INTRODUCTION
The management plans are different depending on the pathology results. Immediate action should be taken in the case of concordant malignancy. If discordant benign lesions are obtained, surgical excision should be considered. For the concordant benign lesions, imaging follow-ups are recommended. Although the management plans for initial Breast Imaging Reporting and Data System (BI-RADS) category 4A and 3 are different, biopsy is the first option for initial category 4A, and regular imaging follow-up is preferable for initial category 3; in addition, if the expected cancer detection rates are different, concordant benign lesions obtained from initial category 4A and 3 are treated in the same manner [
1].
Regarding concordant benign lesions, when benign core biopsy was obtained in an expected benign lesion on imaging study [
2], follow-up is mandatory to confirm stability and to avoid possible delayed false-negative results. Many studies have proposed follow-up strategy for the concordant benign lesion [
345]. Youk et al. [
3] suggested beginning US follow-up at a minimum of 12 months if concordant benign lesions were observed after core needle biopsy, and if there were any symptoms, follow-up US should begin earlier, at least 6 months after core needle biopsy. Lee et al. [
4] suggested that follow-up recommendation should be based on the type of benign histologic finding; a 6-month follow-up was recommended for nonspecific results, and an annual follow-up recommended for specific results. A preliminary report by Marcon et al. [
5] showed that a 6-month follow-up might be sufficient to assess the stability of category 3 lesions in young patients.
According to the American College of Radiology's BIRADS (ACR BI-RADS), the likelihood of cancer in category 4A is known to be 2% to 10% and that of category 3 is 0% to 2% [
1]. Although there is a significant difference in the likelihood of cancer between the two groups, previous publications concentrated on mainly pathology results obtained from the biopsy [
345] and any articles dealing with the effect of the initial BI-RADS category have not been released. The purpose of this study was to investigate if the initial category 4A or 3 in concordant benign lesions could affect follow-up compliance.
Go to :

METHODS
This retrospective, single-institution, observational study was approved by the Institutional Review Board of the National Cancer Center of South Korea (IRB number: 2014-0064), and the requirement for informed consent was waived.
Study design
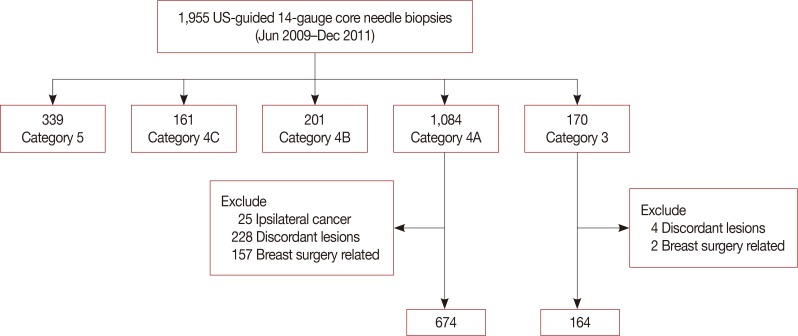
We identified 1,955 cases of consecutive ultrasound-guided, 14-gauge core needle biopsies conducted in 1,787 women (mean age, 44±9.7 years) from June 2009 to December 2011. From these, data for 1,254 lesions (1,084, initial category 4A and 170, initial category 3) were obtained (
Figure 1). Among the 1,084 cases of the initial category 4A group, we excluded 410 cases where surgical removal of ipsilateral breast cancers had been performed simultaneously in the initial category 4A (25 cases), when discordant results such as malignancy or high-risk lesions were obtained (228 cases), and when the initial category 4A lesions were surgically removed with other breast lesions without any pathologic reporting (157 cases). Among the 170 initial category 3 cases, six cases were excluded because of discordant pathology (four cases) and simultaneous surgical removal without any pathologic report about it (two cases). The rest of the 838 lesions (674, category 4A and 164, category 3) of concordant benign results were included in this study (
Figure 1). Concordant benign lesions of initial category 4A group were 674 lesions in 674 patients (mean age, 45.3±9.6 years) and that of category 3 group were 164 lesions in 164 patients (mean age, 43.4±10.1 years).
