Abstract
Purpose
The Gail model is one of the most widely used tools to assess the risk of breast cancer. However, it is known to overestimate breast cancer risk for Asian women. Here, we validate the Gail model and the Korean model using Korean data, and subsequently update and revalidate the Korean model using recent data.
Methods
We validated the modified Gail model (model 2), Asian American Gail model, and a previous Korean model using screening patient data collected between January 1999 and July 2004. The occurrence of breast cancer was confirmed by matching the resident registration number with data from the Korean Breast Cancer Registration Program. The expected-to-observed (E/O) ratio was used to validate the reliability of the program, and receiver operating characteristics curve analysis was used to evaluate the program's discriminatory power. There has been a rapid increase in the incidence of breast cancer in Korea, and we updated and revalidated the Korean model using incidence and mortality rate data from recent years.
Results
Among 40,229 patients who were included in the validation, 161 patients were confirmed to have developed breast cancer within 5 years of screening. The E/O ratios and 95% confidence intervals (CI) were 2.46 (2.10-2.87) for the modified Gail model and 1.29 (1.11-1.51) for the Asian American Gail model. The E/O ratio and 95% CI for the Korean model was 0.50 (0.43-0.59). For the updated Korean model, the E/O ratio and 95% CI were 0.85 (0.73-1.00). In the discriminatory power, the area under curve and 95% CI of the modified Gail model, Asian American Gail model, Korean model and updated Korean model were 0.547 (0.500-0.594), 0.543 (0.495-0.590), 0.509 (0.463-0.556), and 0.558 (0.511-0.605), respectively.
The Gail model is one of the most widely used breast cancer risk assessment tools. The original Gail model [1] was developed from case-control subsamples of patients undergoing annual mammographic screening through the Breast Cancer Detection and Demonstration Project (BCDDP). It used five risk factors: age, age at menarche, the number of previous breast biopsies, age at first live birth, and the number of first-degree relatives with breast cancer. The National Surgical Adjuvant Breast and Bowel Project (NSABP) modified this model by excluding the incidence of ductal carcinoma in situ (DCIS) and including the risk factor of atypical ductal hyperplasia. This modified Gail model was used for the inclusion criteria of the NSABP P-1 [2] and P-2 [3] trials.
The incidence of breast cancer in Asian women is lower than that in Western women, and the Gail model for American women has been shown to overestimate the risk of breast cancer for Asian women [4]. As such, it is necessary to develop a breast cancer risk assessment tool especially for Asian women. A web-based breast cancer risk assessment program has been developed for Korean women using Korean data from 1999 to 2001 [5]. It uses seven risk factors: age, body mass index, menopausal status, breast feeding status, family history, previous breast test, and age at first delivery [6]. It can calculate the risk of developing breast cancer in the next 5 or 10 years, up to the age of 64 or 74 years. However, to date, the accuracy of the program has not been validated.
Although the incidence of breast cancer in Korean women is lower than that of American women, it has rapidly increased in recent years [7]. As such, the Korean model [5], developed using old data, it could underestimate the recent risk of developing breast cancer. It is therefore necessary to update the model with more recent Korean data.
In this study, we initially validate the modified Gail, Asian American Gail, and Korean models using data from the Korean Breast Cancer Registration Program. We then update the Korean model using more recent data on breast cancer incidence and mortality in order to improve its performance. We compare the reliability and discriminatory power of the updated Korean model with the modified Gail, Asian American Gail, and original Korean models.
We validated the modified Gail model (model 2) [2], Asian American Gail model [8], and original Korean model [5]. We could not validate the original Gail model (model 1) [1] because it includes the risk of DCIS and its source code is not opened to the public. The characteristics of the risk assessment models validated in this study, and the original Gail model, are summarized in Table 1.
