Abstract
Purpose
The p53 gene is one of the most frequently mutated genes in breast cancer. We investigated the patterns and biologic features of p53 gene mutation and evaluated their clinical significance in Korean breast cancer patients.
Methods
Patients who underwent p53 gene sequencing were included. Mutational analysis of exon 5 to exon 9 of the p53 gene was carried out using polymerase chain reaction-denaturing high performance liquid chromatography and direct sequencing.
Results
A total of 497 patients were eligible for the present study and p53 gene mutations were detected in 71 cases (14.3%). Mutation of p53 was significantly associated with histologic grading (p<0.001), estrogen receptor and progesterone receptor status (p<0.001), HER2 status (p<0.001), Ki-67 (p=0.028), and tumor size (p=0.004). The most frequent location of p53 mutations was exon 7 and missense mutation was the most common type of mutation. Compared with patients without mutation, there was a statistically significant difference in relapse-free survival of patients with p53 gene mutation and missense mutation (p=0.020, p=0.006, respectively). Only p53 missense mutation was an independent prognostic factor for relapse-free survival in multivariate analysis, with an adjusted hazard ratio of 2.29 (95% confidence interval, 1.08-4.89, p=0.031).
Breast cancer has variable clinical, pathologic and molecular features, resulting in diversity in behavior, response to therapy, and clinical outcome [1]. Breast cancer is divided into subtypes based on hormone receptor status and Her-2-neu (HER2) analysis [2]. These characteristics are commonly used to predict breast cancer prognosis and choose appropriate treatment options [3,4].
Heterogeneity of breast cancer is also associated with different types of genetic alterations such as mutations in oncogenes and tumor suppressor genes. One of the most frequent sites of gene mutation is the p53 gene [5]. The p53 protein has been identified as a transcription factor with sequence-specific DNA-binding properties and the ability to regulate entry into the S phase of the cell cycle [6]. It plays a key role in many cellular pathways and influences the induction of apoptosis in malignant cells [7].
The p53 gene has been described as the most mutated gene in breast cancer, with approximately 30% of tumors having a p53 mutation [5]. A recent study of The Cancer Genome Atlas Network evaluated whole-exome sequencing data and identified the frequency of p53 gene mutation as 37% in breast cancer overall and as high as 80% in basal-like breast cancer [8], which is characterized by expression of genes usually found in basal epithelial cells and it is placed within a cluster of estrogen receptor negative and HER2 negative tumors being associated with poor prognosis [9,10].
The prognostic significance of p53 gene mutations has often been studied, but the impact of individual p53 gene mutations on outcomes in breast cancer remains controversial [11,12]. There are many types of p53 mutations, the most common type being missense mutation followed by frame shift, nonsense, and others [13]. According to several studies, the influence of the type of p53 mutation on survival of breast cancer patients also varies [12,14]. There are few studies on the type and clinical significance of p53 gene mutations in Korean breast cancer patients. Therefore, we used DNA sequence-based analysis to analyze the patterns and biologic features of p53 gene mutations and evaluated the clinical significance of these mutations in Korean patients with breast cancer.
This study initially included 606 patients who were surgically treated for primary invasive breast cancer and who had undergone p53 gene sequencing between December 2002 and December 2009 at Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. Patients who were treated with neoadjuvant chemotherapy and those who were diagnosed with recurrent or metachronous breast cancer were excluded from this study. Patients with ductal carcinoma in situ were also excluded. As a result, 497 patients were included in our analysis. This study was reviewed and approved by the Institutional Review Board (IRB) of Gangnam Severance Hospital (Local IRB approval number, 2011-0253).