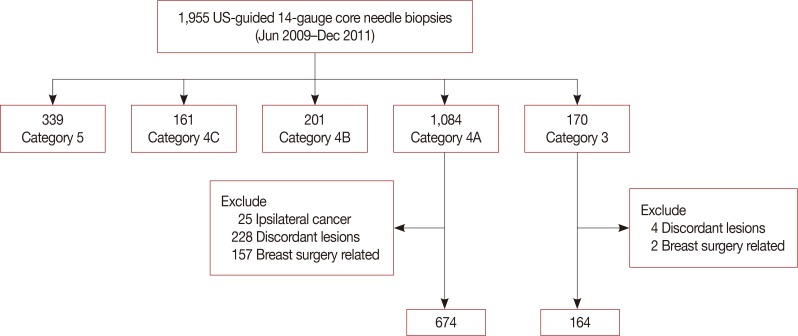 | Figure 1
Flow chart of study population.
US=ultrasound.

|
Biopsy technique
We evaluated breast lesions and assessed the possibility of malignancy based on the BI-RADS-Ultrasound lexicon [
1]. Among them, BI-RADS category 4 or higher lesions were indications for core needle biopsy. On the request of patients or referring physicians, BI-RADS category 3 lesions were referred to undergo core needle biopsy. The freehand technique was used during US-guided gun biopsy, using a 7.5–12 MHz linear array transducer (Philips Advanced Technology Laboratories, Bothell, USA). An automated (TSK Laboratory, Tochigi, Japan) or semi-automated gun (TSK Laboratory) was selected as per the radiologists' preferences. One to four breast radiologists performed US-guided biopsy when the specimen contained four to six core samples per lesion.
Data collection
After biopsy, the decision about concordance or discordance was determined via a consensus conference. A concordance decision meant the pathologic findings provided an appropriate explanation for the imaging abnormality and discordance meant they did not [
2]. If malignant pathology was obtained in category 4B, 4C, and 5, it was considered as concordant malignancy and if benign pathology was obtained in the same categories, it was considered as discordant benign. If malignant pathology was obtained in category 4A and 3, it was considered as discordant malignancy and if benign pathology was obtained in the same categories, it was considered as concordant benign.
If malignancy was found in core needle biopsy, immediate action such as surgery or chemotherapy, were taken. In cases of high-risk lesions (atypical hyperplasia, lobular carcinoma in situ, papillary lesions, phyllodes tumor, mucocele-like lesion, and radial scars), we recommended excisional biopsy through surgical excision or vacuum-assisted devices. For concordant benign lesions, follow-up US after 6 months after biopsy and annually thereafter for minimum 2 years was recommended in either initial category 4A or 3 lesions.
Analysis of follow-up data
If a surgical excision was performed before the next follow-up, we defined it as an immediate surgical excision. We gathered those cases and evaluated the pathologic reports. If the immediate surgical excision was performed, the follow-up was considered to be terminated. Dates of each imaging study, performed subsequent to the initial biopsy, were recorded and grouped into intervals: 6-month follow-up (≤9 months), 12-month follow-up (>9, ≤15 months), and long-term follow-up (>15, ≤36 months). Regarding US follow-up after core needle biopsy, details of the number and the result of follow-up US were comprehensively recorded in both category 4A and 3.
Any changes during follow-up such a development of suspicious findings or progression of previous lesion, the results of additional biopsy performed were recorded. We defined the additional biopsy as performing biopsy in either another newly developed lesion or the same lesion with size enlargement or lesion character changes during the first follow-up.
We evaluated whether the initial category might affect the patients' compliance during the follow-up, in concordant benign lesions with initial category 4A or 3 groups. We also investigated whether additional biopsy rate and the cancer detection rate was related to the initial category, when the patient came for follow-up.
Statistical analysis
Statistical comparisons for the result of first follow-up US compliance and malignant rates among 6-month, 12-month, and long-term intervals were performed by using the chi-square test. A p-value less than or equal to 0.05 was considered to be statistically significant. Kaplan-Meier curves were plotted, and the log-rank test was used to compare the compliance rate in the timing of first follow-up between the two groups, with a significance level of 0.05. All statistical analyses were performed with STATA version 10.0 (StataCorp LP, College Station, USA) software.