Although the BCDDP was a cohort study, the original Gail model was developed using a case-control subsample of the BCDDP data set [1]. It included 2,852 white cases and 3,146 white controls from the BCDDP data. The original Gail model was subsequently modified to exclude the risk of developing DCIS and to include the risk factor of atypical ductal hyperplasia, this model is referred to as model 2. The modified Gail model uses incidence rate data from the Surveillance, Epidemiology, and End Results (SEER) program rather than that of the BCDDP. The code for the modified Gail model is available from the National Cancer Institute (NCI)'s website (http://dceg.cancer.gov/tools/risk-assessment). The log-relative risks of the modified Gail model are described in Supplementary Table 1.
The Asian American Gail model [8] was developed using data from the Asian American Breast Cancer Study [9]. It includes the data from 589 Asian cases and 952 Asian controls who were living in California and Hawaii. It also uses the SEER data on Asian ethnicity. Similar to the modified Gail model, it uses five risk factors. The code for the Asian American Gail model is also available from the NCI website. The log-relative risks of the Asian American Gail model are described in Supplementary Table 2.
The Korean model [5] was developed using data from a Korean case-control study [6]. After logistic regression analysis, the Korean model selected seven risk factors. In this model, family history is not limited to first-degree relatives, and previous breast tests include biopsy and imaging tests such as mammography and sonography. The Korean model only estimates the risk of invasive breast cancer excluding in situ cancer. The log-relative risks for the Korean model are described in Supplementary Table 3.
After construction of the log-relative risks, all three models followed the procedure presented below. The log-relative risks were converted to relative risks by exponentiation.
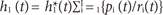
The risk of breast cancer in all three models was calculated using the competing risk analysis proposed by Gail et al. [1]. The baseline hazard rate (h1) refers to the risk for patients who have no risk factors, and was calculated using the age specific breast cancer incidence rate (h1*), relative risk (ri) and the proportions of each risk factor (pi).
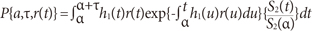
The risk of breast cancer was calculated by the summation of the products of age specific baseline hazard (h1) by relative risks (r) and adjusted by the probability of surviving competing risks (S2). The risk of breast cancer (P) at the age (α) to time (τ) was calculated as follows:
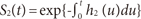
The probability of surviving competing risk (S2) was calculated using the mortality of other causes except breast cancer (h2).
The incidence rate used for the modified Gail model was estimated by using SEER data from 1983 to 1987, whereas the Asian American Gail model used 1998 SEER data. The mortality rate used for the modified Gail model was calculated using National Center for Health Statistics (NCHS) data from 1985 to 1987, whereas the Asian American Gail model used NCHS data from 1998. The Korean model uses incidence and mortality rate data from the Korean Statistical Information System for the years 1999 to 2001 (Table 1).
To evaluate each of the three breast cancer risk assessment models, we used data from breast cancer screening patients at the Women's Healthcare Center of Cheil General Hospital from January 1999 to July 2004. We collected the patients' screening dates, their resident registration number, and data regarding the seven risk factors for the Korean model (age, body mass index, menopausal status, breast feeding status, family history, previous breast tests, and age at first delivery). In addition to collecting the Korean model risk factor data, we also collected data for the for the modified Gail and Asian American Gail models, namely, the patients' age at menarche and the number of first-degree relatives they had with breast cancer. Data on the number of previous breast biopsies and the presence of atypical ductal hyperplasia in a biopsy was not available; we were only able to know whether women had previously any breast biopsy. We entered '0' for no biopsy and '1' for any biopsy. In the case of atypical ductal hyperplasia, we entered 'unknown' into the atypical ductal hyperplasia field for all biopsy cases.
If patients had been screened for breast cancer more than once, we used the data from their first visit. Cases with en error in the resident registration number or with missing variables were excluded.
Resident registration numbers were used to confirm breast cancer occurrence. With the committee's permission, the resident registration number was matched with data from the Korean Breast Cancer Registration Program. DCIS data were excluded. In cases where breast cancer occurrence was identified, the date of diagnosis was verified to be within 5 years of breast cancer screening.
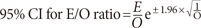
