Abstract
Ectopic breast tissue can occur anywhere along the incompletely regressed mammary ridge. Among the various types of breast choristoma, ectopic breast tissue, which has only glandular tissue without a nipple or areola, is most commonly detected in axillary areas. However, ectopic breast cancer is often not detected until significant clinical symptoms have been revealed, or diagnosis is delayed. Furthermore, an examination of ectopic breast tissue tends to be omitted from a screening mammography. Especially, the microcalcifications of ectopic breast tissue are difficult to delineate on mammography. Herein, the authors report a case of ectopic breast carcinoma that showed clustered microcalcifications on screening mammography, and discuss the interpretation and implications of microcalcification in ectopic breast tissue.
Incomplete regression of the mammary ridges may result in aberrant breast tissue, which can be classified based on its components [1]. Among the various types of breast choristoma, ectopic breast tissue, comprised of only glandular tissue without a nipple or areola, is most commonly detected in the axillary regions [2,3]. Although ectopic breast tissue does not have a secretory ductal system, it is histologically no different from anatomically normal breast tissue. Ectopic breast tissue therefore shows physiologic and pathogenic processes similar to those of eutopic breast tissue.
Clustered microcalcifications on mammography are a relatively common feature of invasive carcinoma or ductal carcinoma in situ [4,5]. However, the microcalcification of ectopic breast tissue is difficult to delineate on mammography, and is often not detected. Furthermore, most cases of microcalcification in the axillary region occur in lymph nodes [6,7,8].
We report herein a case of ductal carcinoma in situ originating from axillary ectopic breast tissue that had revealed clustered microcalcifications on screening mammography.
A 52-year-old woman with bilateral accessory breast tissue attended a local breast clinic for annual mammography and ultrasonography screening, during which clustered microcalcifications were detected in ectopic breast tissue of the right axillary area. It was decided to maintain observation only with close surveillance, because the mammography findings were assessed as Breast Imaging Reporting and Data System category 3 (Figure 1A, 1B). After 3 months the patient was readmitted to the clinic with a palpable axillary mass. The mass was hard and fixed in the right side of axilla and an irregularly shaped axillary mass including microcalcifications, was identified on ultrasonography. A breast surgeon performed an excision biopsy of the axillary mass, and clustered microcalcifications were identified on specimen mammography (Figure 1C). Histologic observations revealed that the mammary ducts, within the fibrofatty stroma, were filled with and distended by a solid epithelial proliferation. The lesion measured 1.5 cm in the largest dimension. Necrosis and multifocal microcalcification were noted (Figure 2A), and the epithelial cells showed a moderate to high degree of nuclear atypia (Figure 2B). The patient was diagnosed as having high-grade ductal carcinoma in situ and was referred to our department for additional procedures.
Preoperative evaluation via positron emission tomography and computed tomography did not reveal any metastatic lesions. The patient underwent a wide local excision of the axillary ectopic breast tissue with a safety margin around the cavity of 1 cm; sampling of sentinel lymph nodes was also performed. For the evaluation of sentinel lymph nodes, 2 mL of a blue dye (indigo carmine) was injected into the peritumoral site. The weight of the excised ectopic breast tissue was 60 g; the contained microcalcifications were identified on specimen mammography.
In a section of the excised specimen, a cavitary lesion was noted along with focal fat necrosis due to the excision procedure. Remnant tumor was not clearly detected on macroscopic examination, but on microscopic examination, remnant tumor measuring 0.5 cm in maximum diameter was observed around the cavity; histologic findings were similar to those for the excision biopsy. And there was no indication of metastasis to the lymph nodes among seven sentinel lymph nodes biopsied. Immunohistochemical assay showed positive and negative staining for the estrogen and progesterone receptors, respectively, and strong positive staining confirmed overexpression of the c-erbB-2 protein. Tamoxifen was administrated as adjuvant hormonal therapy. The patient continues to undergo surveillance up to 3 months after surgery, with no specific problems.
Ectopic breast tissue, a choristoma of the breast, can occur anywhere along the mammary ridge, and almost every form of breast disease can occur in ectopic breast tissue. Primary breast carcinoma arising from accessory breast tissue has been reported in 60% to 70% of all forms of ectopic breast tumor [2,9]. And the invasive ductal carcinoma is the most frequent histologic variant of primary ectopic cancer [10,11]. However, ectopic breast cancer is not easily detected because of the late expression of pathologic symptoms, and is commonly misdiagnosed as axillary lymph node disease, lipoma, or a sebaceous cyst [12]. Furthermore, we report a microcalcification in the axillary region, revealed on mammography; such findings could lead to ectopic breast cancer being overlooked or misdiagnosed as a calcification of the axillary lymph nodes. As late detection of ectopic breast cancer may lead to a worse prognosis, a precancerous sign or symptom should not be ignored. We wish to report the present case because of its rarity, as well as to highlight the implications of microcalcifications being discovered during the regular surveillance of ectopic breast tissue when an abnormality is detected on imaging.
When an abnormal image or symptom of ectopic breast tissue is noted, it should be evaluated in the same manner as for eutopic breast tissue. If a palpable mass is detected in ectopic breast tissue, a needle biopsy can be helpful for a differential diagnosis. If a malignant microcalcification is detected on mammographic imaging of aberrant breast tissue, it should be evaluated as to whether the calcification is located in a choristoma of the breast or a lymph node; a biopsy should be performed for further evaluation.
A malignant microcalcification on mammography strongly correlates with ductal carcinoma in situ or invasive cancer [2,4,5]. When a malignant microcalcification is detected on mammography, a needle biopsy or excision biopsy should be performed to enable a correct diagnosis. This principle would also apply to ectopic breast tissue, because the components of such tissue are the same as those of an anatomically normal breast [2].
When ectopic breast cancer has been diagnosed, it is classified according to the TNM staging system used for primary breast carcinoma [13]. There is a clear distinction between ectopic breast cancer and occult breast cancer that presents in axillary lymph nodes; this is the reason for a thorough examination to accurately establish the location of a microcalcification. Ectopic breast cancer should be managed based on the treatment protocols for primary breast cancer, in contrast to the management of occult breast cancer. Although Francone et al. [3] strongly recommended the preventive excision of ectopic mammary tissue, the incidence of ectopic breast cancer is only 0.2% to 0.6% of all breast cancers, whereas the incidence of postoperative complications (e.g., severe scarring, infection in the remaining sweat glands, pain, or discomfort) is reported to be as high as 4% to 10% [14,15]. However, preventive removal of ectopic breast tissue should be performed in cases that show abnormal signs or symptoms; if it were not performed, routine screening would be sufficient. A wide and complete resection of ectopic breast tissue is indicated after ectopic breast cancer has been diagnosed, and an evaluation of axillary lymph nodes is certainly indicated if the ectopic breast cancer occurs in the axillary region. Ectopic breast cancer can spread to the axillary lymph nodes more rapidly than a typical breast cancer [13]. Based on the TNM staging and characteristics of an ectopic breast cancer, adjuvant chemotherapy or radiotherapy can be administered, and hormonal therapy or targeted therapy can also be used, in accordance with the status of the relevant biological markers.
Although ectopic breast cancer is very rare, diagnostic modalities are usually the same as for typical breast cancer. However, it is not easily detected if a significant clinical symptom is not obvious, which may result in a delayed diagnosis and poor prognosis. A patient with aberrant breast tissue should be carefully evaluated with regard to both eutopic and ectopic tissue. When an abnormal finding is detected, such as clustered microcalcifications on mammography or a clinically palpable mass in ectopic breast tissue, a thorough evaluation should be undertaken.
Despite its rarity, symptomatic ectopic breast cancer is relatively easy to diagnose because of its similarity to typical breast cancer. However, it is less easily delineated on diagnostic imaging, leading to a late diagnosis and poor prognosis. Examination of accessory or ectopic breast tissue in affected patients should take place at the same time as the evaluation of eutopic breast tissue. Suspicious lesions, including microcalcification, should be followed up with close surveillance.
Figures and Tables
Figure 1
Mammographic findings of ectopic breast cancer. (A) Aberrant breast tissue with clustered microcalcifications (dot circle) is detected on right axilla. (B) Magnified mammographic image of ectopic breast tissue with microcalcifications. A clustered microcalcification is well observed on ectopic breast tissue. (C) Mammographic findings of removed breast tissue. Multifocal microcalcification is apparent in two separately removed ectopic breast tissue specimens.
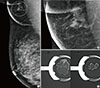
Figure 2
Histopathologic findings of ectopic breast carcinoma. (A) Ductal epithelial proliferative lesion with multiple foci of necrosis and microcalcification is noted (H&E stain, ×20). (B) The tumor cells show moderate to high degree of nuclear atypia characteristic of high-grade ductal carcinoma in situ. Microcalcification is well observed in the tumor cell nests (H&E stain, ×100).

