Abstract
Purpose
The aim of our study was to investigate the characteristics of primary and recurrent breast cancers and the correlation between cancer subtypes and detection modes.
Methods
Between 2003 and 2013, 147 cases of recurrent breast cancer in 137 women (mean age, 45.30±10.78 years) were identified via an annual clinical examination using radiological studies among 6,169 patients with a breast cancer history (mean follow-up period, 13.26±1.78 years). Clinical, radiological, and pathological findings including immunohistochemistry findings of primary and recurrent cancers were reviewed. The size of the tumor in primary and recurrent cancers, disease-free survival, methods of surgery, and the recurrence detection modalities were analyzed with respect to the breast cancer subtype.
Results
Ipsilateral and contralateral in-breast recurrence occurred in 105, 21 had axillary lymph node recurrence, and 21 had chest wall recurrences. The subtypes of the primary cancers were hormone receptor (HR) positive and human epidermal growth factor receptor 2 (HER2) negative (HR+HER2−) in 57, HER2 positive (HER2+) in 39, and triple-negative type in 51, and the recurrent cancers in each subtype showed the same type as the primary cancer in 84.3% of cases. In the in-breast recurrent cancers, the HR+HER2− cancers were most frequently detected using ultrasonography (15/43) followed by mammography (MG) (11/43). The HER2+ recurrent cancers were most commonly detected using MG (14/31, 45.2%), whereas triple-negative type recurrent cancers most commonly presented as symptomatic masses (15/31) (p=0.028).
Conclusion
Most recurrent breast cancers showed the same cancer subtype as the primary tumor, and recurrent breast cancer subtypes correlated with the detection modality. Imaging surveillance of survivors of breast cancer might be more beneficial in cases of HR+HER2− type breast cancer or HER2+ type breast cancer than in cases of triple-negative type breast cancer.
Breast cancer is the one of the most common cancers in women, and it remains the leading cause of death due to cancer among women [1234]. In Korea, the number of survivors of breast cancer who need long term surveillance has been increasing because of its high incidence (50.7 per 100,000 women per year), and the high 5-year relative survival rate (97.7%) of breast cancer [5]. Although significant advances have been made in systemic therapy, locoregional relapses are unfortunately common in breast cancer, and its prognosis has been correlated with conventional clinicopathological parameters including tumor size, grade, lymph node (LN) involvement, and cancer subtype [67].
The surveillance of patients with breast cancer after primary treatment varies among countries and institutions [8910]. Current recommendations for surveillance after primary breast cancer treatment involve routine follow-up, history-taking, clinical breast examination, and annual mammography (MG) [12]. Other imaging modalities, including magnetic resonance imaging (MRI) and ultrasonography (US) are not routinely recommended; however, there have been several studies evaluating the efficacy of various imaging modalities [111213].
In a systematic review of postoperative surveillance of patients with breast cancer, compared with MG, US demonstrated a higher sensitivity (94%–100%) for contralateral breast cancer and a higher sensitivity (43%–91%) with a comparable specificity (31%–95.1%) for ipsilateral breast cancer [10]. MRI also demonstrated comparable sensitivity (75%–100%) and specificity (66.6%–93%) with acceptable accuracy (95%) [10]. These studies suggest a potential role of supplemental imaging tests in survivors of breast cancer. However, investigations of cancer subtype and their correlations with the detection method in survivors of breast cancer are limited; there are no established surveillance recommendations for patients with a history of breast cancer based on the intrinsic subtype of the breast cancer.
Understanding the characteristics of initial and recurrent breast cancer in terms of molecular subtype and detection methods may improve the diagnostic efficacy of surveillance for local recurrences and provide information on decision-making regarding local control strategies for breast cancer.
