviation, and the significance level was set at p<0.05. We considered scores of 8 or greater for rating scale questions as “excellent” satisfaction. The comparison and trend of “excellent” satisfaction rates for different ratios of implant volume to specimen weight were analyzed using Youden's index. This study was approved by the Institutional Review Board of Yonsei University (IRB number: 3-2016-0038) and was conducted in accordance with the Declaration of Helsinki.
Of 84 patients, the mean age was 43.0±9.3 years and the average body mass index was 21.1±2.2. The mean implant size was 275.3±55.2 mL, and the mean mastectomy specimen weight was 386.6±116.2 g. The mean ratio of implant size to mastectomy specimen weight was 75.5±22.2. The mean follow-up period was 3.1±2.6. Sixty-nine patients (82.1%) underwent expander+implant breast reconstruction, and the remaining 15 (17.9%) underwent immediate implant reconstruction (Table 1).
The patients were divided, based on their ratio of implant volume to mastectomy specimen weight, into group 1 (n=25), group 2 (n=28), or group 3 (n=31), for which the average specimen weights were 479.2±114.2 g, 390.5±81.7 g, and 308.5±86.4 g, respectively. The specimen weights of group 1 were generally heavier than those of the other groups (p<0.001). The average implant volume of each group was 267.1±54.8 mL, 273.3±56.9 mL, and 283.7±54.7 mL, respectively (p=0.613). The mean ratios were 56.2%±6.2%, 70.0%± 3.1%, and 96.1%±23.4%, respectively. Demographic data were similar between the three groups, except for weight (Table 2). Among the groups, the patient satisfaction scores were generally higher in group 2 than in the other groups. The mean satisfaction score regarding postoperative body image (category 1, questions Q1–Q5) was 8.9±0.9 in group 2, which was significantly higher than that in the other groups (p<0001). The mean score of Q1 was the highest in the first category. The scores involving standing position (Q2 and Q3) were higher than those involving supine position (Q4 and Q5), regardless of whether the patient was wearing a brassiere. We assumed that these results were due to the character of a reconstructed breast, which is less ptotic and more prominent when lying down. The patients in group 2 were more satisfied with the size or position of the reconstructed breast than were patients in the other groups (category 2, p<0.001) and reconstruction itself (category 3, p=0.005). In addition, we asked a subjective question about the ideal reconstructed breast size compared to their existing one (Q12). The patients in group 1 wanted larger implants by a mean 23.2%±13.5%, but those in group 3 wanted smaller implants by mean 21.1%±11.2%. Meanwhile, the ideal implant size requested by group 2 was similar to the existing breast (1.4%±5.9%). Based on these results, we calculated that the ratio of ideal implant volume to mastectomy specimen weight for each group was 71.9%±11.8%, with the differences across the three groups being insignificant (p=0.244) (Table 3, Figure 1).
We considered scores of 8 or greater as indicating “excellent” satisfaction. In group 2, the proportion with an average score of 8 or greater was 96.4%. In contrast, the percentages of patients indicating “excellent” satisfaction were 29.6% in group 1 and 25.8% in group 3 (p<0.001) (Table 4). We also used Youden's index (J) to determine the upper and lower margins of the ratio that result in a predictable “excellent” satisfaction for a patient. J is formally defined as “J=sensitivity+specificity–1.” The cutoff value that achieved maximum J was used to find the ratio (implant volume to specimen weight) of the predictable greatest satisfaction. In category 1, the maximum J was 0.5769 (sensitivity, 1.0; specificity, 0.5769) when the ratio was 76.9%. The odd ratio (OR) at this ratio was 0.064 (95% confidence interval, 0.004–0.998). This implies that when the ratio is more than 76.9%, the possibility of excellent satisfaction decreases by a factor of 0.064. When the ratio is less than 76.9%, the possibility of excellent satisfaction is increased. The cutoff values of category 2 and Q11 were 76.9% and 80.0%, respectively. A ratio of less than 76.9% in category 2 and 80.0% in Q11 increased the possibility of “excellent” satisfaction among patients. However, in category 3, the cutoff value was 61.1%, and the OR at this ratio was 1.65. This implies that when the ratio was greater than 61.1%, the possibility of “excellent” satisfaction among patients increased. Based on these results, we predicted that a ratio of implant volume to mastectomy specimen weight of 61.1% to 76.9% increases the possibility of excellent satisfaction. This range matched the range of group 2 (65.0%–75.0%), which showed the greatest patient satisfaction.
