Abstract
Purpose
The purpose of this study was to assess the incidence of invasive lobular carcinoma (ILC) and to compare the clinicopathological features and treatment results after breast conserving surgery (BCS) followed by radiotherapy between ILC and invasive ductal carcinoma (IDC).
Methods
A total of 1,071 patients who underwent BCS followed by radiotherapy were included in the study. Medical records and pathological reports were retrospectively reviewed.
Results
The incidence of ILC was 5.2% (n=56). Bilateral breast cancer, lower nuclear grade, and hormone receptor-positive breast cancer were more frequent in patients with ILC than in those with IDC. There were no cases of lymphovascular invasion or the basal-like subtype in patients with ILC. There were no statistically significant differences in patterns of failure or treatment outcomes between patients with ILC and those with IDC. The development of metachronous contralateral breast cancer was more frequent in patients with IDC (n=27). Only one patient with ILC developed contralateral breast cancer, with a case of ductal carcinoma in situ.
Conclusion
The incidence of ILC was slightly higher in our study than in previous Korean studies, but was lower than the incidences reported in Western studies. The differences we observed in clinico pathological features between ILC and IDC were similar to those described elsewhere in the literature. Although there were no statistically significant differences, there was a trend toward better disease-specific survival and disease-free survival rates in patients with ILC than in those with IDC.
The breast is composed of adipose tissue and glandular tissue. A terminal ductal-lobular unit is the basic unit of the glandular tissue and is postulated as the site of origin of most breast cancers [1]. Invasive lobular carcinoma (ILC) arises in the lobule and is microscopically characterized by linear infiltration of small uniform cells. It is the second most common invasive breast cancer after invasive ductal carcinoma (IDC), accounting for 2% to 3% of breast cancers in Korean women [23456]. Multicentric, bilateral, and estrogen receptor (ER)-positive cancers are frequent in patients with ILC compared to those with IDC [789]. Although some studies have claimed that the local recurrence rate after partial mastectomy in patients with ILC is high [1011], the treatment outcomes of breast conserving surgery (BCS) followed by radiation ther apy are comparable to those of mastectomy [12].
The purpose of the current study was to assess the incidence of ILC among patients who underwent BCS followed by radio therapy and to compare the clinicopathological features and treatment results between ILC and IDC.
This was a retrospective study of 1,071 patients with invasive ductal or lobular carcinomas of the breast who underwent BCS followed by radiotherapy in our institution between 1994 and 2007. All patients were newly diagnosed, and those with a prior history of breast cancer, as well as those diagnosed with mixed ductal-lobular types or types other than IDC or ILC, were excluded from the study.
All patients underwent upfront BCS. Patients who received preoperative chemotherapy were not included in the study. If the surgical margins were involved by ductal carcinoma in situ or invasive tumor, a re-excision was performed. Sentinel lymph node biopsies were performed in clinically node-negative patients, and axillary lymph node dissections were performed in clinically node-positive or sentinel lymph node-positive patients.
Adjuvant chemotherapy was recommended for node-positive patients as well as those with tumors larger than 1 cm or basal-like subtypes. The chemotherapy regimens consisted of cyclophosphamide, methotrexate, and 5-fluorouracil (CMF); doxorubicin and cyclophosphamide (AC); 5-fluorouracil, doxorubicin, and cyclophosphamide (FAC); and AC followed by paclitaxel. Anthracycline-based chemotherapy was adopted in 2001 and replaced CMF chemotherapy beginning in 2004. Hormone therapy was recommended for patients with hormone receptor-positive tumors.
Radiation therapy was started 4 to 6 weeks after surgery or completion of adjuvant chemotherapy or was delivered between AC and paclitaxel. The radiation field was matched to the tangential field covering the whole breast and the lower part of the level I and II axillary lymph nodes. The field-in-field technique or the wedge was used to improve the dose homogeneity. Supraclavicular fossa irradiation was performed in patients with pathological N2 or high-risk N1 disease. A median dose of 50.4 Gy (range, 50.0-50.4 Gy) at 1.8 to 2.0 Gy per fraction was delivered with 4 or 6 MV photon beams. An electron boost to the tumor bed with a median dose of 10.0 Gy (range, 6.0-12.0 Gy) was delivered to all patients except those with microinvasive carcinomas.