In this study, we aimed to investigate the characteristics of initial and recurrent breast cancers and to analyze the correlation between cancer subtypes and detection modes.
Seoul National University Hospital Institutional Review Board approved our study (IRB approval number: 1608-011-781) and waived the need for informed consent because the study was performed retrospectively using routinely acquired images. Between 2003 and 2013, 6,169 patients (mean age, 48.4±10.2 years; range, 22–89 years) with breast cancer were treated via either mastectomy or breast conservation therapy at our institution.
A retrospective review of our image and clinical database identified 157 cases of breast cancer recurrence in the breasts, chest wall, or axilla. All cases were pathologically confirmed using either core needle biopsy (n=31) or surgery (n=126). Among 157 lesions, we excluded those without any available immunohistochemistry (IHC) results (one metaplastic carcinoma, one adenoid cystic carcinoma, four invasive mixed ductal and lobular carcinomas, one mucinous carcinoma, and three invasive ductal carcinomas). To analyze the surrogate intrinsic subtype of breast cancer, we reviewed the IHC result of each cancer and determined the expression of the estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). Finally, we included 147 cases of recurrent breast cancer in 137 women (mean age, 45.3±10.8 years; range, 22–78 years).
Our surveillance program after treatment of breast cancer consists of a clinical examination with a radiological examination including MG and US at intervals of 12 months. Screening breast MRI was also selectively performed annually for breast cancer patients according to the surgeon's request. MG examinations were obtained using dedicated digital MG units (Senographe 2000D units; GE Healthcare, Milwaukee, USA) or LORAD Selenia units (Hologic Inc., Boston, USA). Bilateral whole breast US including the axillary region was performed in the radial and anti-radial planes and/or transverse and sagittal planes. All US examinations were performed by one of five radiologists using high-resolution US equipment with a 14-6 MHz linear array transducer (HDI 5000 scanner, Advanced Technology Laboratories, Bothell, USA or LOGIQ 700 scanner, GE Medical Systems, Milwaukee, USA). In patients who had undergone a mastectomy, sonographic evaluations of the chest wall, contralateral breast, and both axilla were performed. Breast MRI examinations were performed with a 1.5 T system (Signa; GE Medical Systems). After obtaining a bilateral transverse localizer image, fat-suppressed T2-weighted fast spin-echo sagittal images were obtained (repetition time [TR]/echo time [TE], 5,500–7,150/85.2; image matrix, 256×160; field of view, 200×200 mm; and section thickness/gap, 1.5 mm/0 mm). A three-dimensional, T1-weighted fast spoiled gradient-echo sequence was also performed with bilateral sagittal imaging for one precontrast and five postcontrast dynamic series after 91, 180, 360, 449, and 598 seconds (TR/TE, 6.5/2.5; flip angle, 10°; image matrix, 256×160; field of view, 200×200 mm; and section thickness/gap, 1.5 mm/0 mm). The acquisition time of each postcontrast series was 76 seconds. In all patients, gadobutrol (Gadovist; Bayer Schering Pharma, Berlin, Germany) was injected into the antecubital vein using an automated injector (Spectris Solaris; Medrad Europe, Maastricht, Netherlands) at a dose of 0.1 mmol/kg and at a rate of 2 mL/sec, followed by a 20 mL saline flush.
After image acquisition, one of the five radiologists interpreted the MG, US, and/or MRI images, recorded the findings for each imaging modality, and gave an assessment according to the Breast Imaging-Reporting and Data System [14]. Each radiologist recorded whether the patients had any symptoms in their breast or axilla. In cases with multiple breast lesions, the lesion with the most suspicious finding was used for the final assessment. After the whole set of imaging interpretations was completed, the radiologist who interpreted the MRI findings combined those with the findings from other imaging modalities and arrived at a final diagnosis for each patient.
