1. Burstein HJ, Lacchetti C, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology Clinical Practice guideline update on ovarian suppression. J Clin Oncol. 2016; 34:1689–1701. PMID:
26884586.

2. Singh G. Oophorectomy in breast cancer-controversies and current status. Indian J Surg. 2012; 74:210–212. PMID:
23730045.

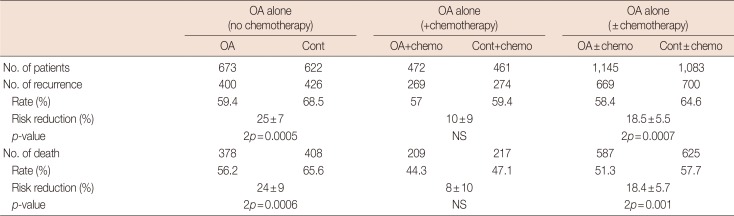
3. Early Breast Cancer Trialists' Collaborative Group. Ovarian ablation in early breast cancer: overview of the randomised trials. Lancet. 1996; 348:1189–1196. PMID:
8898035.
4. Francis PA, Regan MM, Fleming GF, Láng I, Ciruelos E, Bellet M, et al. Adjuvant ovarian suppression in premenopausal breast cancer. N Engl J Med. 2015; 372:436–446. PMID:
25495490.

5. Pagani O, Regan MM, Walley BA, Fleming GF, Colleoni M, Láng I, et al. Adjuvant exemestane with ovarian suppression in premenopausal breast cancer. N Engl J Med. 2014; 371:107–118. PMID:
24881463.

6. Moore HC, Unger JM, Phillips KA, Boyle F, Hitre E, Porter D, et al. Goserelin for ovarian protection during breast-cancer adjuvant chemotherapy. N Engl J Med. 2015; 372:923–932. PMID:
25738668.

7. Beatson GT. On the treatment of inoperable cases of carcinoma of the mamma: suggestions for a new method of treatment, with illustrative cases. Lancet. 1896; 148:104–107.

8. Beatson GT. On the treatment of inoperable cases of carcinoma of the mamma: suggestions for a new method of treatment, with illustrative cases. Lancet. 1896; 148:162–165.

9. Love RR, Philips J. Oophorectomy for breast cancer: history revisited. J Natl Cancer Inst. 2002; 94:1433–1434. PMID:
12359852.

10. Boyd S. On oöphorectomy in the treatment of cancer. Br Med J. 1897; 2:890–896.
11. Boyd S. On oophorectomy in cancer of the breast. BMJ. 1900; 2:1161–1167.
12. Huggins C, Dao TL. Adrenalectomy and oophorectomy in treatment of advanced carcinoma of the breast. J Am Med Assoc. 1953; 151:1388–1394. PMID:
13034482.
13. Mueller MD, Dreher E, Eggimann T, Linder H, Altermatt H, Hänggi W. Is laparoscopic oophorectomy rational in patients with breast cancer? Surg Endosc. 1998; 12:1390–1392. PMID:
9822463.

14. Ahlbom H. Castration by roentgen rays as an auxiliary treatment in the radiotherapy of cancer Mammae at Radiumhemmet, Stockholm. Acta Radiol. 1930; 11:614–635.

15. Lees AW, Giuffre C, Burns PE, Hurlburt ME, Jenkins HJ. Oophorectomy versus radiation ablation of ovarian function in patients with metastatic carcinoma of the breast. Surg Gynecol Obstet. 1980; 151:721–724. PMID:
7444722.

16. Dees EC, Davidson NE. Ovarian ablation as adjuvant therapy for breast cancer. Semin Oncol. 2001; 28:322–331. PMID:
11498826.

17. Bese NS, Iribas A, Dirican A, Oksuz D, Atkovar G, Ober A. Ovarian ablation by radiation therapy: is it still an option for the ablation of ovarian function in endocrine responsive premenopausal breast cancer patients? Breast. 2009; 18:304–308. PMID:
19800233.

18. Davidson NE. Ovarian ablation as treatment for young women with breast cancer. J Natl Cancer Inst Monogr. 1994; (16):95–99. PMID:
7528032.
19. Allen E, Doisy EA. An ovarian hormone: preliminary report on its localization, extraction and partial purification, and action in test animals. JAMA. 1923; 81:819–821.
20. Toft D, Gorski J. A receptor molecule for estrogens: isolation from the rat uterus and preliminary characterization. Proc Natl Acad Sci U S A. 1966; 55:1574–1581. PMID:
5227676.

21. Schally AV, Arimura A, Kastin AJ, Matsuo H, Baba Y, Redding TW, et al. Gonadotropin-releasing hormone: one polypeptide regulates secretion of luteinizing and follicle-stimulating hormones. Science. 1971; 173:1036–1038. PMID:
4938639.

22. Engel JB, Schally AV. Drug insight: clinical use of agonists and antagonists of luteinizing-hormone-releasing hormone. Nat Clin Pract Endocrinol Metab. 2007; 3:157–167. PMID:
17237842.

23. Schally AV, Comaru-Schally AM, Nagy A, Kovacs M, Szepeshazi K, Plonowski A, et al. Hypothalamic hormones and cancer. Front Neuroendocrinol. 2001; 22:248–291. PMID:
11587553.