The clinical data of each patient were reviewed and pathological findings including tumor size, tumor grade, presence of multifocal or multicentric disease, and the number of lymph node metastases were recorded. The results of estrogen receptor (ER) and progesterone receptor (PR) analysis were also recorded. Her-2-neu status was assessed and HER2 positivity was defined by a score of 3+ on immunohistochemical (IHC) staining or HER2 gene amplification in fluorescence in situ hybridization. According to criteria suggested by the St. Gallen panelists [2], we classified breast cancer into four subtypes as follows: 1) luminal A: ER positive and/or PR positive, HER2 negative, Ki-67-positive <14%; 2) luminal B: ER positive and/or PR positive, HER2 negative, Ki-67 ≥14% or HER2 positive, any Ki-67; 3) HER2: ER negative and PR negative, HER-2 positive, any Ki-67; 4) Triple negative: ER negative and PR negative, HER2 negative, any Ki-67. The pathologic T stage and lymph node (N) stage were classified according to the seventh edition of the American Joint Committee on Cancer classification system [15]. The modified Scarf-Bloom-Richardson grading system was used for tumor grading. All eligible patients were followed up for recurrence and survival. Relapse-free survival (RFS) was defined as the time between initial diagnosis and locoregional recurrence, distant metastasis, or death from any cause related to breast cancer. Breast cancer-specific survival (BCSS) was defined as the time between initial diagnosis and death from any cause related to breast cancer.
Mutational analysis for exon 5 to exon 9 of the p53 gene was carried out using polymerase chain reaction (PCR)-denaturing high performance liquid chromatography (DHPLC) and direct sequencing. About 1 mg samples from freshly frozen surgical specimens and extraction of DNA was performed using the Easy-DNATM kit (Invitrogen, Carlsbad, USA) and used as a template for PCR. Specific primers, as shown in Table 1, were used at 20 µmol. Each PCR was performed with an initial denaturation step of 5 minutes at 95℃, followed by 50 cycles of 94℃ for 10 seconds, 62℃ for 10 seconds, 72℃ for 15 seconds; and 72℃ for 5 minutes in a DNA thermal cycler (GeneAmp PCR System 2400; Perkin-Elmer, Branchburg, USA). Each PCR product was first screened for mutations by DHPLC (WAVE; Transgenomic, Omaha, USA), followed by sequence analysis if heteroduplex formation was detected [16,17]. The DHPLC device was operated according to the manufacturer's instructions. For heteroduplex formation, PCR products were denatured at 95℃ for 5 minutes and annealing was performed at 55℃ for about 40 minutes. Afterwards, these products were automatically loaded into the DNASep Cartridge (Transgenomic) column. The column was washed with buffer D (75% acetonitrile solution) at 0.9 mL/min at 60℃ for 30 minutes, and stabilized using buffer A (0.1 M triethylammonium acetate [TEAA] solution, pH 7.0) and buffer B (0.1 M TEAA with 25% acetonitrile, pH 7.0) at 0.9 mL/min for 60 minutes. The eluted DNA was detected using an ultra-violet light detector at a wavelength of 260 nm. Heteroduplexes and homoduplexes appear as separate forms in the chromatogram and the separation of these products was monitored on a computer screen. Sequencing analysis was performed using commercial reagents and an automated sequencer (ABI Prism BigDye Terminator v3.1 cycle sequencing kit and ABI 310 Genetic Analyzer; Applied Biosystems, Foster City, USA). Both forward and reverse strands were sequenced to confirm nucleotide alterations.
Univariate analysis was performed for survival analysis of types of p53 mutation and the Kaplan-Meier method was applied to estimate disease-free survival and overall survival curves. The significance of differences between the estimated survival curves was tested using log-rank statistics. All statistical analyses were performed using the SPSS program version 18.0 (SPSS Inc., Chicago, USA). A p-value less than 0.05 was considered to indicate a statistically significant difference.
Among a total of 606 patients who underwent p53 gene sequencing between December 2002 and December 2009, 497 patients were eligible for the present study. Among them, p53 gene mutations were detected in 71 cases (14.3%). The association of p53 mutation with clinical and pathological characteristics was investigated (Table 2). Mutation of p53 was significantly associated with histologic grade (p<0.001), estrogen receptor and progesterone receptor status (p<0.001), HER2 status (p<0.001), Ki-67 (p=0.028), and tumor size (p=0.004). p53 mutation was more prevalent in patients with high grade, hormone receptor negative, HER2 positive, and large tumors. Subgroup analysis showed that p53 mutation was observed more frequently in patients with HER2 or triple-negative breast cancer subtypes (32.4%) (p<0.001).