For the retrospective analysis of primary and recurrent cancers, pre- and post-operative MG, US, and MRI findings were retrospectively evaluated by two radiologists with 6 and 11 years of experience in breast imaging in consensus along with the clinical examination and pathologic findings. When the patient presented with a specific symptom such as palpability before imaging acquisition, and the lesion was found with a subsequent imaging modality, it was defined as symptom-detected. The cancers were categorized according to their recurrence detection imaging modality regardless of the time sequence in which the test was performed. If any lesion with abnormal findings on MG was also simultaneously detected with other modalities such as US or MRI, it was defined as MG-detected. The recurrent lesions that were detected on US but were not detected on MG were defined as US-detected regardless of MRI and positron emission tomography-computed tomography (PET-CT) positive findings. The lesions that had negative findings on MG and US, but were detected on MRI, were defined as MRI-detected even if the lesion was detected on PET-CT.
Histopathological evaluation was performed by a pathologist with 20 years of experience in breast pathology. Surgical specimens were sliced into 5-mm thick sections that were formalin-fixed, paraffin-embedded, and stained with hematoxylin and eosin for microscopic evaluation.
The expression of ER, PR, and HER2 were evaluated using a standard avidin-biotin complex immunohistochemical staining method. A cutoff value of 1% was used to define ER and PR positivity [15]. HER2 expression was initially assessed via immunohistochemical staining, and tumors with indeterminate HER2 IHC results were further evaluated with fluorescence in situ hybridization (HER2-chromosome 17 centromere ratio >2.0) [16]. Based on the IHC results, the tumors were classified into the following three surrogate subtypes according to their hormone receptors (HR) and HER2 expression statuses: HR+/HER2−, HER2+, and triple-negative (ER−/PR−/HER2−).
We reviewed data from medical records including age at diagnosis of the primary and recurrent breast cancer, anatomic recurrence site (ipsilateral and contralateral in-breast recurrence, axilla LN recurrence, and chest wall recurrence), TNM staging of the primary cancer, the operation method for the primary and recurrent cancer, the time interval between the primary cancer and recurrence, breast density at MG, and the pathology reports of the primary and recurrent cancer. The IHC-based subtypes of the primary and recurrent cancer were evaluated and their relationship with the recurrence detection method, recurrent site, and methods of operation were analyzed using chi-square tests.
A p-value less than 0.05 indicated statistical significance. All statistical analyses were performed with the use of SPSS version 21.0 software (IBM Corp., Armonk, USA).
Of 147 cases of recurrent breast cancer, 69 were ipsilateral and 36 were contralateral in-breast recurrences, 21 were chest wall recurrences, and 21 were axillary LN recurrences. The initial pathological examinations of these lesions showed 133 invasive ductal carcinomas and 14 ductal carcinoma in situ (DCIS). The average size of the primary invasive tumor was 2.48±1.69 cm (range, 0.1–11 cm). Breast conserving surgery was performed in 104 cases and mastectomy in 43 for treatment of the primary cancers. After recurrence, 37 cases involved breast-conserving surgery, 67 cases involved mastectomy, 13 cases involved axillary dissection, and 15 cases involved mass excision. After systematic work-up including PET-CT and chest CT, 11 cases were found to show associated remote metastasis and chemotherapy was started. Four patients refused to receive further treatment after recurrence. The histopathological assessment of the in-breast and chest wall recurrent masses showed invasive ductal carcinomas in 111 patients and DCIS in 15 patients.
Among 105 both in-breast recurrences, 35 cases presented as palpable masses, 31 cases were detected by MG, and 22 cases were detected by US. MRI detected 17 recurrences that could not be detected by MG and US.
Axilla LN recurrences were detected as a palpable mass in nine cases (9/21, 42.8%). US detected four ipsilateral LN recurrences and one contralateral LN recurrence. Two contralateral LN recurrences were detected on MG, and four ipsilateral LN recurrence and one contralateral LN recurrence were detected via PET-CT. None of the recurrent LNs were detected using MRI. Chest wall recurrence was detected with palpable symptoms in eight cases. US examination identified eight chest wall recurrent masses, and the remaining five chest wall recurrences were detected using PET-CT.