Go to :

RESULTS
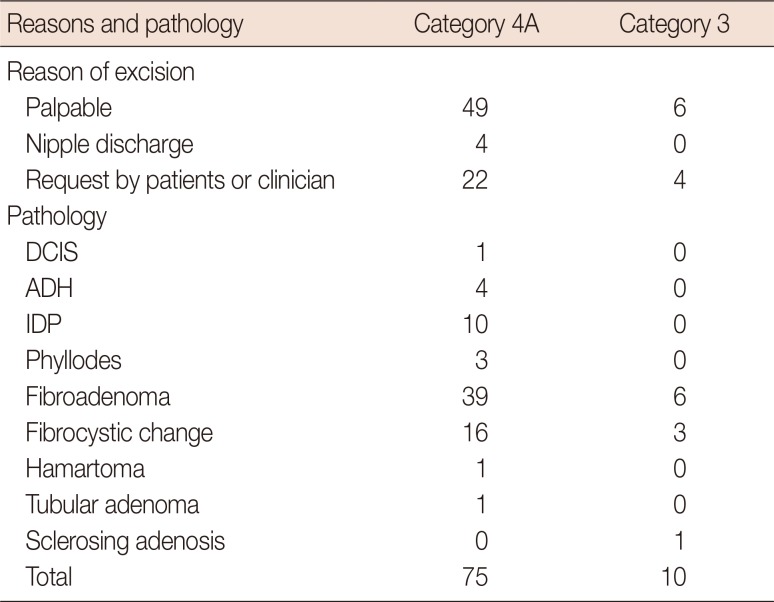
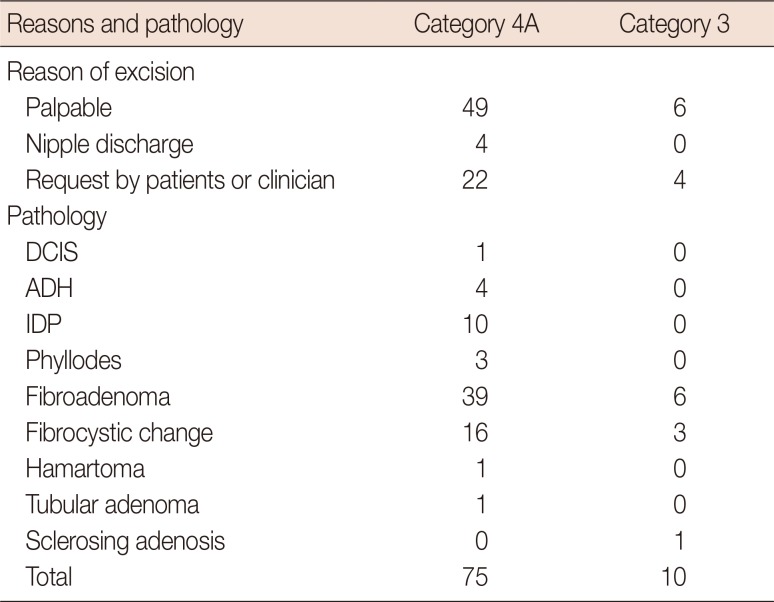
Immediate surgical excision was performed for the radiologic-pathologic concordant benign lesion based on some clinical symptoms such as a palpable lump or nipple discharge, or at the requests of clinicians or patients. The rate of immediate surgical excision was higher in the category 4A group than in the category 3 group, 75 cases (11.1%, 75/674) versus 10 cases (6.1%, 10/164). Only one cancer was confirmed in the category 4A group, a ductal carcinoma
in situ arising in a fibroadenoma, in a patient who had a palpable lump (
Table 1), with the initial biopsy diagnosis being florid ductal hyperplasia. The prevalence of malignancy in the excisional biopsy was 1.3% in the category 4A group and 0% in the category 3 group. Seventeen high-risk lesions (four atypical ductal hyperplasias, 10 intraductal papillomas, and three benign phyllodes tumors) were confirmed in the category 4A group (22.7%, 17/75) through immediate surgical excision. Initial core needle biopsy results of 17 high-risk lesions were as follows: three fibroadenomas, proved to be benign phyllodes tumors; one juvenile fibroadenoma; one usual ductal hyperplasia; two cases of sclerosing adenosis turned out to be atypical ductal hyperplasia; three cases of sclerosing adenosis; three cases of fibrocystic change; two cases of fibroadenoma; one microglandular adenosis; and one florid ductal hyperplasia turned out to contain intraductal papillomas. There was no case of malignancy or high-risk lesion in the category 3 group even in cases with clinical symptoms.