Breast reconstruction is now widely considered to be an important component of the treatment of breast cancer [1]. During this process, the principle aesthetic objective is the restoration of volumetric symmetry [12]. Accurate volume assessment is a prerequisite in breast reconstruction and provides a guideline for implant size selection. Although breast volume assessment is undoubtedly important, it is not conducted routinely in some institutions because of the absence of a commonly accepted standard method [101213141516171819].
There are numerous techniques for preoperative and intraoperative estimation of implant size, but most are inaccurate and inconsistent [9]. Moreover, this estimation depends on the surgeon's experience, skill, and surgical ability in many cases. According to previous studies, preoperative estimation techniques include anthropometric volume estimation and volumetric analysis using ultrasonography, mammography, computed tomography, magnetic resonance imaging, and three-dimensional scanners [131819202122]. Although these exams may occur during the cancer staging workup, they require other specialized staff, including radiographers and radiologists [9]. Furthermore, the thickness of the remnant skin envelop after mastectomy cannot be estimated preoperatively using these tests. Intraoperative estimation techniques include “implant sizers method” and “gauze swab implant-estimation method [9].” While using an implant sizer is a commonly available method, it is expensive [9]. Moreover, it has different characteristics compared to a permanent implant, which can result in intraoperative trial and error [9]. Caulfield and Niranjan [9] used surgical gauze swabs and reported that the “gauze swab implant-estimation method” is an easily reproducible and inexpensive method that produces reliable results. However, the sizes and characteristics of gauzes differ across manufacturers, thereby complicating the process of estimating the volume of a saline-soaked gauze swab, which is used as an intraoperative “trial sizer.” It is also possible to mistakenly leave gauze inside the breast when using this method.
Thus, we introduced a novel technique of using mastectomy specimen weight to select implant size. Although selecting breast implant size according to removed breast volume (mastectomy specimen volume) may be the most accurate method, it is more difficult and time-consuming to assess the specimen volume instead of weight, intraoperatively. Several studies have clarified the close relationship between mastectomy specimen weight and resected breast volume, and thus we decided to use specimen weight in this study [2324].
We surveyed patient satisfaction with an original questionnaire and analyzed the ideal reconstructed breast size that patients desired. By analyzing the ideal volume, we calculated the new ratio (the ratio of ideal implant volume to mastectomy specimen weight), and found that 72.6% (61/84) of new ratios in patients were 65% to 75% (Figure 1). We hypothesized that a 65% to 75% ratio of implant size to mastectomy specimen weight will lead to symmetric and aesthetically pleasing results, which is supported by questionnaire scores (Table 3). A ratio of 65.0% to 75.0% is preferable over 100% because of density differences between the implant and the specimen. Furthermore, since general surgeons remove the tail portion of the breast as well as the body of the breast, the implant that does not cover the tail should be smaller than the total specimen weight. Thus, we thought that the implant volume should be smaller than the specimen weight, yet large enough to fulfill the symmetry of bilateral breasts, and such implants resulted in the greatest level of satisfaction among participants of group 2. We also think that such a ratio, which was not too large, produced a satisfactory shape and natural form while allowing for movement.