The primary and recurrent breast cancer subtypes detected were as follows: in 57 primary breast cancers with an HR+HER2− status, 50 lesions recurred as the same subtype (87.7%), and five (8.8%) and two (3.5%) recurred as HER2+ and triple-negative types, respectively. In 39 HER2+ cancers, 33 (84.6%) recurred as the same type, three cases recurred as HR+HER2− (7.7%), and three as triple-negative types (7.7%). In 51 triple-negative type cancers, 41 (80.4%) recurred as the same type, six (11.8%) as HR+HER2−, and four (7.8%) as HER2+.
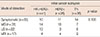
The recurrent breast cancer subtypes with in-breast recurrence showed a correlation with the mode of detection (p=0.028) (Table 1). The HR+HER2− cancers were most frequently detected with US (15/43, 34.9%), the HER2+ cancers were most frequently detected with MG (14/31, 45.2%), and the triple-negative type recurrent cancers most frequently presented as symptomatic masses (15/31, 48.4%). Even though the primary pathology and recurrent breast cancer subtypes shared the same tumor subtype in more than 80% of cases, the initial breast cancer subtypes were not significantly correlated with the in-breast recurrence detection mode (p=0.106) (Table 2). Among the initial HR+HER2− cancers, MG (n=14) or US (n=13) detected cancer recurrence more frequently than MRI (n=4). Initial HER2+ cancers were also more frequently found on MG (n=10). For the triple-negative types, the three imaging modalities showed no remarkable differences.
In this study, we found that most recurrent breast cancers showed the same cancer subtype as the primary cancers, and the recurrent breast cancer subtypes were correlated with the detection modality. Recurrent HR+HER2− cancers were most frequently detected using US, and recurrent HER2+ cancers were most frequently detected using MG. In addition, we observed that recurrent triple-negative subtype cancers most frequently presented with symptoms, which is consistent with the findings of another study [17]. The primary tumor subtype was not correlated with the detection modality of the recurrent cancer because the primary and recurrent cancer subtypes were not always the same. However, the correlation between the primary tumor subtypes and their detection method was similar to that of the recurrent cancers. Most of the primary HR+HER2− cancers were detected via MG and US (65.8%, 27/41), whereas triple-negative cancers were mainly diagnosed on the basis of symptoms (38.9%, 14/36), followed by diagnoses using MRI (25.0%, 9/36).
Imaging surveillance for postoperative patients remains controversial. The purpose of follow-up imaging is to detect early local recurrences or contralateral breast cancers and to monitor treatment responses. Although there are no randomized data to support any particular follow-up sequence or protocol that balances patient needs and costs, the European Society for Medical Oncology (ESMO) 2015 guideline recommends annual MG with US. MRI screening was recommended for young patients with dense breast tissue and genetic or familial predispositions [8]. The American Cancer Society/American Society of Clinical Oncology (ACS/ASCO) breast cancer survivorship care guidelines recommend annual MG for screening. The utility of US was not mentioned in the ASCO guideline, and MRI screening was not recommended unless the patient met the high-risk criteria [9]. Even though there is no evidence-based guideline for US screening in postoperative patients, several studies demonstrated the additional benefit of US for early-stage invasive cancer detection. US was helpful in the detection of mammographically occult breast cancers in the contralateral breast of women with a previous history of cancer and dense breasts [18]. Furthermore, US has a crucial role in the detection of recurrent lesions after breast cancer surgery, especially in patients who present with nonpalpable chest wall or axillary LN recurrences and mammographically occult parenchymal masses [19]. The American College of Radiology Imaging Network (ACRIN) 6666 study in which 53.1% of participants had a previous history of breast cancer also showed an incremental cancer yield of 4.2 cancers per 1,000 women in a single physician-performed prevalent US screen [20].
