Abstract
Purpose
The purpose of this study was to quantify the target coverage, homogeneity, and robustness of the dose distributions against geometrical uncertainties associated with four whole breast radiotherapy techniques.
Methods
The study was based on the planning-computed tomography-datasets of 20 patients who underwent whole breast radiotherapy. A total of four treatment plans (wedge, field-in-field [FIF], hybrid intensity-modulated radiotherapy [IMRT], and full IMRT) were created for each patient. The hybrid IMRT plans comprised two opposed tangential open beams plus two IMRT beams. Setup errors were simulated by moving the beam isocenters by 5 mm in the anterior or posterior direction.
Results
With the original plan, the wedge technique yielded a high volume receiving ≥107% of the prescription dose (V107; 7.5%±4.2%), whereas the other three techniques yielded excellent target coverage and homogeneity. A 5 mm anterior displacement caused a large and significant increase in the V107 (+5.2%±4.1%, p<0.01) with the FIF plan, but not with the hybrid IMRT (+0.4%±1.2%, p=0.11) or full IMRT (+0.7%±1.8%, p=0.10) plan. A 5-mm posterior displacement caused a large decrease in the V95 with the hybrid IMRT (-2.5%±3.7%, p<0.01) and full IMRT (-4.3%±5.1%, p<0.01) plans, but not with the FIF plan (+0.1%±0.7%, p=0.74). The decrease in V95 was significantly smaller with the hybrid IMRT plan than with the full IMRT plan (p<0.01).
The avoidance of hot spots throughout the breast volume is difficult with external whole breast radiotherapy using conventional forward wedge planning [1,2]. For this reason, intensity-modulated radiotherapy (IMRT) is gradually replacing wedge planning [3]. IMRT provides excellent dose homogeneity throughout the breast volume [4]. One disadvantage of IMRT is that the IMRT plans might be more susceptible to setup and motion uncertainties [5,6,7,8,9]. The intact breast flash is used to compensate for motion in the anteroposterior direction in glancing open fields; however, flash cannot be easily achieved when using the IMRT inverse-planning technique.
The field-in-field (FIF) technique is a forward-planning intensity-modulating technique [10,11] in which fields are created by strategically placing multileaf collimator leaves in hot spots. FIF plans can incorporate fields with the breast flash and thus might reduce the effects of geometrical uncertainties. Another possible solution to reduce the effects of geometrical uncertainties would be the use of a hybrid technique that incorporates a combination of glancing open fields and inverse-planned IMRT beams [5].
The purpose of this study was to quantify the target coverage, homogeneity, and robustness of the dose distributions against geometrical uncertainties associated with four whole breast radiotherapy techniques (wedge, FIF, hybrid IMRT, and full IMRT).
This study was approved by the Institutional Review Board (11-R190). The planning computed tomography datasets of 20 patients who underwent whole breast radiotherapy at St. Luke's International Hospital (10 with left-sided and 10 with right-sided cancer) formed the basis of this study. Computed tomography was performed without breath holding by using a LightSpeed RT 16 (GE Healthcare, Fairfield, USA) helical scanner with a 5-mm slice thickness.
A total of four treatment plans (wedge, FIF, hybrid IMRT, and full IMRT) were created for each patient by using the Pinnacle3 version 9.0 planning software package (Philips Medical, Amsterdam, The Netherlands). Adaptive convolution was the selected calculation algorithm. The clinical target volume (CTV) was defined as the ipsilateral whole breast. The planning target volume was defined as the CTV plus a surrounding 0.8- to 1.5-cm margin. The target volume for evaluation (TV_EV) was defined by subtracting the areas within 5 mm of the skin or lung from the whole breast.
All four plans used two opposed tangential 4 to 6 MV beams set at the same angles. The wedge plans comprised two opposed tangential open beams with wedges. The FIF plans comprised two opposed tangential open beams plus 2 to 4 reduction fields at the same angles. Plan optimization was performed in a forward fashion. The details of the FIF plans used in our institution have been reported previously [11]. The hybrid IMRT plans comprised two opposed tangential open beams plus two IMRT beams set at the same angles. The open beams contributed 90% of the dose, whereas the inversely optimized IMRT beams contributed 10%. For IMRT, direct-machine parameter optimization was performed to set the dose to the whole TV_EV between 95% and 107% of the prescribed dose. The full IMRT plans comprised 100% segments that had been inversely optimized. The plans were normalized such that 50% of the TV_EV received a total of 50 Gy in 2-Gy fractions for both the hybrid IMRT and full IMRT plans, whereas for the wedge and FIF plans, doses were prescribed to the beam isocenters.
Setup errors were simulated by moving the beam isocenters by 5 mm in the anterior or posterior direction.
The target coverage and homogeneity were assessed according to the volume of the TV_EV receiving ≥95% of the prescription dose (V95), V107, and the mean dose to the TV_EV. The doses to the organs at risk were assessed as the V20 of both lungs, mean dose to both lungs, V30 of the heart, and mean dose to the heart. The V30 of the heart and mean heart dose were assessed in the patients with left-sided cancer.