Medical records and pathological reports were retrospectively reviewed to assess clinicopathological features including age, laterality, pathologic stage, nuclear grade, ER status, progesterone receptor (PR) status, human epidermal growth factor receptor 2 (HER2) status, extensive intraductal carcinoma (EIC), and lymphovascular invasion (LVI). Pathologic stage was classified according to the seventh edition of the American Joint Committee on Cancer Staging Manual [13]. The histologic grade was scored according to the Bloom-Richardson grading system and the Elston-Ellis modification of the Scarff-Bloom-Richardson grading system (Nottingham histologic score system) [141516]. The hormone receptor status, HER2 status, and p53 protein expression were determined by immunohistochemical (IHC) staining. The tumors were classified into three IHC subtypes: luminal (ER- or PR-positive), basal-like (ER-, PR-, and HER2-negative), and erbB-2 overexpressing (ER-, PR-negative, and HER2-positive) [17]. EIC was defined as an intraductal carcinoma occupying more than 25% of the primary tumor with intraductal foci separate from the main tumor mass.
The clinicopathological features of ILC and IDC were compared using Pearson chi-square test. Disease-specific survival (DSS) was measured from the date of surgery to the date of death from breast cancer, and deaths from other cancers or diseases were censored. Disease-free survival (DFS) was measured from the date of surgery to the date of any recurrence or to the date the patient was last known to be recurrence-free. Metachronous contralateral breast cancer was not considered recurrence. Kaplan-Meier analysis and log-rank tests were used to estimate and compare the DSS and DFS. Multivariate analysis was performed using the Cox proportional hazards model. A Bonferroni correction was applied for multiple testing. The SPSS statistical software version 18.0 (SPSS Inc., Chicago, USA) was used for statistical analyses. A p-value of less than 0.05 was considered statistically significant.
Among 1,071 patients with invasive breast cancer, 56 patients (5.2%) were diagnosed with ILC. Table 1 shows the comparison of clinicopathological features between ILC and IDC. There were many cases in which EIC and LVI data were not reported, because it was not obligatory to report these until the development of a unified format for pathology reports in 2005. However, the proportions of cases in which the hormone receptor status and IHC subtype were unreported were less than 10%. The statistical analyses were performed excluding cases with unreported data. There were no statistically significant differences in age, pathologic stage, resection margins, EIC, or HER2 status. Statistically significant differences were found in laterality, nuclear grade, LVI, hormone receptor status, p53 status, and IHC subtype. Bilateral breast cancer was more frequent in patients with ILC than in those with IDC, at 7.1% vs. 1.5%, respectively. ILC was found to have a lower nuclear grade than IDC. There were no cases of ILC with LVI. The proportion of hormone receptor-positive breast cancers was higher in patients with ILC than in those with IDC. With respect to IHC subtypes, the erbB-2 overexpressing subtype was less frequent in ILC, and there were no instances of the basal-like subtype found among patients with ILC.
A total of 825 patients (77.0%) received chemotherapy after BCS. There was no statistically significant difference in regimens between patients with ILC and those with IDC (p=0.494). A total of 699 patients (65.3%) received hormone therapy including tamoxifen or aromatase inhibitors. Among 722 patients (67.4%) with ER- or PR-positive cancers, 676 patients (63.1%) received hormone therapy.
The median follow-up duration, calculated from the date of surgery, was 114 months (range, 5-238 months). During the follow-up period, 105 patients died of breast cancer and 15 patients died of other causes, including other cancers, myocardial infarction, intracranial hemorrhage, and pneumonia. The 10-year DSS and DFS rates were 89.4% and 84.0%, respectively.
Recurrence occurred in 163 patients (15.2%). There were no statistically significant differences in the patterns of recurrence between ILC and IDC (Table 2). Twenty-eight patients (2.6%) developed contralateral breast cancer, which is not defined as recurrence, and all but one of these patients were initially diagnosed with IDC.
On univariate analyses, age, stage, nuclear grade, EIC, LVI, ER status, PR status, HER2 status, p53 status, and IHC subtypes were statistically significant prognostic factors for DSS. Age, stage, nuclear grade, LVI, PR status, HER2 status, and p53 status were statistically significant prognostic factors for DFS (Table 3).
On multivariate analyses, age, LVI, and p53 status were statistically significant prognostic factors for DSS. Age, stage, and LVI were statistically significant prognostic factors for DFS (Table 4).