Even though the primary breast cancer subtypes were completely consistent with the recurrent cancers, further studies regarding surveillance programs should consider tumor subtypes. In a previous cohort study of 304 women with advanced breast cancer, primary luminal-like tumors frequently adopted a more aggressive subtype in their metastases. Comparing the primary tumor with an asynchronous metastasis, ER positivity was lost in 17%, PR positivity was lost in 39%, and HER2 positivity was lost in only 2% of patients. The subtype changes were observed not only in IHC markers, but also in intrinsic PAM50 subtypes [21]. In our study, only 23 out of the 147 recurrent cancers (15.6%) had a different IHC-based subtype than the primary cancer, and the HR+HER2− group showed changes to more aggressive subtypes in 12.3% of cases, which is lower than that of the previous report.
Different manifestations or characteristics of the imaging features of tumor subtypes have been demonstrated regardless of the consistency of tumor subtype. A noncircumscribed margin and posterior acoustic shadowing are associated with HR-positive tumors and lower-grade tumors, whereas posterior enhancement and a circumscribed margin are associated with HR-negative or high grade tumors [222324]. HER2-positive tumors show branching or fine linear calcifications on MG, irregularly shaped masses on US, and a washout or fast initial kinetics on MRI [25]. Triple-negative breast cancer tends to present as a mass with a relatively circumscribed margin without calcifications. The absence of associated calcifications and a lower association with DCIS suggests rapid progression of malignant transformation bypassing the in situ stage [26]. Owing to the differing imaging features according to tumor subtype, the detection method could vary according to tumor subtype. Bae et al. [27] reported that US-detected breast cancers are more likely to be small invasive cancers and more likely to be of the luminal A subtype. Thus, we can infer that the selection of the screening method could be based on the tumor subtype.
There are several limitations of our study. First, this study is a retrospective single center study with a relatively small number of patients. Our results failed to show a statistically significant correlation between detection methods and primary cancer subtype. We assume that a large-scale study could overcome this limitation. Second, we selected only patients with available IHC data, which may have resulted in selection bias. A prospective study of postoperative patients with imaging and clinical follow-up data could provide more information on the incidence, characteristics, and the tumor subtype of recurrent cancers. Third, because this study has a retrospective nature, there is a possibility that the inter-modality interpretation in the image analysis may have influenced each other.
Furthermore, we did not analyze the cost effectiveness of the surveillance program. The cost of US and MRI surveillance is higher than that of MG. The duration of the examination and the time taken for the radiologist's interpretation are also longer using those modalities. Therefore, cost effectiveness should be evaluated in further studies.
In conclusion, most recurrent breast cancers were of the same cancer subtype as the primary tumors, and the recurrent breast cancer subtypes were correlated with the detection modality. Imaging surveillance of breast cancer after treatment might be more beneficial in cases of primary HR+HER2− or HER2+ type breast cancer than in cases of triple-negative type breast cancers.
Figures and Tables
Table 1
The mode of detection and the recurred surrogate subtypes with in-breast recurrence
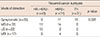
| Mode of detection | Initial cancer subtypes | |||
|---|---|---|---|---|
| HR+HER2− (n = 43) | HER2+ (n = 31) | TN (n = 31) | p-value | |
| Symptomatic (n = 35) | 9 | 11 | 15 | 0.028 |
| MG (n = 31) | 11 | 14 | 6 | |
| US (n = 22) | 15 | 2 | 5 | |
| MRI (n = 17) | 8 | 4 | 5 | |
Notes
References
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108.