We additionally measured the time required to deliver 2 Gy with each technique via simulation with a phantom.
We used the SPSS version 20 package (SPSS Inc., Chicago, USA) for statistical analysis. Differences were deemed significant when the two-tailed p-values were less than 0.05.
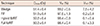
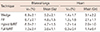
Table 1 shows the target coverage and homogeneity values achieved with the four techniques according to the original plan. The wedge technique yielded a high V107 (7.5%±4.2%) whereas the other three techniques provided excellent target coverage and homogeneity. Table 2 shows the differences in target coverage and homogeneity from the original plan in response to moving the beam isocenters by 5 mm in the anterior or posterior direction.
A 5-mm displacement in the anterior direction caused a large increase in the V107 (+5.2%±4.1%, p<0.01) with the FIF plan, whereas no significant increases were observed with the hybrid IMRT (+0.4%±1.2%, p=0.11) or full IMRT (+0.7%±1.8%, p=0.10) plan. A 5-mm displacement in the posterior direction caused a large decrease in the V95 with the hybrid IMRT (-2.5%±3.7%, p<0.01) and full IMRT (-4.3%±5.1%, p<0.01) plans, whereas no significant decrease was noted with the FIF plan (+0.1%±0.7%, p=0.74). The decrease in the V95 was significantly smaller with the hybrid IMRT plan than with the full IMRT plan (p<0.01).
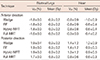
Table 3 shows the doses provided to both lungs and the heart when using the four techniques according to the original plan. Table 4 shows the differences in these values from the original plan after moving the beam isocenters by 5 mm in the anterior or posterior direction. For all four techniques, acceptable outcomes were obtained for all parameters, although a more favorable tendency was observed with the full IMRT plan.
Table 5 shows the time required to deliver 2 Gy using each technique. The FIF delivery time was the shortest, whereas the hybrid IMRT delivery time was the longest. However, the absolute differences in the delivery times were small.
Our results showed that hybrid IMRT was superior to full IMRT in terms of robustness against geometrical uncertainties, thus corroborating the findings of a previous investigation [5]. The breast flash was not implemented in the optimization routine for the inverse planning technique, leading to underdosage near the skin under posterior displacement conditions. In this sense, the full IMRT technique was suboptimal for whole breast radiotherapy.
However, hybrid IMRT offered excellent target coverage and homogeneity comparable to that of full IMRT. Theoretically, hybrid IMRT techniques should provide worse dose distributions in exchange for better robustness against geometrical uncertainties, as the contribution from the inversely optimized IMRT beams is reduced. We used an IMRT beam contribution of only 10% to achieve better robustness against geometrical uncertainties and found that this 10% contribution was sufficient to yield excellent target coverage and homogeneity for whole breast radiotherapy and to provide better robustness against geometrical uncertainties, given the high percentage of glancing open fields.
We found that the FIF technique also offered excellent target coverage and homogeneity. The disadvantage with FIF was the generation of considerable hot spots under anterior displacement conditions. The advantage of FIF was its strong robustness with posterior displacement. Given these features, we consider the FIF technique as an alternative to hybrid IMRT.
The wedge technique showed good robustness against geometrical uncertainties. However, this technique yielded a high V107, which would likely increase the risk of severe dermatitis.
Regarding the doses to the lungs and heart, we observed similar, acceptable outcomes both with the original plan and in terms of the robustness against geometrical uncertainties for all four techniques, although a more favorable tendency was observed with full IMRT.
We also evaluated the delivery time with each technique. The delivery times for all four techniques were similarly short. We therefore do not consider the delivery time to be an important factor in technique selection.
A limitation of our investigation is that only a small series of Japanese patients were evaluated. The breasts investigated in this study might be smaller than the global average. A focus on patients with larger breasts and possibly larger geometrical uncertainties might yield different findings. Another limitation is that only anterior-posterior displacement setup errors were evaluated; however, geometric uncertainties include displacement in the left-right, craniocaudal, and anteroposterior directions. Nevertheless, we believe that the outcomes of this study will offer some guidance to clinicians in a field in which data are relatively lacking.
In conclusion, the FIF, hybrid IMRT, and full IMRT plans offered excellent target coverage and homogeneity. Hybrid IMRT was superior to full IMRT in terms of robustness against geometrical uncertainties, whereas FIF provided comparable robustness to that of hybrid IMRT.
Figures and Tables
Table 2
Differences in the target coverage and homogeneity from the original plan by moving beam isocenters by 5 mm in the anterior or posterior direction

