Abstract
Breast cancer is the most common primary source of orbital metastasis. Metastasis occurs through hematogenous spread and predominantly involves the choroid. We present a case of a metastatic subconjunctival mass associated with primary breast cancer. To our knowledge, this is the first reported case of its kind. A 41-year-old woman presented with complaints of conjunctival injection and a foreign body sensation in the left eye. She had a history of breast cancer and had been treated 2 years previously with modified radical mastectomy followed by adjuvant radiotherapy and chemotherapy. Slit-lamp examination showed a cystic mass under the temporal bulbar conjunctiva, associated with dilated overlying conjunctival vessels. An excisional biopsy revealed a poorly differentiated adenocarcinoma. Positron emission tomography examination for systemic malignancy revealed multiple systemic metastasis. Metastatic disease should be considered in the differential diagnosis of subconjunctival lesions, and ophthalmic manifestations can play an important role in the detection of metastatic spread of a known primary breast cancer.
The rate of breast cancer incidence has increased by approximately 33% over the past 30 years [1,2]. In patients with ocular metastasis, the primary tumor is generally diagnosed prior to ocular manifestation. The average interval between primary diagnosis and discovery of the metastatic lesion is generally 4.5 to 6.5 years, but delays of over 20 years have been reported [3]. Breast cancer generally metastasizes to the orbit via hematogenous spread and predominantly involves the choroid [4], whereas only a limited number of conjunctival breast cancer metastasis cases have been reported. To our knowledge, cases of subconjunctival breast cancer metastasis have not been previously described in the literature, so we present the first reported case of a metastatic subconjunctival mass associated with primary breast cancer.
A 41-year-old woman visited our clinic complaining of conjunctival injection and a foreign body sensation in the left eye, with no other systemic symptoms. She was treated with antibiotics and steroid eye solutions at a local eye hospital, and was later referred to our clinic because of disease progression. She had a history of breast cancer and had been treated 2 years previously with modified radical mastectomy followed by adjuvant radiotherapy (50.4 Gy, 28 cycles; 1,411.2 Gy in total) and six cycles of chemotherapy (cyclolphosphamide, methotrexate, and 5-fluorouracil). Pathological examination revealed an invasive ductal carcinoma (stage T2N1M0) that was moderately differentiated, negative for estrogen receptor/progesterone receptor expression, cytokeratin 5/6, and c-erb-B2, and positive for p53 (positive reaction in more than 51% of tumor cells) and Ki-67 expression (labeling index of 31% in tumor cells). Axillary lymph node metastasis was found in 1 out of 18 resected nodes.
The best-corrected visual acuity was 20/20 in the right eye and 16/20 in the left eye, with an intraocular pressure of 9 mm Hg and 7 mm Hg in the right and left eyes, respectively. A slit lamp bi-microscopic examination showed a cystic mass under the temporal bulbar conjunctiva, associated with dilated overlying conjunctival vessels (Figure 1). The anterior chamber, lens, and media were clear, no signs of choroid or retina involvement were observed, and extraocular muscle movement was not limited. Informed consent was obtained from the patient before the surgery. An excisional biopsy revealed a poorly differentiated adenocarcinoma positive for carcinoembryonic antigen and p53, and negative for gross cystic disease fluid protein 15, thyroid transcription factor-1, and estrogen receptor (Figure 2). Positron emission tomography examination for systemic malignancy revealed multiple bony metastasis with bone marrow infiltration, multiple muscular and subcutaneous metastasis, multiple lung metastasis with metastatic subcarinal and left hilar lymph nodes, mesenteric metastasis, and pancreatic metastasis.
Metastasis to the eye develop most commonly from cancer of the breast (40%) and the lung (29%) [5]. Freedman and Folk [6] reviewed the charts of 112 patients (141 eyes) who presented with metastasis to the eye or orbit and revealed that breast cancer was the most common primary tumor (49.1%). Approximately 5.8% to 9.2% of visually asymptomatic patients with advanced or metastatic breast cancer develop ocular metastasis, which typically develop 2 to 5 years after the primary tumor has been detected [7,8,9]. In our case, an ocular metastasis was found 2 years after the primary tumor was detected.
The subconjunctival space is a potential space between the conjunctiva and sclera that does not normally contain blood vessels. Further, unlike the well-vascularized conjunctiva, the scleral stroma mostly consists of bundles of collagen fibers, occasionally accompanied by blood vessels and fibroblasts. As breast cancer metastasizes via the bloodstream, ocular metastasis tend to be located preferentially in the posterior uvea [10]. Metastatic subconjunctival masses are therefore very rare and, consequently, they can be easily mischaracterized as benign masses that are independent of the breast cancer. Although the precise mechanism is unclear, a sclera stromal blood vessel might have played a role in the metastasis case reported here.
Cancer metastasis to the eye are associated with a poor clinical prognosis, regardless of the type of primary cancer, with an average survival rate of only 15 months [6,11]. When breast cancer metastasizes to the eye, the risk of it spreading to the brain or central nervous system increases significantly. Although many patients die due to systemic disease, up to half of the patients die due to intracranial progression. The prognosis of patients with brain metastasis is poor, with a median survival time of 1 to 2 months in untreated patients and 3 to 6 months in patients treated with radiotherapy [12]. If the metastasis is detected early, metastatic lesions can be treated successfully with modalities such as external beam radiotherapy, radioactive plaque brachytherapy, and immunotherapy [13]. Although our patient did not have brain metastasis, the treatment time was delayed due to a late diagnosis. Therefore, metastatic disease should be considered in the differential diagnosis of subconjunctival lesions, and ophthalmic manifestations can play an important role in the detection of metastatic spread of a known primary breast cancer.
Figures and Tables
 | Figure 1The slit lamp bi-microscopic finding of subconjunctival mass. A cystic mass was discovered under the temporal bulbar conjunctiva, associated with dilated overlying conjunctival vessels. |
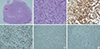 | Figure 2Histopathologic examination of the biopsy specimen. (A) Section of biopsy specimen lined by adjacent sclera (H&E stain, ×40). Sclera stromal vessels containing red blood cells were also noted (arrow). (B) Increased nuclear size with increased nuclear/cytoplasmic ratio. Increased pleomorphism. Lack of differentiation (H&E stain, ×400). (C) Immunohistochemical staining of tumor cells, suggesting a metastatic adenocarcinoma from breast cancer (immunohistochemical staining for carcinoembryonic antigen, ×200). (D) Immunohistochemical staining of tumor cells, suggesting a metastatic adenocarcinoma from breast cancer (immunohistochemical staining for p53, ×200). (E) Immunohistochemical staining of tumor cells, suggesting a metastatic adenocarcinoma from breast cancer (immunohistochemical staining for gross cystic disease fluid protein 15, ×200). (F) Immunohistochemical staining of tumor cells, suggesting a metastatic adenocarcinoma from breast cancer (immunohistochemical staining for estrogen receptor, ×200). |
References
1. Tijl J, Koornneef L, Eijpe A, Thomas L, Gonzalez DG, Veenhof C. Metastatic tumors to the orbit: management and prognosis. Graefes Arch Clin Exp Ophthalmol. 1992; 230:527–530.
2. Kang E, Kim SW. The Korean hereditary breast cancer study: review and future perspectives. J Breast Cancer. 2013; 16:245–253.