ILC is the second most common type of invasive breast cancer after IDC. In 2000, Li et al. [18] analyzed the data of the Surveillance, Epidemiology, and End Results (SEER) Program, including 240,018 patients with invasive breast cancer, and reported that 16,476 patients (6.9%) were diagnosed with ILC. In addition, they reported that the incidence rate of ILC increased steadily from 1987 to 1995 in women older than 50 years. Eheman et al. [19] reported on the changing incidences of IDC and ILC in the United States between 1999 and 2004. The incidence of ILC decreased from 11.7% to 9.3%. Interestingly, the authors noted differences in incidence rates according to race. The age-adjusted incidences of ILC were 11.2, 6.6, 4.4, and 3.6 per 100,000 in Caucasians, African-Americans, Asians, and American Indians, respectively. In Korean women, the incidence of ILC was reported as 2% to 3% [23456]. In our study, it was 5.2%, slightly higher than in other Korean studies. However, even considering selection bias, the figure reported in our study was still lower than that in Western women.
Many studies had reported several differences in clinicopathological features between ILC and IDC [78920212223]. Tumor size, tumor grade, hormone receptor status, and incidence of contralateral breast cancer were the most commonly reported differences in various studies. ILCs were larger and had a lower tumor grade than IDCs. Approximately 76% to 93% of ILCs were hormone receptor-positive. Contralateral breast cancer was more common in patients with ILC, with a reported incidence of 14% to 21%. Although several studies reported statistically significant differences in average age between patients with ILC and those with other invasive carcinomas, the age gap was small (less than 3 years). In our study, there were no statistically significant differences in age, pathologic stage, resection margins, EIC, or HER2 status. Statistically significant differences were found in laterality, nuclear grade, LVI, hormone receptor status, p53 status, and IHC subtype. However, these results should be evaluated carefully, because our study included patients who were suitable for BCS, and EIC and LVI were unreported in more than 50% of cases in the patients with ILC.
Several studies reported higher rates of local recurrence after BCS than after mastectomy and suggested mastectomy for patients with ILC [1011]. In a recently published study by Fodor [24], DSS was not affected by the surgical extent, but the 15-year local recurrence-free survival rates were 77% and 89% after BCS and mastectomy, respectively (p=0.005). However, among the 72 patients who underwent BCS, 19 patients (26.0%) did not receive adjuvant radiotherapy. Add itional analysis revealed that the 15-year local recurrence rates for the BCS groups with or without adjuvant radiotherapy were 10% and 53%, respectively (p<0.001). As adjuvant radiotherapy after BCS has been proven in the National Surgical Adjuvant Breast and Bowel Project clinical trial to decrease local recurrence [25], previous results of BCS should be carefully investigated, with this factor taken into consideration.
Many studies have found that there are no differences in survival or local recurrence between patients with ILC and those with IDC after BCS followed by radiotherapy [212627282930]. The 10-year local recurrence rates were found to be 9%-18% and 7%-12% for ILC and IDC, respectively. In our study, while the differences were not statistically significant, there was a trend toward better DSS and DFS in patients with ILC. The 10-year DSS rates were 98.0% and 89.0% in ILC and IDC, respectively (p=0.262), while the 10-year local recurrence rates were 3.6% and 8.8% in ILC and IDC, respectively (p=0.457). The better outcomes might be due to a higher proportion of hormone-positive breast cancers in patients with ILC. The number of patients with ILC was too small to show statistically significant differences.
Our study does have some limitations. First, we included only patients who underwent BCS, and this population does not represent the entire spectrum of invasive breast cancer patients. Second, although LVI was an independent prognostic factor in both univariate and multivariate analyses, it was not reported in 695 cases (64.9%). Depending on the LVI status in the cases in which it was unreported, the results of the statistical analyses could change. Finally, there was an evolution in the chemotherapy regimens over time, from CMF to anthracycline-based chemotherapy, and this change could have affected regional or distant recurrences.
In conclusion, the incidence of ILC in our study was 5.2%, slightly higher than that observed in other Korean studies, but still lower than those reported in Western studies. Bilateral breast cancer, lower nuclear grade, and hormone receptor-positive breast cancer were more frequent in patients with ILC than in those with IDC. There were no cases of LVI or the basal-like subtype among the patients with ILC. There were no statistically significant differences in the patterns of treatment failure. The development of metachronous contralateral breast cancer was more frequent in patients with IDC (n=27). Only one patient with ILC developed contralateral breast cancer, with ductal carcinoma in situ. Although the difference was not statistically significant, there was a trend toward better DSS and DFS rates in patients with ILC.
Figures and Tables
Table 1
Comparison of clinicopathological features between invasive ductal and lobular carcinomas of the breast

