Abstract
Purpose
Neoadjuvant chemotherapy (NC) is yet to be established as the definitive treatment regimen for locally advanced breast cancer (LABC). The aim of this study was to determine the efficacy and toxicity of NC with epirubicin and paclitaxel.
Methods
Between March 2007 and January 2009, 50 patients with LABC were enrolled in an open-label, phase II, multicenter study carried out at five distinct institutions. All patients were scheduled to receive four cycles of 60 mg/m2 epirubicin and 175 mg/m2 paclitaxel every 3 weeks, preoperatively, unless they developed profound side effects or disease progression. After curative surgery, two additional cycles of chemotherapy were administered to patients who had shown a positive response to NC.
Results
In all, 196 cycles of chemotherapy were administered preoperatively; 47 of the 50 patients (94%) underwent all four cycles of designated treatment. Complete disappearance of invasive foci of the primary tumor, and negative axillary lymph nodes were confirmed in eight patients (16.0%), post operation. The cumulative 5-year disease-free survival rate was 70.0% for patients with complete remission (CR) and partial remission (PR), and 33.3% for patients with stable disease (SD) and progressive disease (PD) (p=0.018). The cumulative 5-year overall survival was 90.0% for patients who achieved CR and PR and 55.6% for patients who had SD and PD (p=0.001). Neutropenia (42.0%) was the most common grade 3/4 toxicity. However, none of the toxicities resulted in cessation of the treatment.
Neoadjuvant chemotherapy (NC) is a standard treatment for locally advanced breast cancer (LABC) and large operable breast tumors, due to its safety and effectiveness as shown in previous studies [1,2,3]. Despite an increase in clinical trials, NC is yet to be established as the definitive treatment regimen for LABC. In order to optimize future treatment, it is important to determine the optimal combination of taxanes with anthracyclines (doxorubicin and epirubicin), which are the most active agents in advanced breast cancer treatment [4]. As previous studies have shown, in both locally advanced and operable breast cancers, long-term survival can be predicted by the pathologic complete response (pCR) to NC [1,2,5,6]; pCR ranges from 5% to 15% after anthracycline-based NC, and this frequency improves to a range of 15% to 34% upon adding taxane [6]. Therefore, combinations of these two drugs need to be developed to facilitate clinical investigation. Several combinations of doxorubicin and paclitaxel have been evaluated in previous studies, covering a variety of doses and schedules of administration [3,7]. However, the concomitant administration of paclitaxel and doxorubicin is associated with a relatively high probability of severe cardiotoxic events, despite its success in the remission of cancer. When administered concomitantly, interactions between doxorubicin and paclitaxel are apparently responsible for the high cardiotoxicity, arising from the pharmacokinetic modifications of doxorubicin and its cardiotoxic metabolites [8]. The increased incidence of cumulative dose-related cardiotoxicity is a potential limitation in the long-term administration of this combination of drugs. At similar dosages, epirubicin is significantly less cardiotoxic than doxorubicin. Furthermore, paclitaxel does not appear to play a significant role in epirubicin metabolism, when they are combined for treatment [9]. Although chronic therapy is limited, data indicate that epirubicin (4'-epidoxorubicin) may be administered in cumulatively higher doses than doxorubicin, before it triggers the onset of cardiotoxicity and subsequent termination of chemotherapy [4,10]. The aim of this study was to determine the efficacy and toxicity of concomitant epirubicin and paclitaxel (ET) NC.
This open label, phase II, multicenter study enrolled 50 eligible participants, who received treatment at five distinct institutions. Each Institutional Review Board approved the study; in addition, each patient provided the required informed consent documentation in writing (IRB number: 1001-15). The participating women ranged in age from 20 to 70 years. Eligibility criteria included the presence of stage III breast cancer as defined by the American Joint Committee on Cancer (sixth edition), and for the cancer to be entirely untreated prior to this study. The requirements to determine whether the patients met adequate performance status from the Eastern Cooperative Oncology Group (a performance status ≤1), and including hematologic, renal, and liver functions are detailed in the following sentences. Requirements for the hematologic function included hemoglobin levels of greater than or equal to 10 g/dL, absolute neutrophil counts of ≥1.5×109/L, and platelet counts of ≥100×109/L. For the renal function, serum creatinine was required to be within the standard limits. Finally, for the liver function, aspartate aminotransferase, alanine transaminase, and alkaline phosphatase were all required to have levels of ≤1.5 times the maximum limit of the standard levels, and bilirubin levels were required to be within the normal range. Each patient was required to be free of metastatic disease. Participants with any evidence of cardiac disease or a history of malignancy were excluded from this study.