To validate the reliability of the models, we compared the observed number of breast cancers with the number expected from the models according to the risk factors and quintiles of predicted risk. Expected numbers of cases were calculated by summation of the 5-year individual absolute risk as predicted by each model, using equations (1)-(4), given the risk factors for each patient at the start of follow-up. The 95% confidence intervals (CI) of the expected-to-observed (E/O) ratio were calculated as follows:
The discriminatory power of the models was evaluated by the area under the curve (AUC) of the receiver operating characteristics (ROC) curve analysis.
After validation of the three risk models, we updated the Korean model [5]. The original Korean model used breast cancer incidence and mortality rates from Korean data, but the data from 1999 to 2001 was used. We updated the model by using more recent breast cancer incidence and mortality rates and overall mortality rate [10]. The updated Korean model calculated the breast cancer risk according to the year of the screening visit. We revalidated the updated Korean model using data from the Korean Breast Cancer Registration Program. Microsoft Excel 2007 (Microsoft Inc., Redmond, USA) and SPSS 19.0 (IBM Inc., Armonk, USA) were used for statistical analyses. The study was approved by the institutional review board of the Cheil General Hospital (CGH-IRB-2011-78) and the Dankook University Hospital (DKUH IRB 2011-11-0427).
A total of 76,727 patients were screened during the study period. After excluding patients who had visited more than once, or had data errors or missing data, 40,229 patients were included in the validation (Figure 1). Among them, 161 patients were confirmed to have developed breast cancer within 5 years of screening.
The expected and observed counts calculated according to the screening years and risk factors using the modified Gail model are shown in Table 2. Overall, 395.46 patients with cancer were expected and 161 were observed. Overall, the modified Gail model showed an overestimation and the E/O ratio was 2.46 (95% CI, 2.10-2.87). A similar over-estimation was found in the predicted 5-year risk quintiles (Supplementary Table 4).
The Asian American Gail model (Table 3, Supplementary Table 5) also showed overestimation, and the overall E/O ratio was 1.29 (95% CI, 1.11-1.51). The magnitude of overestimation by the Asian American Gail model was less than that by the modified Gail model.
Contrary to the modified Gail and Asian American Gail models, the Korean model (Table 4, Supplementary Table 6) showed an underestimation. Overall, 80.90 patients with cancer were expected and the E/O ratio was 0.50 (95% CI, 0.43-0.59). The risk factor and predicted 5-year quintiles were similar to those predicted by the other models.
Having found that the risk of breast cancer is overestimated by the Gail models and underestimated by the Korean model, we proceeded to update the Korean model to achieve a better performance. We updated the models using more recent incidence and mortality rate data.
The updated Korean model is available at http://surgery.dankook.ac.kr/brca2/. In this model, we included the screening year, and breast cancer risk was calculated according to that year. For example, the estimated 5-year breast cancer risk of a 50-year-old postmenopausal woman who is 160 cm tall, 50 kg in weight, delivered her first baby at the age of 22, breast fed her child, had no family and no previous breast tests had a risk of 0.06% in 1999 and 0.12% in 2004. Figure 2 shows the baseline hazards for breast cancer with no risk factors. The baseline hazard increases according to the year, especially for patients aged 45-49. The baseline hazard for patients aged 45-49 in 2004 are more than twofold those for patients aged 45-49 in 1999.
The expected versus observed counts calculated according to the risk factors and screening year using the updated Korean model are shown in Table 5. Overall, 137.48 patients with cancer were expected and 161 were observed. The tendency towards underestimation remained in the updated Korean model, but the performance was improved when compared with the modified Gail, Asian American Gail and original Korean models. The overall E/O ratio was 0.85 (95% CI, 0.73-1.00). In the screening years 1999 and 2004, the E/O ratio was 0.63 (95% CI, 0.45-0.87) and 0.73 (95% CI, 0.56-0.96), respectively. The E/O ratio was 0.11 (95% CI, 0.04-0.30) in patients aged 29 years or less and 0.33 (95% CI, 0.23-0.48) in patients aged 60 years or more. There was a tendency to underestimate breast cancer risk in the breast-feeding (E/O ratio, 0.67; 95% CI, 0.56-0.80), no family history (E/O ratio, 0.83; 95% CI, 0.71-0.97), and no history of biopsy, cytology, screening mammography or sonography (E/O ratio, 0.32; 95% CI, 0.22-0.48) groups.