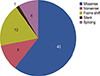
Among the 71 patients with p53 mutation, the types and locations of the mutation were investigated. As shown in Figure 1, missense mutation was the most common type of p53 mutation (43 patients, 60.6%) and frame shift mutation was the second most common (16 patients, 18.3%). Nonsense mutations were observed in 10 patients (11.3%), silent mutation in one patient (1.4%), and splicing mutation in six patients (8.5%). The most frequent location of p53 mutations was exon 7 (23 patients, 32.4%), followed by exon 5 (16 patients, 22.5%) (Figure 2). Mutations in exons 6, 8, and 9 were observed in 10 (14.1%), 10 (14.1%), and five patients (7.0%), respectively. Mutation in an intron was detected in six patients (8.5%). The codon numbers with p53 mutation are presented in Figure 2; codons 175, 213, 237, 238, 241, and 331 were hot spots for mutation in the present study. Frequently observed codons with p53 mutation and the detailed contents of various mutations were summarized in Table 3.
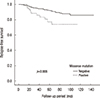
During the median follow-up period of 67 months (1-146 months), 51 patients had recurrence and 17 died from breast cancer. One patient already had distant metastasis at the time of diagnosis and she was excluded from survival analysis. In univariate analysis, we compared RFS and BCSS of the patients according to presence of p53 mutation. The 5-year RFS rates for patients with and without p53 mutation was 81.3% and 92.2%, respectively, and there was a statistically significant difference (p=0.020). The 5-year BCSS rates for patients with and without p53 mutation was 97.0% and 97.5%, respectively, and this was not statistically significant (p=0.401). We further investigated survival according to presence of p53 missense mutation. The 5-year RFS rates for patients with and without missense mutation was 77.3% and 97.0%, respectively, and there was a statistically significant difference in RFS between patients with missense mutation and those without missense mutation (p=0.006) (Figure 3). Missense mutation also showed marginal significance in BCSS (p=0.060).
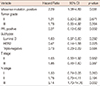
Multivariate analysis included tumor grade, PR, subtypes, T stage, N stage, p53 mutation, and missense mutation as covariates that showed marginally significant association with relapse-free survival in univariate analysis (Table 4). After adjustment for tumor grade, PR, subtypes, T stage, and N stage, presence of p53 mutation was not an independent prognostic factor of RFS (hazard ratio (HR), 1.70; 95% confidence interval (CI), 0.86-3.36; p=0.125). However, after adjustment for the same variables, p53 missense mutation was an independent prognostic factor of RFS with a relative hazard ratio of 2.29 (95% CI, 1.08-4.89; p=0.031) (Table 5).
In the present study we investigated patterns of mutation within exon 5 and exon 9 of the p53 gene in Korean patients with breast cancer. Gene sequencing revealed the presence of p53 mutation in 14.3% of patients, with missense mutations the most common type of mutation. Mutations occurred most commonly in exon 7, and codons 175, 213, 237, 238, 241, and 331 were hot spots of p53 mutation.
A number of previous studies have investigated the types and sites of mutations in the p53 gene in breast cancer. The p53 gene encodes three main protein domains: the transactivation domain, the DNA binding domain, and the oligomerization domain [18]. The DNA binding domain, encoded by exon 5 and exon 8, is the most common site of p53 gene mutation, accounting for approximately 90% of the p53 mutations reported in breast cancer [19,20]. Moreover, according to the International Agency of Research on Cancer (IARC) TP53 mutation database, the types of mutations observed indicate a high prevalence of missense mutations (http://www.irac.Fr/p53). These missense mutations are scattered throughout the coding sequence, but 97% of them cluster in exons encoding the DNA-binding domain and within this domain mutation "hotspots" have been identified at codons 175, 245, 248, 249, 273, and 282. As a result, the majority of studies have focused on mutations occurring within exon 5 and exon 8. Our results showed that the "hotspot" codons of p53 mutation in our patients were different from those in the IARC database or previous Western studies and, with the exception of codon 175, the usual hotspots were not observed. Analysis of the type of p53 mutation showed that missense mutations were the most common type of mutations in this study but the frequency of missense mutation was relatively low compared with that in the IRAC database or other studies.