Interestingly, in operations with greater specimen weights, the operator chose an implant of lesser ratio. We believe that in cases of large specimen weights, other variables, such as the breast width and height, restricted the choices of implants and, thus, smaller ratios. In addition, one can see that the specimen weight range was quite wide for each group, and so, it is difficult to definitively state that patients with large specimen weights used small implants. Nevertheless, the patient survey showed the greatest level of satisfaction in group 2, and we carefully concluded that a ratio between 65.0% and 75.0% produced the greatest level of patient satisfaction. Therefore, choosing an implant volume using specimen weight and size as guides is a powerful method. We do acknowledge that such a ratio is quite specific to our institute with a consistent style of general surgeons, yet this will provide a helpful guide to the general rules of reconstruction and other institutes, where surgeons can establish specific ratios unique to their environment.
For breast surgeons, the most difficult, but most important, goal is achieving symmetry during breast reconstruction. Every person has a unique shape and volume, with even the breasts of a single person differing. Although implants have variations in styles and sizes, they cannot meet the unique circumstances and needs of each patient. While base width and projection are important, choosing implants based on natural projection sometimes results in an insufficient volume. There are many variables to consider and, in this study, we mainly focused on specimen weight and ratio. Although shape and other factors are important, we believe that volume is a more critical factor to patient satisfaction. This is because fixed implant styles are limited in matching the exact shape of the contralateral side; however, when wearing a brassier, a similar volume confers a stable feeling of symmetry and great satisfaction on the patient.
This study has several limitations. First, the follow-up period was shorter in group 2 (2.2±2.3 years) than in the other groups (group 1, 3.2±2.7 years; group 3, 3.7±2.6 years). This difference can affect patient satisfaction and aesthetic outcome. Hu et al. [25] reported that satisfaction with a reconstructed breast including appearance, shape, softness, size, and projection, diminished by the time of long-term follow-up (>8 years). Because the mean follow-up period of all groups was shorter than 8 years, patient satisfaction may decrease in the future. Second, we created a survey focusing on the size and position of the reconstructed breast; however, other factors, such as rippling and capsular contracture, may affect satisfaction as well. Moreover, ancillary procedures, such as autologous fat injection, inframammary fold repositioning, and scar revision, which are performed along with nipple-areolar complex reconstruction, may have affected patient satisfaction. In addition, the density differences between implant and specimen as well as between the specimens among patients may have affected the results. In the future, a large-scale study with more subdivided groups and a long-term follow-up period is necessary. Despite the few limitations, to our knowledge, this is the first report of patient satisfaction analysis involving the ratio of implant volume to mastectomy specimen weight in breast reconstruction.
In this time of increasing breast reconstruction, selecting the appropriate breast implant is undoubtedly of crucial importance. Our novel technique that makes use of the ratio of implant volume to mastectomy specimen weight provides physicians with a useful guide for intraoperative selection of the proper implant for reconstructive breast surgery.
Figures and Tables
 | Figure 1The ideal new ratio in relation to the original ratio of implant volume to specimen weight. X-axis, the ratio of implant volume to mastectomy specimen weight (%); Y-axis, the new ratio recalculated with the ideal implant volume which patients desired (%). Sixty-one patients (61/84, 72.6%) resulted new ratios located within 65.0% to 75.0%. |
Table 1
Patient characteristics

