Abstract
Fibroadenoma is a common benign breast lesion and its malignant transformation is rare. There have been several case reports and studies that retrospectively reviewed breast cancers that arose within fibroadenomas; however, none of these studies reported serial changes in radiologic features of the cancer, including findings from mammography and ultrasound (US). We report a case of breast cancer arising adjacent to an involuting fibro adenoma in a 39-year-old woman who was undergoing serial follow-up after her fibroadenoma was diagnosed. Seven years after her diagnosis, the lesion showed evidence of coarse calcifications, a typical sign of involution. Four years later, US revealed a newly developed hypoechoic lesion with irregular margins and peripherally located calcifications adjacent to the fibroadenoma. A core biopsy was performed, and histopathological examination resulted in a diagnosis of invasive ductal carcinoma. When new suspicious features are observed in a fibroadenoma, radiologists should raise the concern for breast cancer and proceed with diagnosis and treatment accordingly.
Fibroadenoma is a common benign breast lesion occurring in 25% of asymptomatic women [1]. Although previous studies of patients with fibroadenoma report an increased risk of breast carcinoma compared to similarly aged women in the general population, malignant transformation from fibroadenoma to cancer is rare [2]. Furthermore, Worsham et al. [3] reported that the presence of fibroadenoma, regardless of whether the lesion was proliferative or nonproliferative, was protective against breast cancer progression, a result that conflicted with the findings of previous studies. Therefore, management of fibroadenomas has typically been conservative [4]. Lesions that show typical features of fibroadenomas are classified as Breast Imaging Reporting and Data System (BI-RADS) category 3; if the lesion is considered to be involuting, it is classified as BI-RADS category 2.
In this article, we report a case of breast cancer that arose adjacent to or from an involuting fibroadenoma. There have been several case reports and studies that retrospectively reviewed breast cancers that arose within fibroadenomas; however, none of these studies reported serial changes in radiologic features of the cancer site, including findings from mammography and ultrasound (US). In this article, we report a case of breast cancer that arose adjacent to or within a fibroadenoma. Data from the case reported here include mammographic, sonographic, and magnetic resonance (MR) images that were also correlated with pathologic features.
A 39-year-old woman with dense breast tissue underwent breast US as part of her regular screening exam at a local hospital. The US revealed a 0.7 cm nodule located in the upper-outer quadrant (UOQ) of her left breast, classified as BI-RADS category 3 (Figure 1). A follow-up US was recommended.
Two years later, the patient revisited our hospital complaining of a palpable mass in the UOQ of the left breast. US revealed a 1.8 cm circumscribed isoechoic mass in the UOQ of her left breast. It appeared that the previously noted nodule had increased in size (157% over 2 years), and the nodule was then classified as BI-RADS category 4A (Figure 2). This reclassification indicated a need for US-guided core biopsy, which confirmed that the nodule was a fibroadenoma. Subsequent surgery was recommended, but the patient refused and elected to undergo regular follow-up instead.
The patient returned to our hospital after 5 years, because she had been told during a routine follow-up exam performed at an outside hospital that calcifications had newly developed in the lesion. Her mammogram showed macrocalcifications that were centrally located within the lesion and that had a "popcorn-like" appearance (Figure 3A). US revealed that the nodule had decreased in size while also developing internal calcifications, findings indicative of an involuting fibroadenoma (Figure 3B). Because she was scheduled to undergo hormone replacement therapy for menopausal symptoms, the patient was concerned about the presence of calcifications. She wished to have a repeat biopsy of the lesion prior to initiating hormone replacement therapy. The rebiopsy confirmed the diagnosis of fibroadenoma, and the patient began hormonal therapy, which she continued for 3 years.
Another 4 years later, 11 years after the initial fibroadenoma diagnosis, the patient revisited our imaging center because the nodule had increased in size, according to an US result she had received from her local hospital. The patient underwent mammography at our hospital; this showed that the fibroadenoma was denser but the size of the lesion was similar compared to that of her previous exam (Figure 4A). We also performed US of the lesion, which revealed that the fibroadenoma had enlarged eccentrically and was accompanied by a 0.8×1.3 cm, microlobulated hypoechoic lesion. No changes in the previously detected calcifications in the UOQ were noted (Figure 4B). The lesion was classified as BI-RADS category 4A, and a core biopsy was indicated. The biopsy targeted the eccentrically enlarged portion, which was delineated on the US exam. Biopsy confirmed that the lesion was an invasive ductal carcinoma (IDC). For preoperative evaluation, MR imaging was performed and revealed a 1.5 cm enhancing mass in the UOQ of the patient's left breast, which correlated with the lesion detected on US (Figure 5).
The patient underwent breast conservation surgery, which identified a 1.4 cm IDC (estrogen receptor 90% positive, progesterone receptor 60% positive, human epidermal growth factor receptor 2 negative) abutting the previously confirmed fibroadenoma (Figure 6) without axillary metastasis. She underwent postoperative definitive radiation therapy targeted to the left breast.
Fibroadenomas are common benign lesions of the breast that usually present as a single breast mass in young women [4]. There is some controversy regarding whether patients with fibroadenomas have an increased risk of subsequent breast cancer relative to other women. However, because malignant transformation from fibroadenoma is rarely reported, the management of fibroadenomas is typically conservative [4]. Complex fibroadenomas are a subtype of fibroadenoma that harbors one or more complex features, including epithelial calcifications, papillary apocrine metaplasias, sclerosing adenosis, or cysts larger than 3 mm [1]. The risk of developing breast cancer was found to be higher in patients with complex fibroadenomas than in those with noncomplex fibroadenomas (3.1 times greater among women with complex fibroadenomas versus 1.89 times greater among women with noncomplex fibroadenomas, compared to control groups) [5].