We categorized the predicted 5-year risk into quintiles (Supplementary Table 7). In the 40-59 years age group, expected and observed counts were not different, except for those with a risk of less than 0.127. In the more than 60 years age group, there was a tendency of underestimation for patients with a risk less than 0.194, which was in the 40th percentile of the predicted 5-year risk. A similar tendency was observed in the overall age group.
The AUC after ROC analysis of the four models is summarized in Table 6. The AUC of the modified Gail model was 0.547 (95% CI, 0.500-0.594; p=0.039); the Asian-American Gail model AUC was 0.543 (95% CI, 0.495-0.590; p=0.061); the original Korean model AUC was 0.509 (95% CI, 0.463-0.556; p=0.690); and the updated Korean model AUC was 0.558 (95% CI, 0.511-0.605; p=0.011). The updated Korean model showed the best discriminatory power.
In this study, we have validated the modified Gail model (model 2), Asian American Gail model, and Korean model using a dataset of Korean breast cancer screening patients. Breast cancer occurrences were confirmed by matching the data with the Korean Breast Cancer Registration Program. The modified Gail model showed a 146% overestimation and the Asian American Gail model showed a 29% overestimation of breast cancer risk in Korean women.
The Gail model has been validated in many studies, but there are few validation studies for Asians. The modified Gail model and Asian American Gail model have been validated for the 5-year risk of breast cancer in 28,104 Singaporean women [4]. In this study, the modified Gail model showed a 151% overestimation and the Asian American Gail model showed a 43% overestimation; these results are similar to those of our. The authors of the Singaporean validation study suggested that the reason for the Gail model overestimation might be a incidence of breast cancer and reduced mammographic screening in Singapore. Interestingly, they also showed the results of a 10-year risk of breast cancer validation study. In this study, the modified Gail model showed an 85% overestimation but the Asian American Gail model showed an underestimation of just 1%. They attributed this change to an increase in breast cancer incidence and mammographic screening.
Contrary to the Gail models, the Korean model showed a 50% underestimation of breast cancer risk. The Korean model was developed using risk factors from a Korean case-control study, and Korean incidence and mortality data. At the beginning of this study, we hypothesized that the Korean model would be capable of precisely estimating the risk of breast cancer for Korean women. However, the results indicate a severe underestimation. One of the reasons for this underestimation could be a recent increase in the incidence of breast cancer. The validation study population dataset was collected between 1999 and 2004, but the Korean model was developed using data from the years 1999 and 2001. In the year 1999, the incidence of breast cancer in Korean women was 24.3 per 100,000, and increased to 37.6 per 100,000 by the year 2004 [10]; a 55% increase in 5 years. To account for this, we updated the Korean model with data of incidence and mortality for each individual year. The resulting updated Korean model showed a 15% underestimation of breast cancer risk, which was more accurate than the modified Gail, Asian American Gail and original Korean models.
In accordance with our findings, we believe that it is of the utmost importance to periodically update the incidence and mortality data in prediction models, particularly if there is a rapid rate of change in a given population. However, we have been unable to find any studies detailing such updating in countries with rapidly changing incidence and mortality statistics, such as Asia. In North America, which has a relatively stable incidence of breast cancer, updating the model data would also improve the performance, even if this updating was not periodic. A validation study of the Gail model has been performed using data from the National Institutes of Health-American Association of Retired Persons (NIH-AARP) from 1995 to 2003, and the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial (PLCO) from 1993 to 2006 [11]. Using SEER data from 1983 to 1987, the Gail model showed a 13% underestimation in NIH-AARP patients and a 14% underestimation in PLCO patients. After updating the model with SEER data from 1995 to 2003, the updated Gail model showed well-calibrated results (a 3% overestimation in the NIH-AAPR data and a 1% overestimation in the PLCO data). This study illustrates the importance of updating incidence data, even in relatively stable populations.