3. Stevens RJ, Rusby JE, Graham MD. Periorbital cellulitis with breast cancer. J R Soc Med. 2003; 96:292–294.

4. Wickremasinghe S, Dansingani KK, Tranos P, Liyanage S, Jones A, Davey C. Ocular presentations of breast cancer. Acta Ophthalmol Scand. 2007; 85:133–142.

5. Ferry AP, Font RL. Carcinoma metastatic to the eye and orbit. I. A clinicopathologic study of 227 cases. Arch Ophthalmol. 1974; 92:276–286.
6. Freedman MI, Folk JC. Metastatic tumors to the eye and orbit: patient survival and clinical characteristics. Arch Ophthalmol. 1987; 105:1215–1219.
7. Fenton S, Kemp EG, Harnett AN. Screening for ophthalmic involvement in asymptomatic patients with metastatic breast carcinoma. Eye (Lond). 2004; 18:38–40.

8. Albert DM, Rubenstein RA, Scheie HG. Tumor metastasis to the eye. I. Incidence in 213 adult patients with generalized malignancy. Am J Ophthalmol. 1967; 63:723–726.
9. Mewis L, Young SE. Breast carcinoma metastatic to the choroid: analysis of 67 patients. Ophthalmology. 1982; 89:147–151.
10. Frank KW, Sugar HS, Sherman AI, Beckman H, Thoms S. Anterior segment metastases from an ovarian choriocarcinoma. Am J Ophthalmol. 1979; 87:778–782.

11. Font RL, Ferry AP. Carcinoma metastatic to the eye and orbit. III. A clinicopathologic study of 28 cases metastatic to the orbit. Cancer. 1976; 38:1326–1335.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download