There have been some case reports of breast cancer arising within a fibroadenoma; however, these reports lack imaging findings in which the cancer is distinguishable from the fibroadenoma. Abe et al. [6] reported a case of scirrhous-type IDC arising in a fibroadenoma. On US, the suspicious palpable lesion appeared to have ill-defined heterogeneously hypoechoic features; however, the fibroadenoma and cancer components could not be distinguished. Monsefi et al. [7] reported a case of mucinous subtype IDC arising within a fibroadenoma with mammography images only. The lesion appeared to have a well-circumscribed border without calcifications, suggesting a benign lesion, most likely fibroadenoma. However, surgery revealed it to be a mucinous subtype of IDC [7]. Thus, it was difficult to find clues of cancers arising within or adjacent to fibroadenomas on imaging findings. More recently, Iwamoto et al. [8] reported a case of breast IDC that was adjacent to one of multiple macrocalcified fibroadenomas in a patient who had undergone mastectomy for the primary IDC more than 13 years earlier. The sonographic findings in Iwamoto et al.'s case report were similar to ours, particularly with regard to the hypoechoic mass with a microlobulated margin and microcalcifications adjacent to the macrocalcifications of the fibroadenoma. However, at the time of IDC diagnosis, the patient in Iwamoto et al.'s case already had axillary lymph node metastasis and had progressed far more than was the case with our patient.
Our case evaluation has some strengths that are distinguished from other published reports. First, we reported serial imaging findings of the fibroadenoma over time, which allowed us to demonstrate changes in the size of the lesion. During the follow-up, we could detect the newly developed malignant lesion adjacent to the fibroadenoma on the US images, based on regular screening mammography and US in a patient with heterogeneously dense breasts. We also correlated these findings with those of MR imaging performed during the preoperative evaluation. High-resolution ultrasonographic images enabled us to perform a targeted percutaneous biopsy of the suspicious lesion so that we were able to make the diagnosis of IDC before surgery, which is noteworthy because it meant we were able to diagnose IDC at an early stage (T1N0), without axillary lymph node metastasis.
Abe et al. [6] reviewed 15 cases of previously reported breast carcinomas occurring within fibroadenomas, among which carcinoma in situ was the dominant type (56.3%). They attributed this to the ability to make an earlier diagnosis of malignant neoplasm coexisting with an easily palpable fibroadenoma. However, in only two cases were these carcinomas <2 cm in size. In fact, the presence of fibroadenoma may obscure a small-sized cancer that is within or adjacent to the fibroadenoma if a meticulous evaluation is not undertaken. Therefore, it is encouraging that we were able to make a cancer diagnosis at an early stage based on regular screening mammography and US. However, we do not suggest that all involuting fibroadenomas require this type of follow-up. As many other previous case reports have suggested, even if the fibroadenoma is a benign neoplasm that is unlikely to undergo malignant transformation, radiologists should pay attention when imaging reveals newly developed suspicious features, such as irregular or microlobulated margins, increased size, or eccentric calcifications. Any changes that are newly detected should increase the concern for cancer.
In conclusion, we discuss the serial radiologic and pathologic findings of a case of breast cancer that arose adjacent to an involuting fibroadenoma. Fibroadenomas themselves and the malignancies arising within them can exhibit variable features on imaging studies. When new suspicious features are observed in a fibroadenoma, radiologists should raise the concern for breast cancer and proceed with diagnosis and treatment accordingly.
Figures and Tables
 | Figure 1Initial ultrasound image of left breast. Ultrasound image of a 0.7 cm, isoechoic, probably benign nodule in the upper-outer portion (1 o'clock) of the left breast. |
 | Figure 2Ultrasound image of left breast taken 2 years after original diagnosis. An ultrasound image taken 2 years after the original diagnosis, showing an 1.8 cm, circumscribed isoechoic mass lesion in the upper-outer portion (1 o'clock) of the left breast, which had increased in size compared to the previously noted nodule. |
 | Figure 3Radiologic images taken 5 years after the time when Figure 2 was taken. (A) Mammography. Mediolateral-oblique view (left) and cranialcaudal view (right). The nodule shows newly developed calcifications. Macrocalcification was noted centrally within the lesion and had a "popcorn-like" appearance. (B) Ultrasound. The image shows a 1.1 cm, newly developed, centrally located calcification that appears to be an isoechoic mass lesion in the upper-outer portion (1 o'clock) of the left breast, suggesting involuting fibroadenoma. Core biopsy confirmed this lesion as fibroadenoma. |
 | Figure 4Radiologic images taken 4 years after the time when Figure 3 were taken. (A) Mammography. Mediolateral-oblique view (left) and cranial-caudal view (right). It shows that the previously confirmed fibroadenoma was denser but had not changed significantly in size over time. (B) Ultrasound. Transverse view (left) and longitudinal view (right). It shows that the previously noted, centrally located calcification was now shifted into the periphery, with the nodule increasing in size with microlobulated margin (arrow) at the upper-outer portion (1 o'clock) of the left A breast. |
 | Figure 5Magnetic resonance imaging at an early phase after contrast injection with subtraction. Magnetic resonance imaging at an early phase after contrast injection with subtraction revealed an approximately 1.5 cm mass with arterial enhancing components (arrows) that correlated well with microlobulated hypoechoic lesions on ultrasound; this lesion was confirmed for invasive ductal carcinoma. The unenhancing portion (arrowhead) is considered fibroadenoma. |
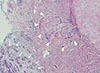 | Figure 6Histological examination revealed invasive ductal carcinoma arising adjacent to the fibroadenoma (H&E stain, ×40). Histological examination revealed invasive ductal carcinoma (arrows) arising adjacent to the fibroadenoma (arrowheads) that is well distinguished from the fibroadenoma due to its distinct margin. The distance between invasive ductal carcinoma and fibroadenoma is measured as 500 µm. |
References
1. Kuijper A, Mommers EC, van der Wall E, van Diest PJ. Histopathology of fibroadenoma of the breast. Am J Clin Pathol. 2001; 115:736–742.