Table 2
Patient classification based on the ratio of implant volume to mastectomy specimen weight

Table 3
Scores of the questionnaire for each group

Table 4
Rate of excellent satisfaction*
References
1. Tzafetta K, Ahmed O, Bahia H, Jerwood D, Ramakrishnan V. Evaluation of the factors related to postmastectomy breast reconstruction. Plast Reconstr Surg. 2001; 107:1694–1701.

2. Vega S, Smartt JM Jr, Jiang S, Selber JC, Brooks CJ, Herrera HR, et al. 500 Consecutive patients with free TRAM flap breast reconstruction: a single surgeon's experience. Plast Reconstr Surg. 2008; 122:329–339.

3. Duggal CS, Grudziak J, Metcalfe DB, Carlson GW, Losken A. The effects of breast size in unilateral postmastectomy breast reconstruction. Ann Plast Surg. 2013; 70:506–512.

4. Noone RB. Thirty-five years of breast reconstruction: eleven lessons to share. Plast Reconstr Surg. 2009; 124:1820–1827.

5. Spear SL, Spittler CJ. Breast reconstruction with implants and expanders. Plast Reconstr Surg. 2001; 107:177–187.

6. Radovan C. Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg. 1982; 69:195–208.

7. Salzberg CA, Ashikari AY, Koch RM, Chabner-Thompson E. An 8-year experience of direct-to-implant immediate breast reconstruction using human acellular dermal matrix (AlloDerm). Plast Reconstr Surg. 2011; 127:514–524.

8. Roostaeian J, Pavone L, Da Lio A, Lipa J, Festekjian J, Crisera C. Immediate placement of implants in breast reconstruction: patient selection and outcomes. Plast Reconstr Surg. 2011; 127:1407–1416.

9. Caulfield RH, Niranjan NS. Innovative techniques: a novel technique for intraoperative estimation of breast implant size in aesthetic and reconstructive breast surgery. Aesthetic Plast Surg. 2008; 32:126–129.

10. Kayar R, Civelek S, Cobanoglu M, Gungor O, Catal H, Emiroglu M. Five methods of breast volume measurement: a comparative study of measurements of specimen volume in 30 mastectomy cases. Breast Cancer (Auckl). 2011; 5:43–52.

11. Shamoun JM, Hartrampf CR. Mastectomy specimen weight and skin dimensions as an adjunct in breast reconstruction. Ann Plast Surg. 1996; 36:251–254.

12. Yoo A, Minn KW, Jin US. Magnetic resonance imaging-based volumetric analysis and its relationship to actual breast weight. Arch Plast Surg. 2013; 40:203–208.

13. Katariya RN, Forrest AP, Gravelle IH. Breast volumes in cancer of the breast. Br J Cancer. 1974; 29:270–273.

14. Malini S, Smith EO, Goldzieher JW. Measurement of breast volume by ultrasound during normal menstrual cycles and with oral contraceptive use. Obstet Gynecol. 1985; 66:538–541.
15. Fowler PA, Casey CE, Cameron GG, Foster MA, Knight CH. Cyclic changes in composition and volume of the breast during the menstrual cycle, measured by magnetic resonance imaging. Br J Obstet Gynaecol. 1990; 97:595–602.

16. Daly SE, Kent JC, Huynh DQ, Owens RA, Alexander BF, Ng KC, et al. The determination of short-term breast volume changes and the rate of synthesis of human milk using computerized breast measurement. Exp Physiol. 1992; 77:79–87.

17. Ward C, Harrison B. The search for volumetric symmetry in reconstruction of the breast after mastectomy. Br J Plast Surg. 1986; 39:379–385.

18. Bulstrode N, Bellamy E, Shrotria S. Breast volume assessment: comparing five different techniques. Breast. 2001; 10:117–123.

19. Yip JM, Mouratova N, Jeffery RM, Veitch DE, Woodman RJ, Dean NR. Accurate assessment of breast volume: a study comparing the volumetric gold standard (direct water displacement measurement of mastectomy specimen) with a 3D laser scanning technique. Ann Plast Surg. 2012; 68:135–141.
20. Caruso MK, Guillot TS, Nguyen T, Greenway FL. The cost effectiveness of three different measures of breast volume. Aesthetic Plast Surg. 2006; 30:16–20.

21. Palin WE Jr, von Fraunhofer JA, Smith DJ Jr. Measurement of breast volume: comparison of techniques. Plast Reconstr Surg. 1986; 77:253–255.
22. Longo B, Farcomeni A, Ferri G, Campanale A, Sorotos M, Santanelli F. The BREAST-V: a unifying predictive formula for volume assessment in small, medium, and large breasts. Plast Reconstr Surg. 2013; 132:1e–7e.
23. Parmar C, West M, Pathak S, Nelson J, Martin L. Weight versus volume in breast surgery: an observational study. JRSM Short Rep. 2011; 2:87.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download