Patients were scheduled to undergo preoperative treatment with four cycles of 60 mg/m2 epirubicin and 175 mg/m2 paclitaxel every 3 weeks unless they developed profound side effects or disease progression. Patients were first administered epirubicin over a 15- to 20-minute interval, followed immediately by a 3-hour intravenous infusion of paclitaxel diluted in 500 mL of 5% dextrose. The paclitaxel was delivered via a polyethylene-lined tube, containing a cellulose acetate 0.22-µm in-line filter. In the premedication phase, 20 mg dexamethasone was administered orally to patients, at 6 and 12 hours prior to paclitaxel infusion. To conclude the premedication phase, 300 mg cimetidine (an alternative of 50 mg ranitidine) and 50 mg diphenhydramine were both administered intravenously, 30 minutes before the paclitaxel infusion. Antiemetics were administered to patients according to the guidelines set by the individual institutions. Prophylactic use of the granulocyte colony-stimulating factor was not permitted. Patients received further chemotherapy, with a 25% reduction in dosage for both epirubicin and paclitaxel upon occurrence of febrile neutropenia or nonhematologic grade 3/4 toxicity; this excluded alopecia. In case the hypersensitivity reaction was deemed clinically significant, paclitaxel infusion was discontinued and appropriate supportive measures were taken. Operations were performed within 3 weeks of administering the fourth cycle of NC. After curative surgery, two additional cycles of the identical chemotherapy regimen were administered in patients who showed objective response to NC. Subsequently, patients received radiotherapy, trastuzumab, or hormone therapy, based on their risk assessment, and human epidermal growth factor receptor 2 and the hormone receptor status.
Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1) was used for assessing the clinical response [11]; pCR was achieved when there was no residual invasive cancer in the breast, including or excluding ductal carcinoma in situ (DCIS), and there was no evidence of nodal involvement with invasive cancer in the surgically removed specimens.
Toxicity was evaluated according to National Cancer Institute Common Toxicity Criteria (NCI CTC) version 2.0. All patients underwent echocardiograms for evaluating their left ventricular ejection fraction, prior to commencing NC, and after four cycles of NC.
To calculate the dose intensity for each agent, we divided the total dosage by the total number of treatment weeks. To obtain the average relative total dose intensity (RDI), we calculated the average delivered dose of the scheduled chemotherapy treatment per week as a percentage of the target dosage. The Kaplan-Meier method was used to calculate the disease-free interval (DFS) and overall survival (OS). By applying the log-rank test, we compared the survival curves from different groups. This study used SPSS version 15.0 (SPSS Inc., Chicago, USA) for statistical analyses.
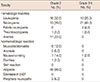
The study enrolled 50 patients with locally advanced breast cancer, between March 2007 and January 2009. Patient characteristics are shown in Table 1. The median age of patients was 47 years, ranging from 27 to 67 years. The median followup time was 73 months, ranging from 12 to 80 months. All patients were assessable for toxicity and efficacy.
During the study, 196 cycles of chemotherapy were administered preoperatively; 47 out of 50 patients (94.0%) received four cycles of the scheduled ET chemotherapy. The study had an average RDI of 96.2% for both paclitaxel and epirubicin. Treatment was terminated in three cases (6.1%) prior to the completion of four cycles, due to progressive disease (PD).
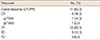
Based on the criteria defined in this study, pCR (ypT0N0+ ypTisN0) was observed in eight patients (16.0%); seven patients (14.0%) showed complete disappearance of the primary tumor (ypT0) with negative axillary lymph nodes. Residual DCIS with complete disappearance of invasive cancer (ypTis) was observed in one patient after the surgery, and 33 patients (66.0%) showed a partial response (PR). The overall response rate was 82%. Stable disease (SD) was observed in six patients (12.0%), and progressive disease in three patients (6.0%) (Table 2).
Data pertaining to grade 2-4 toxicities, based on the NCI CTC v2.0, are presented in Table 3. Neutropenia (42.0%) was the most common grade 3/4 toxicity; however, febrile neutropenia occurred in only two patients (4.0%). None of the toxicities resulted in cessation of the treatment. No cardiac toxicity or peripheral neuropathy was observed during this study, while each patient developed reversible alopecia.
Because of its noted safety and efficacy in treatment, NC has been widely accepted as the treatment of choice for LABC, and for early breast cancer involving an attempt to conserve the breast [2,12]. NC comprising a combination of doxorubicin with paclitaxel is more effective than treatment with anthracycline in combination with other chemotherapeutic agents, or anthracycline alone [13,14]. In two independent studies, Gianni et al. [8], and Dombernowsky et al. [15] have both reported a 20% frequency of congestive heart failure in metastatic breast cancer patients when the patients received doxorubicin and paclitaxel in combination. Therefore, it is particularly important to develop regimens that may decrease the chemotherapy-related toxicity; the doxorubicin analog, epirubicin, is less toxic to the heart even though it possesses a low level of innate cardiotoxicity. However, epirubicin is comparable with doxorubicin in terms of antitumor efficacy [16]; epirubicin is also less myelotoxic than doxorubicin at equimolar dosages [9]. Dose-finding studies involving the epirubicin/paclitaxel combination have not reported significant cardiac toxicity; patients developed grade 3 cardiotoxicity (6%) in only one trial [8,17]. Despite its lower cardiotoxic potential compared to its parent compound, epirubicin is still capable of inducing cardiac failure in 16% to 35% of patients when its cumulative doses exceed 1,000 mg/m2 [18].