2. Carter BA, Page DL, Schuyler P, Parl FF, Simpson JF, Jensen RA, et al. No elevation in long-term breast carcinoma risk for women with fibroadenomas that contain atypical hyperplasia. Cancer. 2001; 92:30–36.

3. Worsham MJ, Raju U, Lu M, Kapke A, Botttrell A, Cheng J, et al. Risk factors for breast cancer from benign breast disease in a diverse population. Breast Cancer Res Treat. 2009; 118:1–7.

4. Sklair-Levy M, Sella T, Alweiss T, Craciun I, Libson E, Mally B. Incidence and management of complex fibroadenomas. AJR Am J Roentgenol. 2008; 190:214–218.

5. Dupont WD, Page DL, Parl FF, Vnencak-Jones CL, Plummer WD Jr, Rados MS, et al. Long-term risk of breast cancer in women with fibroadenoma. N Engl J Med. 1994; 331:10–15.

6. Abe H, Hanasawa K, Naitoh H, Endo Y, Tani T, Kushima R. Invasive ductal carcinoma within a fibroadenoma of the breast. Int J Clin Oncol. 2004; 9:334–338.

7. Monsefi N, Nikpour H, Safavi M, Lashkarizadeh MR, Dabiri S. Mucinous subtype of invasive ductal carcinoma arising within a fibroadenoma. Arch Iran Med. 2013; 16:366–368.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download