Notes
References
1. Aref A, Thornton D, Youssef E, He T, Tekyi-Mensah S, Denton L, et al. Dosimetric improvements following 3D planning of tangential breast irradiation. Int J Radiat Oncol Biol Phys. 2000; 48:1569–1574.

2. Buchholz TA, Gurgoze E, Bice WS, Prestidge BR. Dosimetric analysis of intact breast irradiation in off-axis planes. Int J Radiat Oncol Biol Phys. 1997; 39:261–267.

3. Smith BD, Pan IW, Shih YC, Smith GL, Harris JR, Punglia R, et al. Adoption of intensity-modulated radiation therapy for breast cancer in the United States. J Natl Cancer Inst. 2011; 103:798–809.

4. Harsolia A, Kestin L, Grills I, Wallace M, Jolly S, Jones C, et al. Intensity-modulated radiotherapy results in significant decrease in clinical toxicities compared with conventional wedge-based breast radiotherapy. Int J Radiat Oncol Biol Phys. 2007; 68:1375–1380.

5. van Mourik A, van Kranen S, den Hollander S, Sonke JJ, van Herk M, van Vliet-Vroegindeweij C. Effects of setup errors and shape changes on breast radiotherapy. Int J Radiat Oncol Biol Phys. 2011; 79:1557–1564.

6. Jain P, Marchant T, Green M, Watkins G, Davies J, McCarthy C, et al. Inter-fraction motion and dosimetric consequences during breast intensity-modulated radiotherapy (IMRT). Radiother Oncol. 2009; 90:93–98.

7. Fan Y, Nath R. Intensity modulation under geometrical uncertainty: a deconvolution approach to robust fluence. Phys Med Biol. 2010; 55:4029–4045.

8. Schwarz M, Van der Geer J, Van Herk M, Lebesque JV, Mijnheer BJ, Damen EM. Impact of geometrical uncertainties on 3D CRT and IMRT dose distributions for lung cancer treatment. Int J Radiat Oncol Biol Phys. 2006; 65:1260–1269.

9. Bos LJ, van der Geer J, van Herk M, Mijnheer BJ, Lebesque JV, Damen EM. The sensitivity of dose distributions for organ motion and set-up uncertainties in prostate IMRT. Radiother Oncol. 2005; 76:18–26.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download