We found that p53 mutation was more prevalent in high-grade, large, hormone receptor-negative, HER2-positive tumors. These results were similar to those of previous studies [12,20]. Olivier et al. [12] reported that, in addition to tumor grade and hormone receptor status, p53 mutation was more frequent in large tumors and node-negative tumors. Considering the division of breast tumors according to the subtype classification, previous studies showed that p53 mutations were more frequently found in patients with triple-negative or HER2-positive breast cancer subtypes [8,21,22]. The study of Curtis et al. [22] involving a detailed, genome-scale analysis of nearly 2,000 breast cancer cases reported that p53 mutations were found in 34% of basal-like, 22% of HER2, 13% of luminal B, and 5% of luminal A molecular subtypes. The Cancer Genome Atlas Network [8] reported rates of p53 mutation of up to 80% in the basal-like subtype, 72% in the HER2 subtype, 29% in the luminal B subtype, and 12% in the luminal A subtype. Although mutation rates were quite different from those reported in these studies, the present study also showed that p53 mutation was detected most frequently in tumors with triple-negative or HER2 subtypes. The discrepancies in the incidence and location of p53 mutations between previous studies and the present study may be due to ethnic differences in the study populations and/or heterogeneous samples and analytical methods (e.g., whole-exome sequencing). Further investigations are needed to explain these discrepancies.
There are several studies on the prognostic value of p53 mutation types. Børresen-Dale [5] suggested that the presence of mutations in the DNA binding domain of p53 is associated with aggressive tumors and poor prognosis. Végran et al. [14] also suggested that only missense mutations occurring in the DNA binding domain were significantly associated with worse disease-free survival and overall survival. Alsner et al. [23] showed that patients with missense mutations affecting the DNA binding or zinc binding domains displayed a very aggressive phenotype with short survival. These findings are supported by our data showing that missense mutation of the p53 gene is an independent prognostic factor and is associated with poor clinical outcome, although overall p53 mutation was not an independent prognostic factor. Olivier et al. [12] also showed that missense mutations, especially in the DNA-binding domain encoded by exon 5 and exon 8, and specific missense mutations (i.e., codon 179 and R248W) are associated with worse prognosis. However, they found that nonmissense mutations in DNA-binding domains had a similar poor prognostic value. Moreover, additional analysis of the whole coding sequence in 651 cases revealed that mutations located outside exon 5 and exon 8 were detected in 4% of patients and were associated with worse prognosis compared with wild type. Thus, they recommended conducting mutation analysis on all coding exons and splicing junctions. The present study did not investigate all coding exons (2 to 11) and could not assess the prognostic significance of p53 mutations occurring outside of the DNA-binding domain. A whole exon sequencing study with a large population seems to be warranted.
In summary, the present study analyzed the patterns and biologic features of p53 mutation types and evaluated the clinical significance of these mutations in Korean patients with breast cancer. Our data showed that exon 7 was the most frequent site of p53 mutation, and missense mutation was the most common type of mutation. Mutation of p53 was more prevalent in high-grade, large, triple-negative tumors, and HER2-positive tumors. Missense p53 mutation was an independent predictive factor associated with poor prognosis. We need additional studies with a large number of patients for clinical implication of results and for explanation of the observed differences in "hotspot" codons and the incidence of p53 gene mutation between this and other studies.
Figures and Tables
References
1. Rakha EA, El-Sayed ME, Green AR, Lee AH, Robertson JF, Ellis IO. Prognostic markers in triple-negative breast cancer. Cancer. 2007; 109:25–32.

2. Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ, et al. Strategies for subtypes: dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011; 22:1736–1747.

3. Kaplan HG, Malmgren JA. Impact of triple negative phenotype on breast cancer prognosis. Breast J. 2008; 14:456–463.

4. Grann VR, Troxel AB, Zojwalla NJ, Jacobson JS, Hershman D, Neugut AI. Hormone receptor status and survival in a population-based cohort of patients with breast carcinoma. Cancer. 2005; 103:2241–2251.

5. Børresen-Dale AL. TP53 and breast cancer. Hum Mutat. 2003; 21:292–300.
7. Yonish-Rouach E, Resnitzky D, Lotem J, Sachs L, Kimchi A, Oren M. Wild-type p53 induces apoptosis of myeloid leukaemic cells that is inhibited by interleukin-6. Nature. 1991; 352:345–347.

8. Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature. 2012; 490:61–70.
9. Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000; 406:747–752.

10. Sotiriou C, Neo SY, McShane LM, Korn EL, Long PM, Jazaeri A, et al. Breast cancer classification and prognosis based on gene expression profiles from a population-based study. Proc Natl Acad Sci U S A. 2003; 100:10393–10398.

11. Berns EM, van Staveren IL, Look MP, Smid M, Klijn JG, Foekens JA. Mutations in residues of TP53 that directly contact DNA predict poor outcome in human primary breast cancer. Br J Cancer. 1998; 77:1130–1136.

12. Olivier M, Langerød A, Carrieri P, Bergh J, Klaar S, Eyfjord J, et al. The clinical value of somatic TP53 gene mutations in 1,794 patients with breast cancer. Clin Cancer Res. 2006; 12:1157–1167.

13. Pharoah PD, Day NE, Caldas C. Somatic mutations in the p53 gene and prognosis in breast cancer: a meta-analysis. Br J Cancer. 1999; 80:1968–1973.

14. Végran F, Rebucci M, Chevrier S, Cadouot M, Boidot R, Lizard-Nacol S. Only missense mutations affecting the DNA binding domain of p53 influence outcomes in patients with breast carcinoma. PLoS One. 2013; 8:e55103.

15. Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual. 7th ed. New York: Springer;2010.
16. Xiao W, Oefner PJ. Denaturing high-performance liquid chromatography: a review. Hum Mutat. 2001; 17:439–474.

17. Keller G, Hartmann A, Mueller J, Höfler H. Denaturing high pressure liquid chromatography (DHPLC) for the analysis of somatic p53 mutations. Lab Invest. 2001; 81:1735–1737.

18. Levrero M, De Laurenzi V, Costanzo A, Gong J, Wang JY, Melino G. The p53/p63/p73 family of transcription factors: overlapping and distinct functions. J Cell Sci. 2000; 113(Pt 10):1661–1670.

19. Olivier M, Hainaut P. TP53 mutation patterns in breast cancers: searching for clues of environmental carcinogenesis. Semin Cancer Biol. 2001; 11:353–360.

20. Berns EM, Foekens JA, Vossen R, Look MP, Devilee P, Henzen-Logmans SC, et al. Complete sequencing of TP53 predicts poor response to systemic therapy of advanced breast cancer. Cancer Res. 2000; 60:2155–2162.
21. Bull SB, Ozcelik H, Pinnaduwage D, Blackstein ME, Sutherland DA, Pritchard KI, et al. The combination of p53 mutation and neu/erbB-2 amplification is associated with poor survival in node-negative breast cancer. J Clin Oncol. 2004; 22:86–96.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download