Table 1
Reason for immediate surgical excision and pathology
|
Reasons and pathology |
Category 4A |
Category 3 |
|
Reason of excision |
|
|
|
Palpable |
49 |
6 |
|
Nipple discharge |
4 |
0 |
|
Request by patients or clinician |
22 |
4 |
|
Pathology |
|
|
|
DCIS |
1 |
0 |
|
ADH |
4 |
0 |
|
IDP |
10 |
0 |
|
Phyllodes |
3 |
0 |
|
Fibroadenoma |
39 |
6 |
|
Fibrocystic change |
16 |
3 |
|
Hamartoma |
1 |
0 |
|
Tubular adenoma |
1 |
0 |
|
Sclerosing adenosis |
0 |
1 |
|
Total |
75 |
10 |

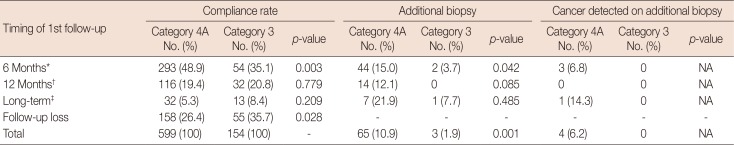
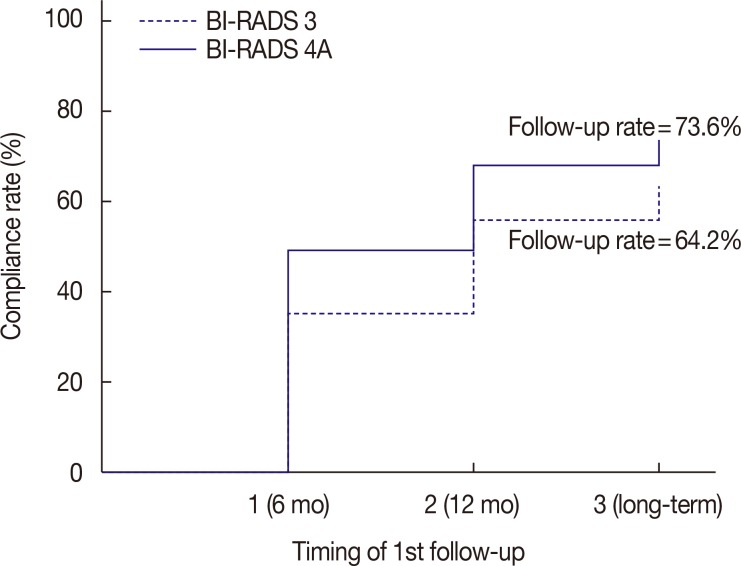
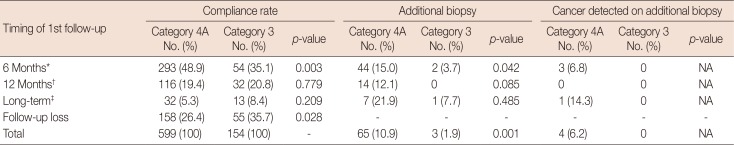
We investigated for any significant difference in the time of first imaging follow-up or compliance rate, depending on the initial BI-RADS category (
Table 2). There were 158 cases of follow-up loss in category 4A and 55 cases in category 3. The follow-up loss rate showed statistical significance in both the category 4A and 3 groups (26.4% vs. 35.7%,
p=0.028). Follow-up was possible in 441 patients in category 4A and 99 patients in category 3. The patients with initial category 4A showed higher compliance rate than those with category 3, with statistical significance (log-rank
p=0.015) (
Figure 2). In a 6-month follow-up, there was a statistical difference observed between the category 4A and 3 groups (48.9% vs. 35.1%,
p=0.003). In the 12-month and long-term follow-up groups, no significant differences were noted (19.4% vs. 20.8%,
p=0.779 in the 12-month follow-up; 5.3% vs. 8.4%,
p=0.209 in the long-term follow-up) (
Table 2). In the initial follow-up in the concordant benign group, the initial BIRADS category before core needle biopsy might affect the follow-up compliance especially on the 6-month follow-up.