24. Taylor CW, Green S, Dalton WS, Martino S, Rector D, Ingle JN, et al. Multicenter randomized clinical trial of goserelin versus surgical ovariectomy in premenopausal patients with receptor-positive metastatic breast cancer: an intergroup study. J Clin Oncol. 1998; 16:994–999. PMID:
9508182.

25. Boccardo F, Rubagotti A, Perrotta A, Amoroso D, Balestrero M, De Matteis A, et al. Ovarian ablation versus goserelin with or without tamoxifen in pre-perimenopausal patients with advanced breast cancer: results of a multicentric Italian study. Ann Oncol. 1994; 5:337–342. PMID:
8075030.

26. Prowell TM, Davidson NE. What is the role of ovarian ablation in the management of primary and metastatic breast cancer today? Oncologist. 2004; 9:507–517. PMID:
15477635.

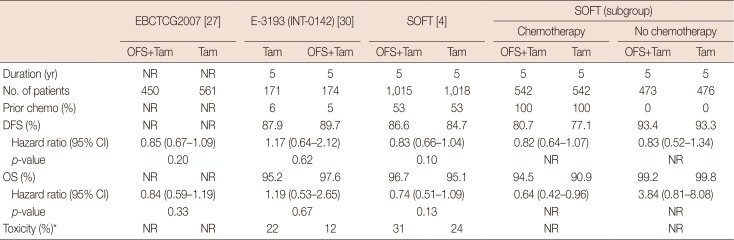
27. LHRH-agonists in Early Breast Cancer Overview Group. Cuzick J, Ambroisine L, Davidson N, Jakesz R, Kaufmann M, et al. Use of luteinising-hormone-releasing hormone agonists as adjuvant treatment in premenopausal patients with hormone-receptor-positive breast cancer: a meta-analysis of individual patient data from randomised adjuvant trials. Lancet. 2007; 369:1711–1723. PMID:
17512856.
28. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005; 365:1687–1717. PMID:
15894097.
29. Söreide JA, Varhaug JE, Fjösne HE, Erikstein B, Jacobsen AB, Skovlund E, et al. Adjuvant endocrine treatment (goserelin vs tamoxifen) in premenopausal patients with operable node positive stage II breast cancer: a prospective randomized national multicenter study. Eur J Surg Oncol. 2002; 28:505–510. PMID:
12217302.

30. Tevaarwerk AJ, Wang M, Zhao F, Fetting JH, Cella D, Wagner LI, et al. Phase III comparison of tamoxifen versus tamoxifen plus ovarian function suppression in premenopausal women with node-negative, hormone receptor-positive breast cancer (E-3193, INT-0142): a trial of the Eastern Cooperative Oncology Group. J Clin Oncol. 2014; 32:3948–3958. PMID:
25349302.

31. Ribi K, Luo W, Bernhard J, Francis PA, Burstein HJ, Ciruelos E, et al. Adjuvant tamoxifen plus ovarian function suppression versus tamoxifen alone in premenopausal women with early breast cancer: patient-reported outcomes in the Suppression of Ovarian Function Trial. J Clin Oncol. 2016; 34:1601–1610. PMID:
27022111.

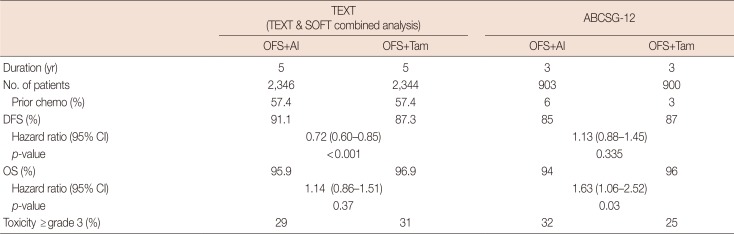
32. Regan MM, Francis PA, Pagani O, Fleming GF, Walley BA, Viale G, et al. Absolute benefit of adjuvant endocrine therapies for premenopausal women with hormone receptor-positive, human epidermal growth factor receptor 2-negative early breast cancer: TEXT and SOFT trials. J Clin Oncol. 2016; 34:2221–2231. PMID:
27044936.

33. Gnant M, Mlineritsch B, Stoeger H, Luschin-Ebengreuth G, Knauer M, Moik M, et al. Zoledronic acid combined with adjuvant endocrine therapy of tamoxifen versus anastrozol plus ovarian function suppression in premenopausal early breast cancer: final analysis of the Austrian Breast and Colorectal Cancer Study Group Trial 12. Ann Oncol. 2015; 26:313–320. PMID:
25403582.

34. Lambertini M, Ceppi M, Poggio F, Peccatori FA, Azim HA Jr, Ugolini D, et al. Ovarian suppression using luteinizing hormone-releasing hormone agonists during chemotherapy to preserve ovarian function and fertility of breast cancer patients: a meta-analysis of randomized studies. Ann Oncol. 2015; 26:2408–2419. PMID:
26347105.

35. Elgindy E, Sibai H, Abdelghani A, Mostafa M. Protecting ovaries during chemotherapy through gonad suppression: a systematic review and meta-analysis. Obstet Gynecol. 2015; 126:187–195. PMID:
26241272.
36. Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013; 31:2500–2510. PMID:
23715580.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download