The aim of this study was to determine the response and safety of combination chemotherapy with paclitaxel (Genexol®; CJ, Seoul, Korea) plus epirubicin for the treatment of LABC. Previous phase II studies have evaluated concomitant paclitaxel and anthracycline-based NC in breast cancer [14,19]. To the best of our knowledge, there is only one published phase II study that has explored treatment with a combination of epirubicin and paclitaxel for operable breast cancer, to date. The Bellino et al. [20] study enrolled 48 patients with tumors >3 cm in diameter; the treatment regimen comprised four cycles of 200 mg/m2 paclitaxel and 90 mg/m2 epirubicin every 3 weeks, and the authors reported a 12% pCR rate. In the present study, the rate of pCR is higher than that reported in the previous study where 90 mg/m2 epirubicin and 200 mg/m2 paclitaxel were used concomitantly. In this study, we used lower dosages of epirubicin (60 mg/m2) and paclitaxel (175 mg/m2) than in the Bellino et al. [20] study. Most of the participants in this study completed all four cycles of treatment within the scheduled time-frame; each patient received a total dosage of 240 mg/m2 epirubicin, compared with the 360 mg/m2 administered to each patient in the other studies. Similarly, the paclitaxel dosage was lower (175 mg/m2) in comparison with the dosage (200 mg/m2) administered to each patient in the previous study. The combination of epirubicin and paclitaxel shows excellent cardiac tolerability relative to the combination of doxorubicin and paclitaxel. However, the lower rate of epirubicininduced cardiotoxicity in this study cannot be justified solely on the basis of its use in combination with paclitaxel. Two possible explanations include the higher stringency in patient selection, and the lower administered doses of both epirubicin and paclitaxel in this study. Moreover, according to data from the Gianni et al. study, concomitant administration of epirubicin and paclitaxel induces an increase in glucuronidation of epirubicin; this leads to an increase in urinary elimination, and subsequent decrease in the plasma levels of epirubicinol, the cardiotoxic metabolite of epirubicin [8,17]. Conversely, concomitant administration of doxorubicin and paclitaxel causes the nonlinear disposition of doxorubicin. This results in increased plasma concentrations of doxorubicin and its metabolite doxorubicinol; the latter is capable of causing significant myocardial damage. A meta-analysis of collaborative trials in neoadjuvant breast cancer (CTNeoBC) included 12 randomized neoadjuvant trials (n=13,125), and the results indicated that patients who achieved pCR had more favorable long-term outcomes [21]. In the current study, it was found that the responsive group (CR/PR) shows more favorable long-term outcomes than the nonresponsive group (SD/PD) (Figures 1, 2). The progression of cancers during NC is very unusual; in our study, 6.0% (3 of 50 patients) incurred tumor progression during treatment, compared to only 1.4% in the European Organisation for Research and Treatment of Cancer 10902 trial, and 3% in the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-18 trial [12,13,22]. There were no statistically significant differences in DFS and OS between the neoadjuvant and adjuvant groups with respect to the preoperative or postoperative chemotherapy sequencing, according to the findings from the NSABP B-18 trial. However, there is supporting evidence for preoperative chemotherapy in terms of DFS and OS for breast cancer patients under the age of 50 [22]. Considering the younger age of Korean breast cancer patients relative to Western women, it may be advantageous to pursue NC treatment. Although cardiotoxicity is a common and deadly complication when doxorubicin and paclitaxel are used concomitantly for the treatment of breast cancer, it is less of an issue when epirubicin replaces doxorubicin. Concomitant administration of epirubicin and paclitaxel is safe and effective, and the treatment warrants further evaluation.
Figures and Tables
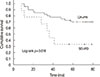 | Figure 1Disease-free survival curves according to response to neoadjuvant chemotherapy using the Kaplan-Meier statistical method. The cumulative 5-year disease-free survival rate was 70.0% for patients with complete remission (CR) and partial remission (PR), and 33.3% for patients with stable disease (SD) and progressive disease (PD) (p=0.018). |
 | Figure 2Overall survival curves according to response to neoadjuvant chemotherapy using the Kaplan-Meier statistical method. The cumulative 5-year overall survival was 90.0% for patients who achieved complete remission (CR) and partial remission (PR) and 55.6% for patients who had stable disease (SD) and progressive disease (PD) (p=0.001). |
References
1. Heys SD, Sarkar T, Hutcheon AW. Primary docetaxel chemotherapy in patients with breast cancer: impact on response and survival. Breast Cancer Res Treat. 2005; 90:169–185.