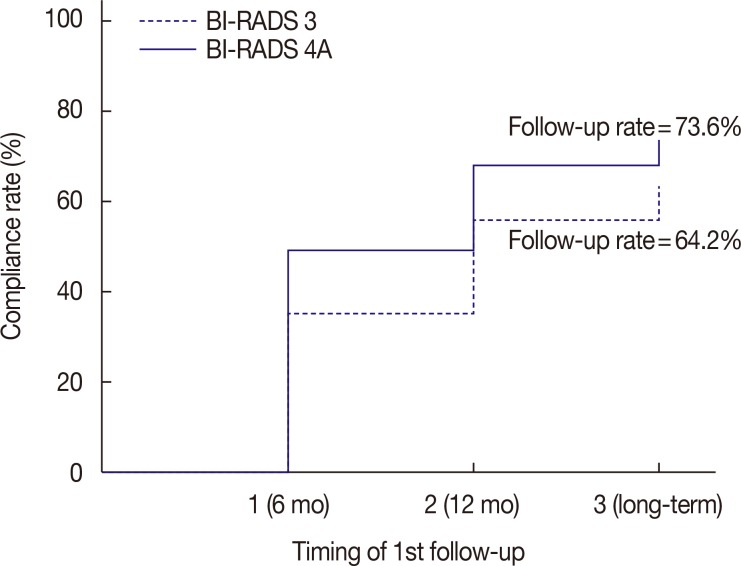 | Figure 2
Compliance rate in the timing of first follow-up. The patients with initial category 4A showed higher compliance rate than that of category 3 with statistical significance (log-rank p=0.015).
BI-RADS=Breast Imaging Reporting and Data System.

|
Table 2
Comparison of follow-up compliance and the first follow-up intervals according to the initial radiological category
|
Timing of 1st follow-up |
Compliance rate |
Additional biopsy |
|
Cancer detected on additional biopsy |
|
Category 4A No. (%) |
Category 3 No. (%) |
p-value |
Category 4A No. (%) |
Category 3 No. (%) |
p-value |
Category 4A No. (%) |
Category 3 No. (%) |
p-value |
|
6 Months*
|
293 (48.9) |
54 (35.1) |
0.003 |
44 (15.0) |
2 (3.7) |
0.042 |
3 (6.8) |
0 |
NA |
|
12 Months†
|
116 (19.4) |
32 (20.8) |
0.779 |
14 (12.1) |
0 |
0.085 |
0 |
0 |
NA |
|
Long-term‡
|
32 (5.3) |
13 (8.4) |
0.209 |
7 (21.9) |
1 (7.7) |
0.485 |
1 (14.3) |
0 |
NA |
|
Follow-up loss |
158 (26.4) |
55 (35.7) |
0.028 |
- |
- |
- |
- |
- |
- |
|
Total |
599 (100) |
154 (100) |
- |
65 (10.9) |
3 (1.9) |
0.001 |
4 (6.2) |
0 |
NA |

Except for the cases lost to follow-up, the remaining 441 category 4A cases and 99 category 3 cases were analyzed (
Table 2). The additional biopsy rate was higher in the initial category 4A group (10.9%) compared with the category 3 group (1.9%) with statistical significance (
p=0.001). Most of the additional biopsy was performed within 6 months in the initial category 4A group. We found four cases of malignancy and all of them were from initial category 4A and were carcinomas
in situ (one, intraductal papillary carcinoma and three, ductal carcinomas
in situ). Regardless of the follow-up timing, the malignancy detection was observed in the category 4A group only.
Go to :

DISCUSSION
About one million minimally invasive breast biopsies are performed in the United States each year, with about 75% yielding benign results [
6]. Delayed diagnosis of missed cancers has been reported in concordant benign results obtained after image-guided biopsy [
78]. Decisions for interval imaging in patients with core needle biopsies should be individualized based on imaging and pathologic findings. Although ACR BI-RADS's recommendation for category 3 lesions was an observation with regular period imaging, biopsies in category 3 lesions were performed in practices for several reasons, as follows: when the patients were transferred from private clinics, or when there was a discrepancy in interpretations between a clinician and a radiologist, or when the patient had clinical symptoms such as a palpable lump, pain, or nipple discharge associated with definite benign images, or when the breast lesions were found accidentally on other imaging modalities. There are several publications related to follow-up of concordant benign lesions [
34] or follow-up of category 3 lesions [
91011], but there were no reports about category 4A concordant benign follow-up or category 3 concordant benign follow-up. In this context, we hypothesized that because the initial category 4A or 3 was an important determinant for making a decision about percutaneous biopsy, it could affect even concordant benign results obtained after percutaneous biopsy from either category 4A or 3.