EIC=extensive intraductal component; LVI=lymphovascular invasion; HER2=human epidermal growth factor receptor 2; IHC=immunohistochemistry; CMF=cyclophosphamide, methotrexate and 5-flurouracil; AC=doxorubicin and cyclophosphamide; FAC=5-fluorouracil, doxorubicin and cyclophosphamide; ACT=doxorubicin, cyclophosphamide, and paclitaxel.
*Median (range); †Pearson chi-square test was performed excluding unreported or indeterminate cases.
Table 2
Comparison of patterns of recurrence between invasive lobular carcinoma (ILC) and invasive ductal carcinoma (IDC)
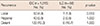
| Recurrence |
IDC (n = 1,015) No. (%) |
ILC (n = 56) No. (%) |
p-value |
|---|---|---|---|
| Local | 50 (4.9) | 1 (1.8) | 0.513 |
| Regional | 40 (3.9) | 2 (3.6) | 1.000 |
| Distant | 122 (12.0) | 6 (10.7) | 1.000 |
Table 3
Univariate analysis: variables associated with disease-specific survival and disease-free survival

Table 4
Multivariate analysis: variables associated with disease-specific survival and disease-free survival

References
1. Wellings SR. A hypothesis of the origin of human breast cancer from the terminal ductal lobular unit. Pathol Res Pract. 1980; 166:515–535.

2. Lee JH, Park S, Park HS, Park BW. Clinicopathological features of infiltrating lobular carcinomas comparing with infiltrating ductal carcinomas: a case control study. World J Surg Oncol. 2010; 8:34.

3. Jung YS, Na KY, Kim KS, Ahn SH, Lee SJ, Park HK, et al. Nation-wide Korean breast cancer data from 2008 using the breast cancer registration program. J Breast Cancer. 2011; 14:229–236.

4. Ko BS, Noh WC, Kang SS, Park BW, Kang EY, Paik NS, et al. Changing patterns in the clinical characteristics of Korean breast cancer from 1996-2010 using an online nationwide breast cancer database. J Breast Cancer. 2012; 15:393–400.

5. Kim Z, Min SY, Yoon CS, Lee HJ, Lee JS, Youn HJ, et al. The basic facts of Korean breast cancer in 2011: results of a nationwide survey and breast cancer registry database. J Breast Cancer. 2014; 17:99–106.

6. Jung SY, Jeong J, Shin SH, Kwon Y, Kim EA, Ko KL, et al. The invasive lobular carcinoma as a prototype luminal A breast cancer: a retrospective cohort study. BMC Cancer. 2010; 10:664.

7. Sastre-Garau X, Jouve M, Asselain B, Vincent-Salomon A, Beuzeboc P, Dorval T, et al. Infiltrating lobular carcinoma of the breast: clinicopathologic analysis of 975 cases with reference to data on conservative therapy and metastatic patterns. Cancer. 1996; 77:113–120.

8. Orvieto E, Maiorano E, Bottiglieri L, Maisonneuve P, Rotmensz N, Galimberti V, et al. Clinicopathologic characteristics of invasive lobular carcinoma of the breast: results of an analysis of 530 cases from a single institution. Cancer. 2008; 113:1511–1520.

9. Pestalozzi BC, Zahrieh D, Mallon E, Gusterson BA, Price KN, Gelber RD, et al. Distinct clinical and prognostic features of infiltrating lobular carcinoma of the breast: combined results of 15 International Breast Cancer Study Group clinical trials. J Clin Oncol. 2008; 26:3006–3014.