References
1. Kajava Y. The proportions of supernumerary nipples in the Finnish population. Duodecim. 1915; 31:143–170.
2. Marshall MB, Moynihan JJ, Frost A, Evans SR. Ectopic breast cancer: case report and literature review. Surg Oncol. 1994; 3:295–304.

3. Francone E, Nathan MJ, Murelli F, Bruno MS, Traverso E, Friedman D. Ectopic breast cancer: case report and review of the literature. Aesthetic Plast Surg. 2013; 37:746–749.

4. Stomper PC, Geradts J, Edge SB, Levine EG. Mammographic predictors of the presence and size of invasive carcinomas associated with malignant microcalcification lesions without a mass. AJR Am J Roentgenol. 2003; 181:1679–1684.

5. Venkatesan A, Chu P, Kerlikowske K, Sickles EA, Smith-Bindman R. Positive predictive value of specific mammographic findings according to reader and patient variables. Radiology. 2009; 250:648–657.

6. Singer C, Blankstein E, Koenigsberg T, Mercado C, Pile-Spellman E, Smith SJ. Mammographic appearance of axillary lymph node calcification in patients with metastatic ovarian carcinoma. AJR Am J Roentgenol. 2001; 176:1437–1440.

7. Burdeny DA, Reed MH, Ferguson CA. Calcification of axillary lymph nodes following BCG vaccination. Can Assoc Radiol J. 1989; 40:92–93.
8. Chen SW, Bennett G, Price J. Axillary lymph node calcification due to metastatic papillary carcinoma. Australas Radiol. 1998; 42:241–243.

9. Amsler E, Sigal-Zafrani B, Marinho E, Aractingi S. Ectopic breast cancer of the axilla. Ann Dermatol Venereol. 2002; 129:1389–1391.
10. Yerra L, Karnad AB, Votaw ML. Primary breast cancer in aberrant breast tissue in the axilla. South Med J. 1997; 90:661–662.

11. Nihon-Yanagi Y, Ueda T, Kameda N, Okazumi S. A case of ectopic breast cancer with a literature review. Surg Oncol. 2011; 20:35–42.

12. Das DK, Gupta SK, Mathew SV, Sheikh ZA, al-Rabah NA. Fine needle aspiration cytologic diagnosis of axillary accessory breast tissue, including its physiologic changes and pathologic lesions. Acta Cytol. 1994; 38:130–135.
13. Bakker JR, Sataloff DM, Haupt HM. Breast cancer presenting in aberrant axillary breast tissue. Community Oncol. 2005; 2:117–122.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download