ACR BI-RADS recommends the likelihood of cancer in category 4A to be from 2% to 10% and that of category 3 to be less than 2% [
1]. We performed immediate surgical excisions if patients had clinical symptoms or if clinicians preferred excision to follow-up. The rate of immediate surgical excision in concordant benign cases was higher in the category 4A group than in the category 3 group and malignancy was confirmed only in patients with palpable lump in the category 4A group, which was confirmed as a ductal carcinoma
in situ arising with a fibroadenoma. Liberman et al. [
8] reported missed cancer like ours and our results could give power to the reliability of the BI-RADS recommendations by verifying that immediate surgical excision should be suggested if the patient in a higher category group had any clinical symptoms. Twenty-two initial category 4A lesions and four initial category 3 lesions were surgically excised before the next imaging follow-up, on the request of patients or clinicians, and no malignancy was found. If patients with concordant benign lesions did not have clinical symptoms, such as a palpable lump or nipple discharge, regular periodical imaging follow-up would be sufficient.
In our study, the compliance rate of initial category 4A was 73.6% and that of category 3 was 64.3%. We found a statistically higher follow-up rate of category 4A than category 3 on the 6-month follow-up, although this trend did not show any change in longer follow-ups, which means that the initial category before core needle biopsy affected the follow-up intervals. The clinicians might explain to the patients actively about the malignant risk of their breast lesions on following the ACR BI-RADS category or explain to the patients who already know the benign biopsy results so they did not find rebiopsy a necessity. The reported compliance rate of BI-RADS 3 ranged from 63% to 71% [
12].
Manjoros et al. [
13] reported that interval imaging performed within 12 months after detection of benign concordant breast biopsy demonstrated a low yield for the detection of breast cancer. Salkowski et al. [
7] suggested that yearly follow-up might be more appropriate because 6-month followup imaging for benign concordant lesions did not aid in detection of breast cancers or influence recommended rebiopsy rates. Youk et al. [
14] also recommended that in case of presence of concordant benign lesions after US-guided core needle biopsy, US follow-up should begin at minimum 12 months after core needle biopsy, considering that earlier the diagnosis, the better the prognosis. However, follow-up US should begin earlier, at 6 months after core needle biopsy, for concordant benign lesions associated with any clinical symptoms [
3]. Similar to that described in these reports, lesions with clinical symptoms were surgically excised in our study group before the next imaging follow-up and only one cancer was found in initial category 4A group.
Our result showed a higher additional biopsy rate in the initial category 4A group than in the initial category 3 group, with statistical significance. In addition, the cancer detection frequency on additional biopsy showed slightly higher trend in the initial category 4A group than in the category 3 group, especially on 6-month follow-ups. More attention should be paid to the initial category 4A group than the category 3 group during the 6-month follow-ups, as the chances for performing additional biopsy and finding a potential cancer are high at this time point.
Our study had several limitations. First, as a retrospective study, there was a lack of randomization. There was variability in actual follow-up times, likely influenced by multiple factors, including patient or referring physician preference, or insurance criteria. This could be a potential source of bias. Second, despite the large number of US-guided biopsies performed with available follow-up information, the actual number of patients that were included in our study was small. This might have excluded missed cancers that had been present in the population but were lost to follow-up, resulting in a lower than expected cancer yield with imaging interval. Third, the decision for additional biopsy was based on the change in imaging findings in the follow-up group and the clinical symptoms were not taken into consideration. Last, the pathologic slides of core or surgical specimens were not re-reviewed retrospectively by a pathologist and the original pathologic report was accepted.
Despite several limitations, initial category 4A or 3 of ACR BI-RADS could be a significant factor that affects follow-up compliance and even immediate surgical excision. It is related to a significantly high additional biopsy rate and clinically high cancer detection in the initial category 4A group. More attention should be paid to the concordant benign lesions from the initial category 4A group than from the category 3 group.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download