2. Fisher B, Bryant J, Wolmark N, Mamounas E, Brown A, Fisher ER, et al. Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol. 1998; 16:2672–2685.

3. Buzdar AU. Preoperative chemotherapy treatment of breast cancer: a review. Cancer. 2007; 110:2394–2407.

4. Hortobagyi GN, Holmes FA. Optimal dosing of paclitaxel and doxorubicin in metastatic breast cancer. Semin Oncol. 1997; 24:1 Suppl 3. S4–S7.
5. Kuerer HM, Newman LA, Smith TL, Ames FC, Hunt KK, Dhingra K, et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicinbased neoadjuvant chemotherapy. J Clin Oncol. 1999; 17:460–469.

6. Smith IC, Heys SD, Hutcheon AW, Miller ID, Payne S, Gilbert FJ, et al. Neoadjuvant chemotherapy in breast cancer: significantly enhanced response with docetaxel. J Clin Oncol. 2002; 20:1456–1466.

7. Diéras V, Fumoleau P, Romieu G, Tubiana-Hulin M, Namer M, Mauriac L, et al. Randomized parallel study of doxorubicin plus paclitaxel and doxorubicin plus cyclophosphamide as neoadjuvant treatment of patients with breast cancer. J Clin Oncol. 2004; 22:4958–4965.

8. Gianni L, Munzone E, Capri G, Fulfaro F, Tarenzi E, Villani F, et al. Paclitaxel by 3-hour infusion in combination with bolus doxorubicin in women with untreated metastatic breast cancer: high antitumor efficacy and cardiac effects in a dose-finding and sequence-finding study. J Clin Oncol. 1995; 13:2688–2699.

9. Conte PF, Baldini E, Gennari A, Michelotti A, Salvadori B, Tibaldi C, et al. Dose-finding study and pharmacokinetics of epirubicin and paclitaxel over 3 hours: a regimen with high activity and low cardiotoxicity in advanced breast cancer. J Clin Oncol. 1997; 15:2510–2517.

10. Cersosimo RJ, Hong WK. Epirubicin: a review of the pharmacology, clinical activity, and adverse effects of an adriamycin analogue. J Clin Oncol. 1986; 4:425–439.

11. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009; 45:228–247.

12. van der Hage JA, van de Velde CJ, Julien JP, Tubiana-Hulin M, Vandervelden C, Duchateau L. Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902. J Clin Oncol. 2001; 19:4224–4237.

13. Fisher B, Brown A, Mamounas E, Wieand S, Robidoux A, Margolese RG, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol. 1997; 15:2483–2493.

14. Bear HD, Anderson S, Brown A, Smith R, Mamounas EP, Fisher B, et al. The effect on tumor response of adding sequential preoperative docetaxel to preoperative doxorubicin and cyclophosphamide: preliminary results from National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol. 2003; 21:4165–4174.

15. Dombernowsky P, Boesgaard M, Andersen E, Jensen BV. Doxorubicin plus paclitaxel in advanced breast cancer. Semin Oncol. 1997; 24:5 Suppl 17. S17.
16. Coukell AJ, Faulds D. Epirubicin: an updated review of its pharmacodynamic and pharmacokinetic properties and therapeutic efficacy in the management of breast cancer. Drugs. 1997; 53:453–482.
17. Danesi R, Conte PF, Del Tacca M. Pharmacokinetic optimisation of treatment schedules for anthracyclines and paclitaxel in patients with cancer. Clin Pharmacokinet. 1999; 37:195–211.

18. Jain KK, Casper ES, Geller NL, Hakes TB, Kaufman RJ, Currie V, et al. A prospective randomized comparison of epirubicin and doxorubicin in patients with advanced breast cancer. J Clin Oncol. 1985; 3:818–826.

19. Gogas H, Papadimitriou C, Kalofonos HP, Bafaloukos D, Fountzilas G, Tsavdaridis D, et al. Neoadjuvant chemotherapy with a combination of pegylated liposomal doxorubicin (Caelyx) and paclitaxel in locally advanced breast cancer: a phase II study by the Hellenic Cooperative Oncology Group. Ann Oncol. 2002; 13:1737–1742.

20. Bellino R, Cortese P, Danese S, De Sanctis C, Durando A, Genta F, et al. Epidoxorubicin and paclitaxel as primary chemotherapy for T > 3 cm and T4 breast cancer patients. Anticancer Res. 2000; 20(6C):4825–4828.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download