2. Garne JP, Aspegren K, Balldin G, Ranstam J. Increasing incidence of and declining mortality from breast carcinoma: trends in Malmö, Sweden, 1961-1992. Cancer. 1997; 79:69–74.

3. Otten JD, Broeders MJ, Fracheboud J, Otto SJ, de Koning HJ, Verbeek AL. Impressive time-related influence of the Dutch screening programme on breast cancer incidence and mortality, 1975-2006. Int J Cancer. 2008; 123:1929–1934.

4. Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: an independent review. Lancet. 2012; 380:1778–1786.
5. National Cancer Center. Ministry of Health and Welfare. Korea Central Cancer Registry. Annual Report of Cancer Statistics in Korea in 2012. Goyang: National Cancer Center;2014.
6. Soerjomataram I, Louwman MW, Ribot JG, Roukema JA, Coebergh JW. An overview of prognostic factors for long-term survivors of breast cancer. Breast Cancer Res Treat. 2008; 107:309–330.

7. Lowery AJ, Kell MR, Glynn RW, Kerin MJ, Sweeney KJ. Locoregional recurrence after breast cancer surgery: a systematic review by receptor phenotype. Breast Cancer Res Treat. 2012; 133:831–841.

8. Senkus E, Kyriakides S, Penault-Llorca F, Poortmans P, Thompson A, Zackrisson S, et al. Primary breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013; 24:Suppl 6. vi7–vi23.

9. Runowicz CD, Leach CR, Henry NL, Henry KS, Mackey HT, Cowens-Alvarado RL, et al. American Cancer Society/American Society of Clinical Oncology breast cancer survivorship care guideline. J Clin Oncol. 2016; 34:611–635.

10. Yoon JH, Kim MJ, Kim EK, Moon HJ. Imaging surveillance of patients with breast cancer after primary treatment: current recommendations. Korean J Radiol. 2015; 16:219–228.

11. Berg WA, Zhang Z, Lehrer D, Jong RA, Pisano ED, Barr RG, et al. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012; 307:1394–1404.

12. Kim MJ, Kim EK, Kwak JY, Park BW, Kim SI, Sohn J, et al. Role of sonography in the detection of contralateral metachronous breast cancer in an Asian population. AJR Am J Roentgenol. 2008; 190:476–480.

13. Kim MJ, Kim EK, Kwak JY, Park BW, Kim SI, Sohn J, et al. Sonographic surveillance for the detection of contralateral metachronous breast cancer in an Asian population. AJR Am J Roentgenol. 2009; 192:221–228.

14. American College of Radiology, BI-RADS Committee. ACR BI-RADS Atlas: Breast Imaging Reporting and Data System. 5th ed. Reston: American College of Radiology;2013.
15. Spitale A, Mazzola P, Soldini D, Mazzucchelli L, Bordoni A. Breast cancer classification according to immunohistochemical markers: clinicopathologic features and short-term survival analysis in a population-based study from the South of Switzerland. Ann Oncol. 2009; 20:628–635.

16. Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013; 31:3997–4013.

17. Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007; 13(15 Pt 1):4429–4434.

18. Kim SJ, Chung SY, Chang JM, Cho N, Han W, Moon WK. Ultrasound screening of contralateral breast after surgery for breast cancer. Eur J Radiol. 2015; 84:54–60.

19. Kim SJ, Moon WK, Cho N, Chang JM. The detection of recurrent breast cancer in patients with a history of breast cancer surgery: comparison of clinical breast examination, mammography and ultrasonography. Acta Radiol. 2011; 52:15–20.

20. Berg WA, Blume JD, Cormack JB, Mendelson EB, Lehrer D, Böhm-Vélez M, et al. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA. 2008; 299:2151–2163.

21. Kimbung S, Kovács A, Danielsson A, Bendahl PO, Lövgren K, Frostvik Stolt M, et al. Contrasting breast cancer molecular subtypes across serial tumor progression stages: biological and prognostic implications. Oncotarget. 2015; 6:33306–33318.

22. Shin HJ, Kim HH, Huh MO, Kim MJ, Yi A, Kim H, et al. Correlation between mammographic and sonographic findings and prognostic factors in patients with node-negative invasive breast cancer. Br J Radiol. 2011; 84:19–30.

23. Mazurowski MA, Zhang J, Grimm LJ, Yoon SC, Silber JI. Radiogenomic analysis of breast cancer: luminal B molecular subtype is associated with enhancement dynamics at MR imaging. Radiology. 2014; 273:365–372.

24. Kawashima H, Inokuchi M, Furukawa H, Kitamura S. Triple-negative breast cancer: are the imaging findings different between responders and nonresponders to neoadjuvant chemotherapy? Acad Radiol. 2011; 18:963–969.
25. Elias SG, Adams A, Wisner DJ, Esserman LJ, van't Veer LJ, Mali WP, et al. Imaging features of HER2 overexpression in breast cancer: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2014; 23:1464–1483.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download