10. du Toit RS, Locker AP, Ellis IO, Elston CW, Nicholson RI, Robertson JF, et al. An evaluation of differences in prognosis, recurrence patterns and receptor status between invasive lobular and other invasive carcinomas of the breast. Eur J Surg Oncol. 1991; 17:251–257.
11. Hussien M, Lioe TF, Finnegan J, Spence RA. Surgical treatment for invasive lobular carcinoma of the breast. Breast. 2003; 12:23–35.

12. Singletary SE, Patel-Parekh L, Bland KI. Treatment trends in early-stage invasive lobular carcinoma: a report from the National Cancer Data Base. Ann Surg. 2005; 242:281–289.
13. Compton CC, Byrd DR, Garcia-Aguilar J, Kurtzman SH, Olawaiye A, Washington MK. AJCC Cancer Staging Atlas: A Companion to the Seventh Editions of the AJCC Cancer Staging Manual and Handbook. 2nd ed. New York: Springer;2012.
14. Elston CW, Ellis IO. Pathological prognostic factors in breast cancer I The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology. 1991; 19:403–410.

15. Genestie C, Zafrani B, Asselain B, Fourquet A, Rozan S, Validire P, et al. Comparison of the prognostic value of Scarff-Bloom-Richardson and Nottingham histological grades in a series of 825 cases of breast cancer: major importance of the mitotic count as a component of both grading systems. Anticancer Res. 1998; 18:571–576.
16. Bloom HJ, Richardson WW. Histological grading and prognosis in breast cancer: a study of 1409 cases of which 359 have been followed for 15 years. Br J Cancer. 1957; 11:359–377.

17. Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ, et al. Strategies for subtypes: dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011; 22:1736–1747.

18. Li CI, Anderson BO, Porter P, Holt SK, Daling JR, Moe RE. Changing incidence rate of invasive lobular breast carcinoma among older women. Cancer. 2000; 88:2561–2569.

19. Eheman CR, Shaw KM, Ryerson AB, Miller JW, Ajani UA, White MC. The changing incidence of in situ and invasive ductal and lobular breast carcinomas: United States, 1999-2004. Cancer Epidemiol Biomarkers Prev. 2009; 18:1763–1769.

20. Molland JG, Donnellan M, Janu NC, Carmalt HL, Kennedy CW, Gillett DJ. Infiltrating lobular carcinoma: a comparison of diagnosis, management and outcome with infiltrating duct carcinoma. Breast. 2004; 13:389–396.

21. Silverstein MJ, Lewinsky BS, Waisman JR, Gierson ED, Colburn WJ, Senofsky GM, et al. Infiltrating lobular carcinoma: is it different from infiltrating duct carcinoma. Cancer. 1994; 73:1673–1677.

22. Winchester DJ, Chang HR, Graves TA, Menck HR, Bland KI, Winchester DP. A comparative analysis of lobular and ductal carcinoma of the breast: presentation, treatment, and outcomes. J Am Coll Surg. 1998; 186:416–422.

23. Arpino G, Bardou VJ, Clark GM, Elledge RM. Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res. 2004; 6:R149–R156.

24. Fodor J, Major T, Toth J, Sulyok Z, Polgar C. Comparison of mastectomy with breast-conserving surgery in invasive lobular carcinoma: 15-year results. Rep Pract Oncol Radiother. 2011; 16:227–231.

25. Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002; 347:1227–1232.

26. Weiss MC, Fowble BL, Solin LJ, Yeh IT, Schultz DJ. Outcome of conservative therapy for invasive breast cancer by histologic subtype. Int J Radiat Oncol Biol Phys. 1992; 23:941–947.

27. Peiro G, Bornstein BA, Connolly JL, Gelman R, Hetelekidis S, Nixon AJ, et al. The influence of infiltrating lobular carcinoma on the outcome of patients treated with breast-conserving surgery and radiation therapy. Breast Cancer Res Treat. 2000; 59:49–54.

28. Mersin H, Yildirim E, Gülben K, Berberoglu U. Is invasive lobular carcinoma different from invasive ductal carcinoma. Eur J Surg Oncol. 2003; 29:390–395.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download