Despite updating the incidence and mortality data, the updated Korean model showed a 15% underestimation of breast cancer risk, although this was not statistically significant. There are a number of reasons that this underestimation might have occurred. Firstly, the validation data in this study was not a prospective cohort of the general population. We used data from breast cancer screening patients, most of whom were routinely screened. Routinely screened patients show a higher incidence rate than unscreened patients, which results in a comparatively high number of cases been observed and therefore an underestimating model. Conversely, a model developed using data from routinely screened patients will show a relatively high expected rate of incidence, and will therefore overestimate risk if applied to unscreened patients. The original Gail model, which was developed using data from the annual mammographic screening BCDDP, showed a 33% overestimation in validation using data from the Nurse's Health Study, which did not enforce regular screening [12].
A second possible reason for the updated Korean model underestimation is that in our study we confirmed the occurrence of breast cancer by retrospective matching with the Korean Breast Cancer Registration Program data, not by prospective follow-up. Given that the Korean Breast Cancer Registration Program does not include all the breast cancer cases in Korea, it is possible that the observed incidence of breast cancer in our study is inaccurate. Although the National Cancer Registration Program in Korea has more accurate cancer incidence data, we were unable to access the data because of the Personal Information Protection Act, which was introduced in 2011. To overcome this limitation, a prospective study with participant permission would need to be conducted.
The AUC of the modified Gail model was 0.547, the Asian American model AUC was 0.543, the Korean model AUC was 0.509, and the AUC of the updated Korean model was 0.558 (Table 6). The AUC has the same significance as the concordance statistic. The AUC of the modified Gail model using the data from the Nurses' Health Study was 0.58 (95% CI, 0.56-0.60) [13]. The AUC of the Asian American Gail model using the data from the Women's Health Initiative was 0.614 (95% CI, 0.587-0.640) [8]. Compared with the concordance statistic of the modified Gail model and the Asian American Gail model, the updated Korean model has a comparable discriminatory power. A prediction model with only clinical information cannot have strong discriminatory power. For a greater discriminatory power, biochemical data, such as estrogen level, radiological data, such as mammographic density, and molecular markers, such as single nucleotide polymorphisms should be included.
Assessment of breast cancer risk is important for the screening and prevention of disease. In high-risk patients, more frequent screening is required. In Western countries, mammographic screening has produced a sharp reduction in breast cancer mortality in women aged over 50 [14]. However, the position is less clear for women aged 40 to 49. For women aged 40 to 49 with a risk of developing breast cancer greater than the baseline risk of a 50-year-old, it would be reasonable to conduct screening mammography. In Korean women, screening mammography is recommended for those aged over 40. However, Korean women show denser breast tissue on mammography than Western women [15], and so sonography is frequently used for screening. As such, a risk assessment model to guide sonographic screening in Korean women would be useful.
Tamoxifen and raloxifene have been approved for breast cancer prevention in the United States. It has been confirmed that 49% of breast cancer in women assessed as having a breast cancer risk greater than 1.66% by the Gail model could be prevented. However, tamoxifen and raloxifene are not commonly used for breast cancer prevention because of potentially fatal complications, such as endometrial cancer, deep vein thrombosis, and cerebral stroke. Gail et al. [16] have proposed a risk-benefit index to assess the risks and potential benefits of tamoxifen chemoprevention. Korean women have different risks and benefits, and so a Korean breast cancer risk assessment model would be crucial in order to develop a risk-benefit index for Koreans [17].
In conclusion, we have validated the modified Gail model, the Asian American Gail model, and the Korean model using data from screening patients matched to the Korean Breast Cancer Registration Program. The updated Korean model shows a better performance than the other three previous models. It is hoped that this validation study can form the basis of a clinical risk assessment program and a future prospective study of breast cancer prevention.
Figures and Tables
Table 2
Expected and observed cancers for categories by screening years and risk factors using modified Gail model

Table 3
Expected and observed cancers for categories by screening years and risk factors using Asian American Gail model

Table 4
Expected and observed cancers for categories by screening years and risk factors using original Korean model

References
1. Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989; 81:1879–1886.

2. Fisher B, Costantino JP, Wickerham DL, Redmond CK, Kavanah M, Cronin WM, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998; 90:1371–1388.

3. Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006; 295:2727–2741.

4. Chay WY, Ong WS, Tan PH, Jie Leo NQ, Ho GH, Wong CS, et al. Validation of the Gail model for predicting individual breast cancer risk in a prospective nationwide study of 28,104 Singapore women. Breast Cancer Res. 2012; 14:R19.

5. Kim SH, Chae YS, Son WJ, Shin DJ, Kim YM, Chang MC. Estimation of individualized probabilities of developing breast cancer for Korean women. J Korean Surg Soc. 2008; 74:405–411.
6. Park SK, Yoo KY, Kang DH, Ahn SH, Noh DY, Choe KJ. The estimation of breast cancer disease-probability by difference of individual susceptibility. Cancer Res Treat. 2003; 35:35–51.

7. Ko BS, Noh WC, Kang SS, Park BW, Kang EY, Paik NS, et al. Changing patterns in the clinical characteristics of Korean breast cancer from 1996-2010 using an online nationwide breast cancer database. J Breast Cancer. 2012; 15:393–400.

8. Matsuno RK, Costantino JP, Ziegler RG, Anderson GL, Li H, Pee D, et al. Projecting individualized absolute invasive breast cancer risk in Asian and Pacific Islander American women. J Natl Cancer Inst. 2011; 103:951–961.

9. Ziegler RG, Hoover RN, Pike MC, Hildesheim A, Nomura AM, West DW, et al. Migration patterns and breast cancer risk in Asian-American women. J Natl Cancer Inst. 1993; 85:1819–1827.

10. Korea National Statistical Office. Korean Statistical Information System. 2013. Accessed November 1st, 2013. Available from: http://www.kosis.kr/.
11. Schonfeld SJ, Pee D, Greenlee RT, Hartge P, Lacey JV Jr, Park Y, et al. Effect of changing breast cancer incidence rates on the calibration of the Gail model. J Clin Oncol. 2010; 28:2411–2417.

12. Spiegelman D, Colditz GA, Hunter D, Hertzmark E. Validation of the Gail et al. model for predicting individual breast cancer risk. J Natl Cancer Inst. 1994; 86:600–607.

13. Rockhill B, Spiegelman D, Byrne C, Hunter DJ, Colditz GA. Validation of the Gail et al. model of breast cancer risk prediction and implications for chemoprevention. J Natl Cancer Inst. 2001; 93:358–366.

14. Kerlikowske K, Grady D, Rubin SM, Sandrock C, Ernster VL. Efficacy of screening mammography: a meta-analysis. JAMA. 1995; 273:149–154.

15. Kim SH, Kim MH, Oh KK. Analysis and comparison of breast density according to age on mammogram between Korean and Western women. J Korean Radiol Soc. 2000; 42:1009–1014.

Supplementary Materials
Supplementary Table 4
Expected and observed cancers for categories by age group and predicted 5-year risk using modified Gail model
Supplementary Table 5
Expected and observed cancers for categories by age group and predicted 5-year risk using Asian American Gail model




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download